Invasive group B streptococcal infection in a patient with post splenectomy for hypersplenism secondary to liver cirrhosis and portal hypertension
Tomoya Okazaki, Toru Hifumi, Arisa Manabe, Hikari Matsumura, Satoshi Egawa, Hideyuki Hamaya, Nastuyo Shinohara, Koshiro Takano, Hajime Shishido, Yuko Abe, Kenya Kawakita, Masanobu Hagiike, Yasuhiro KurodaEmergency Medical Center, Kagawa University Hospital, Kita, Kagawa, 761-0793, Japan
Invasive group B streptococcal infection in a patient with post splenectomy for hypersplenism secondary to liver cirrhosis and portal hypertension
Tomoya Okazaki, Toru Hifumi, Arisa Manabe, Hikari Matsumura, Satoshi Egawa, Hideyuki Hamaya, Nastuyo Shinohara, Koshiro Takano, Hajime Shishido, Yuko Abe, Kenya Kawakita, Masanobu Hagiike, Yasuhiro Kuroda
Emergency Medical Center, Kagawa University Hospital, Kita, Kagawa, 761-0793, Japan
KEY WORDS:Group B streptococcal infection; Splenectomy; Liver cirrhosis
World J Emerg Med 2016;7(1):68–70
INTRODUCTION
The effi cacy of splenectomy on portal hemodynamics has been found in patients with liver cirrhosis (LC).[1]Hence the number of LC patients undergoing splenectomy will increase in the near future.
Patients in a hyposplenic state or undergoing splenectomy are highly susceptible to bacteria such as group B streptococcus (GBS) and may develop an overwhelming post-splenectomy infection (OPSI).[2]Once OPSI develops, the mortality rate of patients will be as high as 38%–69% despite aggressive critical care.[3]Immunologically, as LC itself is an independent risk factor for mortality in sepsis,[4]patients who have to undergo splenectomy with LC are considered at critical risk.Moreover, prophylaxis against GBS including vaccination and prophylactic antibiotics has not been established.[5]
This report is to describe an alarming case of invasive GBS infection in a patient after splenectomy for hypersplenism secondary to LC and portal hypertensionand highlight the need for immediate action against the possible increase of infection in this type of patients.
CASE REPORT
A 72-year-old woman with a history of splenectomy for hypersplenism secondary to liver cirrhosis and portal hypertension was admitted to our emergency department after respiratory failure.Three months before her admission, a left lateral segmentectomy of the liver for recurrent hepatocellular carcinoma and splenectomy for hypersplenism secondary to LC and portal hypertension were performed at another hospital.Four hours before presentation, the patient experienced a sudden onset of dyspnea while she was asleep.On admission, her body temperature was 38.5 °C, blood pressure 190/100 mmHg, pulse rate 120/minute, respiratory rate 30/minute, and oxygen saturation rate 98% (10 L of oxygen by face mask).Pulmonary examination revealed significant wheezing during inspiration and expiration, but no crackles and stridors.Chest radiography and computed tomography (CT) showed no infiltrates.A presumptive diagnosis of bronchial asthma caused by upper respiratory infection was made, and the patient was treated with inhaled short-acting β2-agonist, intravenous methylprednisolone, ampicillin sulbactam (ABPC/SBT), and non-invasive mechanical ventilation.Two hours later, she experienced symptom improvement, although she developed hypotension (80/46 mmHg) and sinus tachycardia.Fluid resuscitation, norepinephrine, and vancomycin (VCM) were initiated (Figure 1).Her condition stabilized and norepinephrine was gradually tapered off.Four days after admission, GBS infection was confirmed by blood culture.No obvious focus of infection was detectable.ABPC/SBT and VCM were discontinued and penicillin G was administered.Antibiotics were intravenously administered for a total of 12 days.The patient was discharged on the 12th day after admission.Vaccinations against OPSI were scheduled at the outpatient clinic of another hospital.
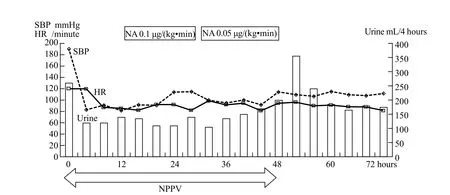
Figure 1.Hospital course.NA: noradrenaline; NPPV: non-invasive positive pressure ventilation.
DISCUSSION
In our case, although the patient with LC developed invasive GBS infection after splenectomy, a favorable outcome was obtained with appropriate management.
There is a significant increase of GBS infection in adults in contrast to a reduction of the infection in neonates and pregnant women, concomitant to an increase in elderly patients.[6]Underlying conditions such as diabetes mellitus, followed by malignancy, renal failure, and LC have been identified as risk factors for GBS infection.[6]Moreover, a study[7]showed that LC is the highest risk factor for developing invasive GBS infections.
Among organisms that induce fatal sepsis post splenectomy, Streptococcus pneumoniae is the most common, followed by Haemophilus influenzae type b and Neisseria meningitidis.[8]OPSI is characterized by high mortality despite patients being aggressively treated according to the "Surviving Sepsis Campaign" guidelines.[9]A prevention strategy with vaccination is fundamental for patients who have undergone splenectomy or have hyposplenism.According to the current guidelines, vaccination for S.pneumoniae,[10]H.influenzae type b,[11]and N.meningitidis[12]is recommended in patients with asplenia or splenic hypofunction aged over 5 years.[5]Although the currentcase also received vaccinations, a significant question pertaining to S.pneumoniae, H.influenzae type b, N.meningitides, and GBS is whether prevention by vaccination can be achieved in clinical practice.
In the absence of commercially available GBS vaccines, physicians should be aware of the increase of potential GBS infection risk related to splenectomy in LC patients.Moreover, prophylactic antibiotics against GBS have not been discussed in the guidelines.[5]
Although the effi cacy of splenectomy in LC patients was proven, the side effect of splenectomy on the immune status has not yet been thoroughly evaluated.[1]The side effects of splenectomy in LC patients, who are mainly focused on, include bleeding requiring resurgery, postoperative bleeding, and liver functions.[13]However, immune status during a longer observational period should be evaluated and indications for splenectomy should be carefully assessed while judging the risk of severe infection.
Our patient developed GBS bacteremia without a clear source, and the primary bacteremia comprised 40% of invasive GBS cases.[14]Most GBS infections in adults have no distinctive features that would lead the physicians to strongly suspect GBS infection.In the current case, we could only confirm the GBS infection once the GBS was isolated in cultures.Therefore, physicians must perform a detailed examination of host risk factors.
In conclusion, although efficacy of splenectomy in LC patients was proven, the side effect of splenectomy on the immune status during a longer observational period should be evaluated.
Funding: None.
Ethical approval: Not needed.
Conflicts of interest: The authors declare that they have no competing interests.
国家与地区在经济发展方面是相辅相成的,地区经济发展能够拉动国家整体经济的进步。我国水资源分步不均,水利工程调整水资源分布代价高昂。农田水利现代化建设能够帮助人们在农业生产和生活中提高水资源利用率,对水资源充分利用和防止浪费起到重要作用。此外,农田水利现代化建设也有助于加强对节水技术的研究和推广。
Contributors: Okazaki T wrote the manuscript.All authors read and approved the fi nal manuscript.
REFERENCES
1 Kawanaka H, Akahoshi T, Kinjo N, Iguchi T, Ninomiya M, Yamashita YI, et al.Effect of laparoscopic splenectomy on portal haemodynamics in patients with liver cirrhosis and portal hypertension.Br J Surg 2014; 101: 1585–1593.
2 Chihara D, Sakamoto T, Murakami G, Takeoka T, Ohno T.An overwhelming post-splenectomy infection with toxic shock syndrome by group B Streptococcus.Rinsho Ketsueki 2010; 51: 253–257.
3 Lynch AM, Kapila R.Overwhelming postsplenectomy infection.Infectious disease clinics of north america.Infect Dis Clin North Am 1996; 10: 693–707.
4 Lin JN, Tsai YS, Lai CH, Chen YH, Tsai SS, Lin HL, et al.Risk factors for mortality of bacteremic patients in the emergency department.Acad Emerg Med 2009; 16: 749–755.
5 Davies JM, Lewis MP, Wimperis J, Rafi I, Ladhani S, Bolton-Maggs PH, et al.Review of guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen: prepared on behalf of the British Committee for Standards in Haematology by a working party of the Haemato-Oncology task force.Br J Haematol 2011; 155: 308–317.
6 Matsubara K, Yamamoto G.Invasive group B streptococcal infections in a tertiary care hospital between 1998 and 2007 in Japan.Int J Infect Dis 2009; 13: 679–684.
7 Jackson LA, Hilsdon R, Farley MM, Harrison LH, Reingold AL, Plikaytis BD, et al.Risk factors for group B streptococcal disease in adults.Ann Intern Med 1995; 123: 415–420.
8 Holdsworth RJ, Irving AD, Cuschieri A.Postsplenectomy sepsis and its mortality rate: actual versus perceived risks.Br J Surg 1991; 78: 1031–1038.
9 Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al.Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008.Crit Care Med 2008; 36: 296–327.
10 Ardanuy C, Tubau F, Pallares R, Calatayud L, Dominguez MA, Rolo D, et al.Epidemiology of invasive pneumococcal disease among adult patients in barcelona before and after pediatric 7-valent pneumococcal conjugate vaccine introduction, 1997-2007.Clin Infect Dis 2009; 48: 57–64.
11 Kristensen K.Antibody response to a Haemophilus influenzae type b polysaccharide tetanus toxoid conjugate vaccine in splenectomized children and adolescents.Scand J Infect Dis 1992; 24: 629–632.
12 Spoulou V, Tzanakaki G, Lekka S, Chouliaras G, Ladis V, Theodoridou M.Natural and vaccine-induced immunity to Neisseria meningitidis serogroup C in asplenic patients with beta-thalassemia.Vaccine 2011; 29: 4435–4438.
13 Zhan XL, Ji Y, Wang YD.Laparoscopic splenectomy for hypersplenism secondary to liver cirrhosis and portal hypertension.World J Gastroenterol 2014; 20: 5794–5800.
14 Farley MM, Harvey RC, Stull T, Smith JD, Schuchat A, Wenger JD, et al.A population-based assessment of invasive disease due to group B Streptococcus in nonpregnant adults.N Engl J Med 1993; 328: 1807–1811.
Received June 10, 2015
Accepted after revision December 20, 2015
BACKGROUND: Splenectomy in patients with liver cirrhosis (LC) is expected to become more common owing to its effi cacy on portal hemodynamics.In this report we describe an alarming case of group B streptococcus (GBS) infection after splenectomy in a patient with LC.
METHODS: A 72-year-old woman with a history of LC was admitted to our emergency department because of respiratory failure.The patient had received left lateral segmentectomy of the liver and splenectomy three months before admission.Pulmonary examination revealed significant wheezing during inspiration and expiration, but no crackles and stridor.Chest radiography and CT showed no infiltrates.A presumptive diagnosis of bronchial asthma caused by upper respiratory infection was made.Four days after admission, GBS infection was confirmed by blood culture and penicillin G was administered.Antibiotics were given intravenously for a total of 12 days.
RESULTS: The patient was discharged on the 12th day after admission.
CONCLUSIONS: Although efficacy of splenectomy in patients with LC has been reported, immune status should be evaluated for a longer period.Patients who have undergone splenectomy are highly susceptible to bacteria; moreover, LC itself is an independent risk factor for mortality in patients with sepsis.Since prophylaxis against GBS has not been established, immediate action should be taken.Emergency physicians should be aware of invasive GBS infection in the context of the critical risk factors related to splenectomy and LC, particularly the expected increase of splenectomy performed in LC patients.
Corresponding Author:Toru Hifumi, Email: hifumitoru@gmail.com
DOI:10.5847/wjem.j.1920–8642.2016.01.013
Case Report
 World journal of emergency medicine2016年1期
World journal of emergency medicine2016年1期
- World journal of emergency medicine的其它文章
- Airway foreign bodies: A critical review for a common pediatric emergency
- End-tidal capnometry during emergency department procedural sedation and analgesia: a randomized, controlled study
- Intranasal ketamine for the treatment of patients with acute pain in the emergency department
- Analgesic effect of paracetamol combined with lowdose morphine versus morphine alone on patients with biliary colic: a double blind, randomized controlled trial
- Comparison of intravenous pantoprazole and ranitidine in patients with dyspepsia presented to the emergency department: a randomized, double blind, controlled trial
- A correlation analysis of Broselow™ Pediatric Emergency Tape-determined pediatric weight with actual pediatric weight in India
