IgG4相关性疾病影像诊断现状与进展
刘立恒,王振常,杨正汉,李文武,靳二虎*
IgG4相关性疾病影像诊断现状与进展
刘立恒1,2,王振常1,杨正汉1,李文武2,靳二虎1*

IgG4相关性疾病是一种几乎可累及人体所有器官的慢性炎症性疾病,但大多数患者对糖皮质激素治疗有效,预后较好。由于对该病认识不足,临床上将其误诊为恶性肿瘤或感染性病变的情况时有发生,这不仅延误治疗,更给患者带来沉重的身心负担。为了进一步了解并加深对该病的认识,作者介绍了IgG4相关性疾病的临床及影像表现,回顾了近期国内外的研究进展。
IgG4相关性疾病;磁共振成像;体层摄影术,X线计算机;诊断
1Department of Radiology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China
2Department of Radiology, Shandong Cancer Hospital affiliated to Shandong University, Shandong Academy of Medical Sciences, Jinan 250117, China
ACKNOWLEDGMENTS This article was supported by the Health Industry Special Scientific Research Project (No. 201402019).
国家卫生计生委卫生公益性行业科研专项项目(201402019)
接受日期:2016-04-30
刘立恒, 王振常, 杨正汉, 等. IgG4相关性疾病影像诊断现状与进展. 磁共振成像, 2016, 7(7): 527-534.
IgG 4相关性疾病(IgG 4-related disease,IgG4-RD)是一种由免疫介导的系统性慢性炎症性疾病,其病理组织学特征是受累器官肿大、纤维化、IgG4+浆细胞浸润和闭塞性静脉炎,常伴有血清IgG4水平升高(≥135 mg/d l)[1]。目前认为IgG 4-RD几乎可累及人体所有器官,常见的受累器官或病变部位有胰腺、涎腺、泪腺、胆道、肾脏、肝脏、肺脏、眶周组织、腹膜后间隙、乳腺、血管、胃肠道及淋巴结[2-4]。临床上患者可以单个器官肿大或多个器官同时受累起病。
IgG4-RD本世纪初才被发现和命名[5]。由于临床上对该病认识不足,加之IgG4-RD的临床及影像表现多样化,使其被误诊为恶性肿瘤及感染性病变的情况时有发生,导致有些患者不能得到及时有效的治疗,甚至接受不必要的手术[6]。实际上IgG4-RD对糖皮质激素治疗敏感,如能在病变早期正确诊断、及时治疗,通常可获得较好的预后,这对患者而言意义重大[1]。建立IgG 4-RD的诊断往往需要对临床表现、组织病理学改变、影像学特征及实验室检查结果进行综合分析。影像学检查是IgG4-RD诊断环节中的重要组成部分,同时还可了解病变的累及范围、评估激素治疗的效果[7-8]。笔者以IgG 4-RD常见的受累器官或病变部位为线索,重点介绍其临床病理特征和病变的影像表现,以期使读者能够加深对该病的认识,提高诊断准确性。
1 IgG4相关性胰腺炎
胰腺是IgG4-RD最常见的受累器官之一[9],实际上当初IgG4-RD也正是因其导致的各种胰腺病变而逐步被人们所认识[5]。目前将自身免疫性胰腺炎(autoimmune pancreatitis,AIP)分为两型。其中1型AIP最常见,属于IgG4-RD[9],多见于50~70岁的男性,具有如下典型的临床病理特征:血清IgG4升高,组织学上可见丰富的IgG4+浆细胞(IgG4+浆细胞>10个/高倍镜视野)和淋巴细胞浸润,特征性的席纹状、漩涡状纤维化,闭塞性小静脉炎(图1),常伴有硬化性胆管炎、腹膜后纤维化等胰腺外病变,胰腺内、外病变均对糖皮质激素治疗敏感[10]。2型AIP,即特发性导管中心性胰腺炎,较少见,病理以胰腺组织粒细胞上皮损伤为主要特征,患者发病年龄较轻,一般不伴有血清IgG4升高,胰腺外病变少见,但常伴有溃疡性结肠炎[10]。
梗阻性黄疸是AIP患者最常见的症状,出现率约75%[11],患者常伴有间断发作的上腹部不适及消化不良。另一方面,A IP的临床症状无特异性,出现腹痛和胰酶升高时,容易与急性胰腺炎混淆,而黄疸伴有局部的胰腺病灶时易误诊为胰腺癌。
AIP的影像表现有一定特点[12],大致可分为弥漫型、局灶型、多灶型三种模式(图2)。其中弥漫型最常见,表现为胰腺弥漫性肿大,T1W I信号及CT值普遍性降低,胰腺边缘正常的分叶状结构及内部的细微结构消失,外观呈腊肠状,胰腺周围的脂肪边界清晰,增强扫描动脉期病变轻微强化,后期强化逐渐明显,呈渐进性强化模式(反映纤维化病变特征)。增强图像上包绕于胰腺边缘的胶囊状低密度环是AIP的典型征象之一,约见40%的患者[13-15]。局灶型AIP多发生于胰头,表现为局灶性CT低密度或T1W I低信号病灶,胰腺节段性肿大,病灶上游的胰管轻度扩张,此型易与胰腺癌混淆。与胰腺癌鉴别诊断要点如下:局灶型AIP的上游胰管扩张程度一般较轻(<5 mm),胰管走行于病灶内(胰管贯穿征),DW I上胰腺病灶信号更高及表观弥散系数值(apparent diffusion coefficient,ADC)更低[16],增强后多为延迟强化,胰周脂肪结构清晰,无血管受累,出现胶囊征。多灶型AIP相对少见,往往是AIP治疗过程中的阶段性表现。
2 IgG4相关性硬化性胆管炎
胆管是IgG4-RD除胰腺外另一常见的受累器官,约占文献报道病例的20%[11]。IgG4相关性硬化性胆管炎(IgG4-related sclerosing cholangitis,IgG4-SC)是一种特殊类型的硬化性胆管炎症,病理以胆管壁内大量IgG4+浆细胞浸润及广泛纤维化为特征。IgG4-SC常与自身免疫性胰腺炎、自身免疫性肝炎、IgG4相关性涎腺炎等伴发[2],但也可单独发生。
IgG4-SC多见于中老年男性。梗阻性黄疸及上腹部不适是其主要症状。与其他的IgG4-RD受累器官相似,IgG4-SC的特征性病理改变包括胆管壁全层大量IgG4+浆细胞和淋巴细胞浸润、广泛席纹状纤维化、闭塞性静脉炎等[17]。血液学检查一般有血清IgG4水平升高。
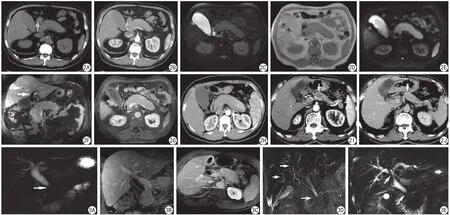
图2 男,70岁,IgG4相关性自身免疫性胰腺炎。A、B:横断面平扫CT显示胰腺弥漫性肿大,呈稍低密度,胰腺内部细微结构及边缘羽毛状结构消失,胰管不可见,增强扫描动脉期胰腺轻度强化;C:横断面T2W I显示胰腺肿胀、信号升高;D:横断面T1W I上胰腺信号降低。E:DW I (b=800 s/mm2)显示胰腺组织弥散受限,呈高信号;F、G:增强扫描平衡期T1W I胰腺呈中等程度强化,白箭所示为肝内外胆管扩张并胆管壁增厚及异常强化;H:另一患者,增强扫描动脉期CT显示包绕于胰腺边缘的特征性低密度环(白箭);I、J:另一患者,局灶型AIP,横断面增强扫描动脉期和延迟期CT显示胰腺体部局限性肿大及渐进性强化(白箭) 图3 A~C为同一患者,男性,55岁, IgG4相关性硬化性胆管炎。A:MRCP显示胆总管胰腺段狭窄(白箭),上游胆管扩张,为1型狭窄;B、C:增强T1W I显示狭窄段及扩张段胆管壁均出现增厚及异常强化,胆囊壁弥漫性增厚;D:另一患者,MRCP显示肝内胆管多发的狭窄和肝外胆管胰腺段狭窄(白箭),为2型狭窄;E:另一患者,MRCP显示肝门区胆管和胆总管胰腺段狭窄(白箭),为3型狭窄Fig. 2 IgG4-related autoimmune pancreatitis in a 70-year-old man. A, B: Abdom inal CT images show enlargement of the pancreas w ith hypo-attenuation on unenhanced and arterial phase. C—E: The enlarged pancreas shows hyperintense on T2-weighted image, m ild hypointense on T1-weighted image and hyperintense on DW I (b=800 s/mm2). F, G: On gadolinium-enhanced T1-weighted image, the pancreas shows a moderate enhancement, the bile duct dilatation and lum inal wall thickening is seen as well (white arrow). H: Another patient, arterial phase CT image shows a hypo-attenuation rim encircling the margin of the pancreas (white arrow). I, J: Another patient, the body of the pancreas exhibits focally enlarged (white arrow). The lesion shows hypoattenuation on arterial phase, and it is difficult to be differentiated from a pancreatic cancer. Fig. 3 IgG4-related sclerosing cholangitis in a 55-year-old man (A—C). A: MRCP shows the stenosis at the pancreatic segment of the common bile duct (white arrow, type 1). B, C: Gadolinium-enhanced T1-weighted image shows the thickening and enhancing of the walls of the bile ducts and gall bladder. D: The stenosis is diffusely distributed in the intra- and extrahepatic bile ducts (white arrow, type 2). E: The stenosis is seen both in the hilar bile duct and pancreatic segment of the common bile duct (white arrow, type 3).
由于胆管壁的特殊结构和形态,实际内镜操作中较难获取足够的组织样本,故IgG4-SC的病理诊断有一定局限性,使得影像学检查在IgG4-SC的诊断中具有重要意义。内镜逆行胰胆管造影(endoscopic retrograde cholangiopancreatography,ERCP)能够准确显示胆管狭窄范围、程度,CT、MRI等非侵入性检查可以全面评价胆管壁增厚、管腔扩张、肝脏、胰腺及其他器官有无病变。IgG4-SC多累及胆总管胰腺段,但肝内外胆管均可受累。受累胆管壁可表现为均匀的环状增厚,胆管壁增厚同时累及狭窄段与非狭窄段是该病特征。ERCP及MRCP可发现肝内外胆管弥漫性或节段性狭窄,狭窄段上游胆管扩张。胆管狭窄段较长(连续狭窄大于10 mm)伴上游胆管扩张是IgG4-SC的另一特征[18]。有学者将IgG4-SC依胆管狭窄分布模式分为四型[18]:1型,仅有肝外胆管胰腺段(局限性)狭窄,最常见;2型,肝内胆管和(或)肝外胆管弥漫性狭窄;3型,肝门区胆管和肝外胆管胰腺段狭窄;4型,仅有肝门区胆管狭窄(图3)。
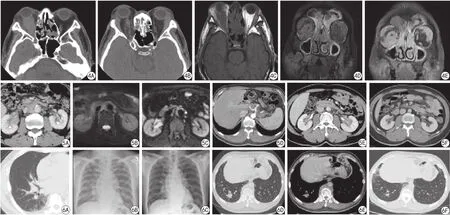
图4 男,49岁,IgG4相关性头颈部病变患者。A、B:横断面平扫CT见双侧泪腺弥漫性肿大,右眼眶肌锥内软组织肿块影包绕视神经;C:横断面平扫T1W I显示右眼眶肌锥内软组织病变呈稍低信号,眼球后脂肪组织高信号消失;D、E:冠状面早期增强T1W I显示双侧泪腺及右眼眶肌锥内软组织病变轻度异常强化,晚期增强T1W I显示病变明显强化,同时见双侧的鼻窦黏膜增厚及异常强化 图5 A~C为同一患者,男,68岁,IgG4相关性腹膜后纤维化,同时伴有胰腺病变。A:增强CT静脉期可见腹主动脉旁及右侧肾门区软组织密度病变中等程度异常强化;B:T2W I上病变呈稍高信号,边界模糊;C:DW I (b=800 s/mm2)显示病变组织弥散受限,呈高信号。D~F:另一患者,男,55岁。D:增强CT动脉期显示软组织密度病变包绕腹腔干及其分支血管,呈轻度异常强化;E:增强CT延迟期显示双侧肾门及肾盂旁软组织密度病变明显异常强化;F:该患者6年前腹部CT检查,腹膜后未见病变 图6 A~C与图5 A为同一患者,IgG4相关性肺部疾病。A:CT可见右肺下叶斑片状磨玻璃密度影及支气管血管束增粗(间质病变模式);B:1个月后复查,期间由于病因不明未行治疗,胸片显示右肺透光度减低及散在结节、索条影;C:激素治疗2个月后复查,右肺病变基本消散。D~F与图4 为同一患者。D、E:CT显示右肺下叶高密度结节灶,边界清晰(实性结节模式),胸椎两侧的肺组织也可见多发的软组织密度小灶;F:激素治疗3周后复查,右肺结节大部消散Fig. 4 IgG4-related head and neck diseases in a 49-year-old man. A, B: Axial CT images show diffuse enlargement of the bilateral lacrimal glands and a soft tissue mass in the muscle funnel of the right orbit. C: The lesion in the right muscle funnel appears as hypointense on T1-weighted image. D, E: The bilateral intraorbital lesions show progressive enhancement on coronal early and late gadolinium-enhanced T1-weighted images. Fig. 5 IgG4-related retroperitoneal fibrosis in a 68-year-old man (A—C). A: Venous phase CT image shows soft tissue lesions w ith m ild enhancement around the abdom inal aorta and the right renal hilum. B, C: The lesions appear as m ild hyperintense on T2-weighted image and hyperintense on diffusion-weighted image. D—F: Another patient. Arterial phase (D) and delayed phase (E) contrast-enhanced CT images show soft tissue thickening surrounding the celiac axis and bilateral renal hilus. No retroperitoneal lesion was found on contrast-enhanced CT image (F) obtained 6 years ago in the same patient. Fig. 6 A—C is IgG4-related pulmonary disease in the same patient of Fig.5A. A: Axial CT image shows ground-glass opacity at the right lower lung and m ild thickening of the bronchovascular bundles. B: Chest radiography obtained 1 month later w ithout any treatment shows linear opacities and tiny nodules at the right lung. C: Chest radiography obtained 2 months later follow ing glucocorticoids therapy, the lesions in the right lung disappear nearly. D, E is another IgG4-related pulmonary disease in the same patient of Fig.4. D, E: Axial CT images show a soft tissue nodule at the right lower lung. F: CT image obtained 3 weeks later follow ing glucocorticoids therapy, the nodule at the right lower lobe disappears mostly.
IgG 4-SC的影像表现与原发性硬化性胆管炎(primary sclerosing cholangitis,PSC)、胰腺癌及胆管癌有诸多重叠,临床上对于这些疾病的处理方式完全不同,因此鉴别诊断非常重要。在上述IgG4-SC分型中,2型胆管狭窄应与PSC鉴别,1和3型胆管狭窄需要与胰腺癌鉴别。不同于IgG4-SC的胆管狭窄,PSC的典型狭窄通常为多发的窄带状,并与其间的管腔扩张形成串珠状改变,胆管分支往往减少,同时伴有炎性肠病更提示PSC。胰腺癌多伴有明显的胰管梗阻及上游胰管扩张,而IgG4-SC的胰管往往不连续显示,不形成狭窄段上游胰管的全程梗阻性扩张。需要注意的是,临床实际工作中单独依靠胆管影像表现诊断IgG4-SC并不可靠,建议根据多器官受累表现、血清IgG4检查结果及组织学改变进行综合分析。
3 IgG4相关性头颈部病变
头颈部器官是除胰胆管系统外另一处易被IgG4-RD累及的区域,其中以颌下腺、腮腺、甲状腺和眼眶受累较常见[11]。近年来,随着对疾病认识与观点的更新,M ikulicz病、Küttner瘤、眼眶炎性假瘤、里德尔氏甲状腺炎、部分桥本氏甲状腺炎及垂体炎等异常均被纳入IgG4-RD的范畴[19-20]。
头颈部IgG4-RD具有一些与其他部位IgG4-RD不同的临床特征,比如,头颈部IgG4-RD患者男女比例相当,甚至部分器官病变多见于女性,同时患病年龄趋于年轻化[21]。患者常缓慢出现涎腺、甲状腺对称性、无痛性肿大,质硬,常伴有相应的涎腺分泌障碍、嗅觉障碍、甲状腺功能减低等症状;病程较长,可达数年或数十年,少数病例具有自限性。下颌下腺病变通常具有IgG4-RD典型的组织学改变,如大量淋巴浆细胞浸润、席纹状纤维化及闭塞性静脉炎。但在眼眶内及腮腺病变中,席纹状纤维化及闭塞性静脉炎出现率极低[22],该区域病变更多表现为淋巴滤泡增生,在泪腺病变常发生胶原性纤维化。这些非典型的病理组织学改变对头颈部IgG4-RD的诊断造成一定困难,但病变组织中丰富的IgG4+浆细胞(>10个/高倍视野,比例>40%)及伴发的多器官、多部位病变能够提示诊断。
头颈部IgG4-RD的基本影像表现是腺体、垂体等器官弥漫性肿大,但大致保持原有形态,边界清晰,CT图像上密度均匀减低(腮腺病变呈软组织密度)。由于细胞密度增加和纤维化,病变在T2W I呈相对低信号,同时ADC值减低,增强扫描呈均匀强化,有渐进性强化趋势。Küttner瘤常累及双侧或单侧下颌下腺,偶尔累及泪腺[23],表现为受累腺体弥漫性肿大,如单侧发病需要与肿瘤性病变鉴别。M ikulicz病通常表现为下颌下腺、腮腺、泪腺及舌下腺对称性肿大,由于临床症状及累及器官与Sjögren综合征有相似之处,临床工作中容易混淆,但后者对激素治疗不敏感,因此鉴别诊断非常必要。Sjögren综合征一般不伴血清IgG4升高,必要时需结合组织学改变进行鉴别。里德尔氏甲状腺炎及IgG4阳性桥本甲状腺炎表现为弥漫性或结节性甲状腺肿大,病变区CT值、T1W I、T2W I信号及强化程度均低于正常甲状腺,CT密度或MR信号强度均匀,需要与良恶性甲状腺肿瘤鉴别。眼眶内IgG4-RD常表现为双侧泪腺肿大及神经束增粗(图4)。
4 IgG4相关性腹膜后纤维化
腹膜后纤维化是一种发生于腹膜后间隙的慢性炎性纤维化病变,可能的致病因素包括肿瘤、放射治疗、感染、药物及外伤。然而,约70%的腹膜后纤维化病因不明,称为特发性腹膜后纤维化[24]。随着近年来IgG4-RD概念的提出,原来所谓的“特发性”腹膜后纤维化被重新认识。最新研究发现约2/3病例的病理组织学改变独特,并且对激素治疗敏感,被认为属于IgG4-RD[25]。
IgG4相关性腹膜后纤维化主要发生于老年男性,多伴有其他部位的病变[26]。患者常有定位模糊的腰背痛、体重减轻,或因病变包埋输尿管、血管而导致的肾功能异常、下肢水肿等。IgG4相关性腹膜后纤维化具有典型的病理学特征,一般伴有血清IgG4升高。由于在腹膜后区穿刺活检有一定难度和风险,加之腹膜后纤维化病变分布不均,细针穿刺标本常难以获取闭塞性静脉炎等特征性病理改变,因此需结合临床及影像表现综合分析。主要的影像表现为腹膜后软组织密度影包绕腹主动脉,常同时包绕下腔静脉和双侧输尿管,甚至延伸至肾周间隙及肾门内(图5);病变在平扫CT为等或低密度,与肌肉密度相近,在MRI表现为长T1、长T2信号;常伴有因输尿管狭窄导致的肾积水和胰腺、胆管等器官病变[27]。有学者将IgG4相关性腹膜后纤维化的影像表现分为三型[20]:(1)主动脉周围型,病变累及主动脉及其第一级分支周围的结缔组织;(2)输尿管周围型;(3)斑块型,在腹膜后区出现明显的斑块状病变。鉴别诊断包括腹膜后淋巴瘤、淋巴结转移瘤等异常。
5 IgG4相关性肺疾病
IgG4-RD肺部受累常与肺外病变共存(可同时发生或先后出现),少数患者可单独肺部发病[28]。临床上对此了解较少,往往难以做出正确诊断。患者大多为中老年男性,常见症状为干咳、气短、喘憋,病程较长,伴有基础疾病患者的病情可进展迅速。病理检查见淋巴细胞和IgG4+浆细胞弥漫性浸润肺间质,即支气管血管束、小叶间隔、小叶内间质及胸膜区;纤维化病变和闭塞性静脉炎则多见于实性肺结节和胸膜结节[29]。如果支气管镜活检未能获取满意结果,可考虑CT引导下肺组织穿刺活检,一般能够获取足够的组织样本。

图7 男,55岁,IgG4相关性肝脏疾病。A:横断面同相位T1W I显示肝实质内多发低信号结节;B:同层面反相位T1W I上病变信号无明显减低;C:横断面T2W I上病变呈不均质高信号;D:DW I上病变呈稍高信号;E:钆对比剂增强T1W I门静脉期显示肝结节病变明显强化 图8 男,70岁,IgG4相关性肾小管间质性肾炎。A:横断面平扫CT双肾实质未见异常密度灶;B:增强扫描动脉期见双肾皮质局部强化不均匀,未见明确病灶;C:增强扫描静脉期见双肾皮质区多发稍低密度结节;D:横断面T2W I上病变呈稍低信号;E:横断面T1W I上病灶为等信号,显示不清;F:横断面DW I显示双肾皮质区多发高信号病灶;G、H:增强T1W I平衡期及延迟期显示灶性病变强化程度低于正常肾实质,呈低信号 图9 男,49岁,IgG4相关性前列腺炎,膀胱导尿状态。A:横断面T2W I显示前列腺中央腺体弥漫性肿大,呈稍高信号,外周带受压变薄;B:横断面T1W I上肿大的前列腺呈均匀稍低信号;C:DW I上病变区呈大片高信号;D~F:FSPGR序列动态增强扫描T1W I显示病变渐进性强化Fig. 7 IgG4-related hepatic disease in a 55-year-old man. A: Axial in-phase T1-weighted image shows multiple lesions w ith round hypointense in the liver. B: Axial out-phase T1-weighted image shows no signal-decrease in the lesions. C, D: The nodular lesions appear as heterogeneous hyperintense on axial T2-weighted image and mild hyperintense on diffusion-weighted image. E: The nodular lesions obviously enhance at the portal venous phase of gadoliniumenhanced T1-weighted image. Fig. 8 IgG4 related-tubulointerstitial nephritis in a 70-year-old man. A: Axial CT image shows normal bilateral kidneys. B: Contrast-enhanced cortical phase CT image shows m ild abnormal enhancement in the cortex of the bilateral kidneys, but no obvious lesion. C: Venous phase CT image shows m ild hypo-attenuation focal lesions in the bilateral renal cortex. D: The lesions appear as m ild hypointense on T2-weighted image. E: On T1-weighted image, the lesions appear as isointense and could not be identified. F: Diffusion-weighted image shows multiple cortical lesions w ith diffusion restriction. G, H: The lesions appear as focal hypointense on equilibrium phase and delayed phase of gadolinium-enhanced T1-weighted images. Fig. 9 IgG4-related prostatitis in a 49-year-old man. Urethral catheterication existed. A: Axial T2-weighted image shows enlarged, mild hyperintense central gland and compressed peripheral zone of the prostate. B: The diseased prostate appears as m ild hypointense on T1-weighted image. C:Diffusion-weighted image shows the lesion w ith obvious hyperintense. D—F: The lesion shows progressive enhancement on dynam ic contrast-enhanced T1-weighted images.
IgG4-RD肺部受累的影像表现大致有两种模式[30-32]:(1)肺间质病变模式,最多见,CT特征包括弥漫性磨玻璃密度影,支气管血管束增粗,小叶间隔及小叶内间质增厚,还可见蜂窝征和支气管扩张;(2)其他模式,包括肺内局灶性磨玻璃密度结节、实性结节或肿块、胸膜结节等(图6)。患者可伴有纵隔及肺门淋巴结肿大。本病影像表现不具特异性,鉴别诊断包括肺结节病、Castleman病、淋巴瘤样肉芽肿等疾病。部分疾病甚至在病理组织学上与IgG4-RD亦有相似之处,并对激素治疗反应良好,需注意全面观察、综合分析[32]。
6 其他器官受累的IgG4相关性疾病
肝脏受累在IgG 4-RD患者中较常见,多表现为与A IP或IgG 4-SC共存的继发性肝功能损害或器质性病变。此外,有些自身免疫性肝炎(autoimmune hepatitis,AIH)的肝组织IgG4染色阳性,并且对激素治疗反应良好,故被认为可能与IgG4相关[2]。但其临床表现有别于其他器官的IgG4-RD,如AIH多为单独发病,与IgG4-A IP、IgG4-SC等疾病共存少见;组织学上浆细胞浸润散在分布,而不是典型的“丰富型”浸润;血清IgG4水平正常或仅轻微升高。因此,目前对于IgG4阳性AIH是否属于IgG4-RD尚无定论[33-34]。
IgG4相关性肝脏疾病影像学上有两种表现形式:弥散型与炎性假瘤型(图7)。炎性假瘤型病变在平扫CT呈稍低密度结节,增强扫描门静脉期结节大部分区域的强化程度高于肝实质,中心为斑片状低密度,病变外周可见环形低密度。表现不典型者易误诊为恶性肿瘤。炎性假瘤型病变一般对抗生素和激素治疗敏感。如治疗两周后病变无缩小或有增大趋势,可考虑穿刺活检或手术切除,以除外恶性病变[34]。
肾脏受累患者一般表现为急性或进展性肾功能减低。根据肾组织受累部位不同,分为IgG4相关性肾小管间质性肾炎和IgG4相关性肾盂炎,以前者多见。多为双肾受累,也可单侧受累。影像表现为肾皮质区多发的类圆形、楔形结节状病变,或肾实质及肾盂内软组织肿块。病变在平扫CT呈稍低密度,增强后病变强化程度不及邻近的肾实质,T1W I多呈等信号,T2W I呈稍低信号,DW I呈高信号[35-36],动态增强T1W I渐进性强化,边缘清晰。需要与肾癌及淋巴瘤鉴别(图8)。
淋巴结受累在IgG 4-RD的疾病谱中并不少见,一般与其他器官的IgG4-RD病变共存,临床上偶尔淋巴结单独发病。组织学上表现为淋巴结内大量IgG4+浆细胞浸润。影像表现无特异性,可有轻度至中度淋巴结肿大,密度均匀,少见坏死,多发生于纵隔、肺门、腹部及颈部。
前列腺受累在IgG4-RD的疾病谱中少见,表现为前列腺肿大及排尿困难,部分患者出现前列腺抗原水平(PSA)升高。影像检查见前列腺中央腺体弥漫性肿大,DW I呈明显高信号,增强后病变不均匀强化[37](图9)。该病需要与前列腺癌鉴别,但较为困难。因为两者在DW I均可呈显著高信号,均可有占位效应。考虑到两者的组织病理学改变不同,他们的血流动力学改变也会有差别。定量MRI参数可以反映局部组织的微循环及血流动力学信息[38],因而可能有助于区分IgG4相关性前列腺炎与前列腺癌,尚无这方面的研究报道。
此外,与IgG4-RD有关的胃肠道、肠系膜、皮肤、子宫等器官受累偶有报道[39-40],患者出现相应的临床症状。这些受累器官的组织病理学改变大致相近,主要的影像表现是多个或单一器官肿大。具体的CT、MRI表现与病变区弥漫性纤维化和高细胞密度有关。
7 小结
IgG4-RD既可以多个器官同时受累发病,也可以单一器官孤立受累发病。影像检查能够全面观察受累器官内病变数目、大小、形态及强化模式,在诊断、鉴别诊断、评估激素疗效和长期随访中起重要作用。对于AIP,通过识别弥漫性胰腺肿大及胶囊征等影像特征,做出正确诊断相对容易。而对于其他器官的IgG4-RD,由于影像特征缺乏或是对其认识不足,仅凭借CT或MRI表现做出正确诊断尚有难度。临床上患者多器官受累、多部位病变对于诊断IgG4-RD有一定提示意义。大多数情况下,明确诊断需要对临床症状、影像表现、血清IgG4水平及病理组织学所见进行综合分析。
IgG4-RD综合诊断标准[41]:(1)临床及影像学检查:累及单一或多器官的弥漫性、局灶性肿大或占位。(2)血液学检查:血清IgG4≥135 mg/dl。(3)病理组织学检查:①丰富的淋巴细胞、浆细胞浸润及席纹状纤维化;② IgG4+浆细胞浸润:IgG4+/IgG+>40%且IgG4+浆细胞数>10个/高倍镜视野。
确定诊断:(1)+(2)+(3);很可能诊断:(1)+(3);可能诊断:(1)+(2)。
备注:注意与恶性肿瘤(癌、淋巴瘤等)、相似病变(Sjögren综合征、原发性硬化性胆管炎、巨淋巴结增生症、继发性腹膜后纤维化、Wegener肉芽肿、结节病、Churg-Strauss综合征)鉴别诊断,必要时再次进行组织病理学检查。
如果不适用“综合标准”诊断IgG4-RD,应采用特定器官的IgG4-RD诊断标准。
[References]
[1] Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med, 2012, 366(6): 539-551.
[2] Joshi D, Webster GJ. Biliary and hepatic involvement in IgG4-related disease. Aliment Pharmacol Ther, 2014, 40(11-12): 1251-1261.
[3] Raj R. IgG4-related lung disease. Am J Respir Crit Care Med, 2013, 188(5): 527-529.
[4] Rodriguez EA, Williams FK. A mass in the junction of the body and tail of the pancreas w ith negative IgG4 serology: IgG4-related disease w ith negative serology. Am J Case Rep, 2015, 16: 305-309.
[5] Kam isawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol, 2003, 38(10): 982-984.
[6] Zhao YH, Wang Q, Zhou R, et al. MRI and CT fingdings of the patient with IgG4-related disease: a case report. Chin J Magn Reson Imaging, 2015, 6(3): 218-220.
赵云辉, 王倩, 周荣, 等. IgG4相关性疾病MRI和CT表现一例. 磁共振成像, 2015, 6(3): 218-220.
[7] Okazaki K, Uchida K, Koyabu M, et al. IgG4 cholangiopathy -current concept, diagnosis, and pathogenesis. J Hepatol, 2014, 61(3): 690-695.
[8] Otsuki M, Chung JB, Okazaki K, et al. Asian diagnostic criteriafor autoimmune pancreatitis: consensus of the Japan-Korea symposium on autoimmune pancreatitis. J Gastroenterol, 2008, 43(6): 403-408.
[9] Sah RP, Chari ST, Pannala R, et al. Differences in clinical profile and relapse rate of type 1 versus type 2 autoimmune pancreatitis. Gastroenterology, 2010, 139(1): 140-148, quiz e112-143.
[10] Okazaki K, Uchida K, M iyoshi H, et al. Recent concepts of autoimmune pancreatitis and IgG4-related disease. Clin Rev Allergy Immunol, 2011, 41(2): 126-138.
[11] Brito-Zerón P, Ramos-Casals M, Bosch X, et al. The clinical spectrum of IgG4-related disease. Autoimmunity Review s, 2014, 13(12): 1203-1210.
[12] Crosara S, D'Onofrio M, De Robertis R, et al. Autoimm une pancreatitis: Multimodality non-invasive imaging diagnosis. World J Gastroenterol, 2014, 20(45): 16881-16890.
[13] Takahashi N, Fletcher JG, Fidler JL, et al. Dual-phase CT of autoimmune pancreatitis: a multireader study. AJR Am J Roentgenol, 2008, 190(2): 280-286.
[14] Bodily KD, Takahashi N, Fletcher JG, et al. Autoimmune pancreatitis: pancreatic and extrapancreatic im aging findings. AJR Am J Roentgenol, 2009, 192(2): 431-437.
[15] M an fredi R, Fru lloni L, M antovani W, et al. Autoimm une pancreatitis: pancreatic and ex trapancreatic MR imaging-MR cholangiopancreatography findings at diagnosis, after steroid therapy,and at recurrence. Radiology, 2011, 260(2): 428-436.
[16] Kamisawa T, Takuma K, Anjiki H, et al. Differentiation of autoimmune pancreatitis from pancreatic cancer by diffusion-weighted MRI. Am J Gastroenterol, 2010, 105(8): 1870-1875.
[17] Zen Y, Nakanuma Y, Portmann B. Immunoglobulin G4-related sclerosing cholangitis: pathologic features and histologic m im ics. Sem in Diagn Pathol, 2012, 29(4): 205-211.
[18] Ohara H, Okazaki K, Tsubouchi H, et al. Clinical diagnostic criteria of IgG4-related sclerosing cholangitis 2012. J Hepatobiliary Pancreat Sci, 2012, 19(5): 536-542.
[19] Ferry JA, Deshpande V. IgG4-related disease in the head and neck. Semin Diagn Pathol, 2012, 29(4): 235-244.
[20] Mahajan VS, Mattoo H, Deshpande V, et al. IgG4-related disease. Annu Rev Pathol, 2014, 9: 315-347.
[21] Deshpande V. IgG4 Related Disease of the Head and Neck. Head Neck Pathology, 2015, 9(1): 24-31.
[22] Zen Y, Nakanuma Y. IgG4-related disease: a cross-sectional study of 114 cases. Am J Surg Pathol, 2010, 34(12): 1812-1819.
[23] Ho HW, Lim Z, KH TL, et al. Bilateral Kuttner tumours of the lacrimal glands. Orbit, 2011, 30(2): 96-97.
[24] Zhao LD, Shi Q, Zhan X. Immunoglobulin G4 related retroperitoneal fibrosis. Chin J Practi Int Med, 2013, 33(12): 919-922.
赵丽丹, 史群, 张烜. IgG4相关性腹膜后纤维化. 中国实用内科杂志, 2013, 33(12): 919-922.
[25] Khosroshahi A, Carruthers MN, Stone JH, et al. Rethinking Ormond's disease: "idiopathic" retroperitoneal fibrosis in the era of IgG4-related disease. Medicine (Baltimore), 2013, 92(2): 82-91
[26] Stone JR. Aortitis, periaortitis, and retroperitoneal fibrosis, as manifestations of IgG4-related system ic disease. Curr Opin Rheumatol, 2011, 23(1): 88-94.
[27] Fujimori N, Ito T, Igarashi H, et al. Retroperitoneal fibrosis associated w ith immunoglobulin G4-related disease. World J Gastroenterol, 2013, 19(1): 35-41.
[28] Umeda M, Fujikawa K, Origuchi T, et al. A case of IgG4-related pulmonary disease w ith rapid improvement. Mod Rheumatol, 2012, 22(6): 919-923.
[29] Cheuk W, Yuen HK, Chan AC, et al. Ocular adnexal lymphoma associated w ith IgG4+ chronic sclerosing dacryoadenitis: a previously undescribed complication of IgG4-related sclerosing disease. Am J Surg Pathol, 2008, 32(8): 1159-1167.
[30] Shigem itsu H, Koss MN. IgG4-related interstitial lung disease: a new and evolving concept. Curr Opin Pulm Med, 2009, 15(5): 513-516.
[31] Inoue D, Zen Y, Abo H, et al. Immunoglobulin G4-related lung disease: CT findings w ith pathologic correlations. Radiology, 2009, 251(1): 260-270.
[32] Zen Y, Inoue D, Kitao A, et al. IgG4-related lung and pleural disease: a clinicopathologic study of 21 cases. Am J Surg Pathol, 2009, 33(12): 1886-1893.
[33] Chung H, Watanabe T, Kudo M, et al. Identification and characterization of IgG4-associated autoimmune hepatitis. Liver Int, 2010, 30(2): 222-231.
[34] Ahn KS, Kang KJ, K im YH, et al. Inflammatory pseudotumors m im icking intrahepatic cholangiocarcinoma of the liver; IgG4-positivity and its clinical significance. J Hepatobiliary Pancreat Sci, 2012, 19(4): 405-412.
[35] V lachou PA, Khalili K, Jang HJ, et al. IgG4-related sclerosing disease: autoimmune pancreatitis and extrapancreatic manifestations. Radiographics, 2011, 31(5): 1379-1402.
[36] Kim B, Kim JH, Byun JH, et al. IgG4-related kidney disease: MRI findings w ith emphasis on the usefulness of diffusion-weighted imaging. Eur J Radiol, 2014, 83(7): 1057-1062.
[37] Li D, Kan Y, Fu F, et al. IgG4-related prostatitis progressed from localized IgG4-related lymphadenopathy. Int J Clin Exp Pathol, 2015, 8(9): 11747-11752.
[38] Fang JH, M in XD, Feng ZY, et al. Quantitative assessment of vascular kinetics using perfusionw eighted MRI for the differentiation of prostate cancer in the peripheral zone. Chin J Magn Reson Imaging, 2015, 6(2): 136-140.
方俊华, 闵祥德, 冯朝燕, 等. 磁共振灌注加权成像定量参数在前列腺外周带前列腺癌鉴别诊断中的价值. 磁共振成像, 2015, 6(2): 136-140.
[39] Leivo T, Koskenm ies S, Uusitalo M, et al. IgG4-related disease m im icking chalazion in the upper eyelid w ith skin manifestations on the trunk. Int Ophthalmol, 2015, 35(4): 595-597.
[40] Ohkubo H, M iyazaki M, Oguri T, et al. A rare case of IgG4-related disease involving the uterus. Rheumatology (Oxford), 2015, 54(6): 1124-1125.
[41] Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol, 2012, 22(1): 21-30.
Imaging of IgG4-related disease: current situation and update
LIU li-heng1, 2, WANG zhen-chang1, YANG zheng-han1, LI wen-wu2, JIN er-hu1*
4 Apr 2016, Accepted 30 Apr 2016
IgG4-related disease (IgG4-RD) is a chronic inflammatory disorder which could involve almost any organ of the body. Most lesions of IgG4-RD respond well to glucocorticoids and the prognoses are relatively good. However, some patients w ith IgG4-RD would be m isdiagnosed as malignant or infectious disorders from time to time in the clinic due to lack of enough recognition for the disease. In order to obtain a better umderstanding of the disease and improve the diagnostic accuracy, here we summarized the common clinical and imaging features of IgG4-RD, and reviewed the latest research progress in the literature.
IgG4-related disease; Magnetic resonance imaging; Tomography, X-ray computed; Diagnosis
1. 首都医科大学附属北京友谊医院放射科,北京 100050
2. 山东大学附属山东省肿瘤医院放射科,山东省医学科学院,济南 250117
靳二虎,E-mail:erhujin@263.net
2016-04-04
R445.2;R392
A
10.12015/issn.1674-8034.2016.07.010
*Correspondence to: Jin EH, E-mail: erhujin@263.net

