体质量指数与食管贲门腺癌发病风险相关性Meta分析
王君化, 蒋 谦, 孙静锋, 周国志
1. 西安市第四医院消化内科,陕西 西安 710004;2. 南京医科大学附属逸夫医院肿瘤中心
其他论著
体质量指数与食管贲门腺癌发病风险相关性Meta分析
王君化1, 蒋 谦2, 孙静锋2, 周国志2
1. 西安市第四医院消化内科,陕西 西安 710004;2. 南京医科大学附属逸夫医院肿瘤中心
目的 分析不同体质量指数(BMI)与食管贲门腺癌发病风险相关性。方法 通过Medline、PubMed、Embase、WOS检索至2015年相关文献,统计分析BMI与食管、贲门腺癌的发病关系。结果 22项研究入选病例数共1 307 549例,其中试验组7 718例,对照组1 299 831例。BMI 25~30 kg/m2,贲门、食管腺癌发病总风险RR=1.56,95%CI:1.46~1.68(P=0.000);食管腺癌RR=1.82,95%CI:1.57~2.11(P=0.00);贲门腺癌RR=3.47,95%CI:1.93~6.25(P=0.000);贲门、食管同时癌变RR=1.47,95%CI:1.35~1.59(P=0.000)。BMI≥30 kg/m2,贲门、食管腺癌发病相对风险RR=2.19,95%CI:1.96~2.45(P=0.000);贲门及食管同时发生癌变相对风险RR=2.11,95%CI:1.86~2.39(P=0.000);贲门腺癌发生风险RR=2.58,95%CI:1.24~5.35(P=0.011);食管腺癌发生风险RR=2.49,95%CI:1.95~3.17(P=0.000)。结论 BMI>25 kg/m2时,贲门、食管腺癌发病率明显升高。
体质量指数;食管腺癌;贲门腺癌;Meta分析;肥胖;超重
近几年,胃癌和食管癌发病率上升,特别是发达国家中食管与贲门交界处的癌发病率上升明显[1]。2007年Holmes等[2]报道食管、贲门腺癌同高体质量指数(body mass index,BMI)存在密切关系,超重人群中食管和贲门腺癌患病人群增加超过40%。控制肥胖、降低BMI能预防及减少贲门及食管腺癌的发病率。BMI能增加贲门、食管腺癌发病风险循证医学证据不足[3]。本文通过研究BMI和食管、贲门腺癌关系,为食管、贲门腺癌一级预防提供客观依据。
1 资料和方法
1.1 检索策略 以‘body mass index’ or ‘BMI’ or ‘obesity’ and combinations of ‘esophageal neoplasms’ or ‘stomach neoplasms’ and ‘adenocarcinoma’作为检索词,采取自由词同关键词相结合方式通过Medline、PubMed、Embase、WOS检索至2015年相关文献,中文研究资料真实性欠佳,为了保证本研究质量,本次不予纳入。
1.2 纳入标准 (1)所有资料类型均为队列研究或前瞻对照研究;(2)研究对象BMI和食管、贲门腺癌之间的风险联系;(3)具有暴露结果指标如RR、OR、95%CI、P值等。
1.3 排除标准 (1)回顾性研究;(2)重复报道;(3)资料中没有涉及RR及95%CI;(4)同一研究多篇文献的取最近一次文献,排除其他文献。
1.4 资料收集 初次检索:通过检索并仔细阅读全文,共有22篇国外文献纳入研究。再次检索:根据以上检索所得到文献的参考文献进行扩大检索,未发现新的符合条件的文献。
1.5 统计学分析 采用Stata 11.0统计软件进行分析,取得BMI同贲门、食管腺癌相对风险及95%CI,进行分层分析各研究之间异质性差异判定用χ2检验,用统计量Q表示,其中P<0.05表示纳入资料存在异质性,使用随机效应模型,反之表示资料不存在异质性用固定效应模型。分析结果用RR值和95%CI表示,P<0.05为差异有统计学意义。
2 结果
2.1 文献检索结果 最终纳入的文献为22篇[4-25]。所有评分均为>3分的高质量文献,入选病例共1 307 549例,其中试验组7 718例,对照组1 299 831例;详细的文献特征及数据如表1所示。
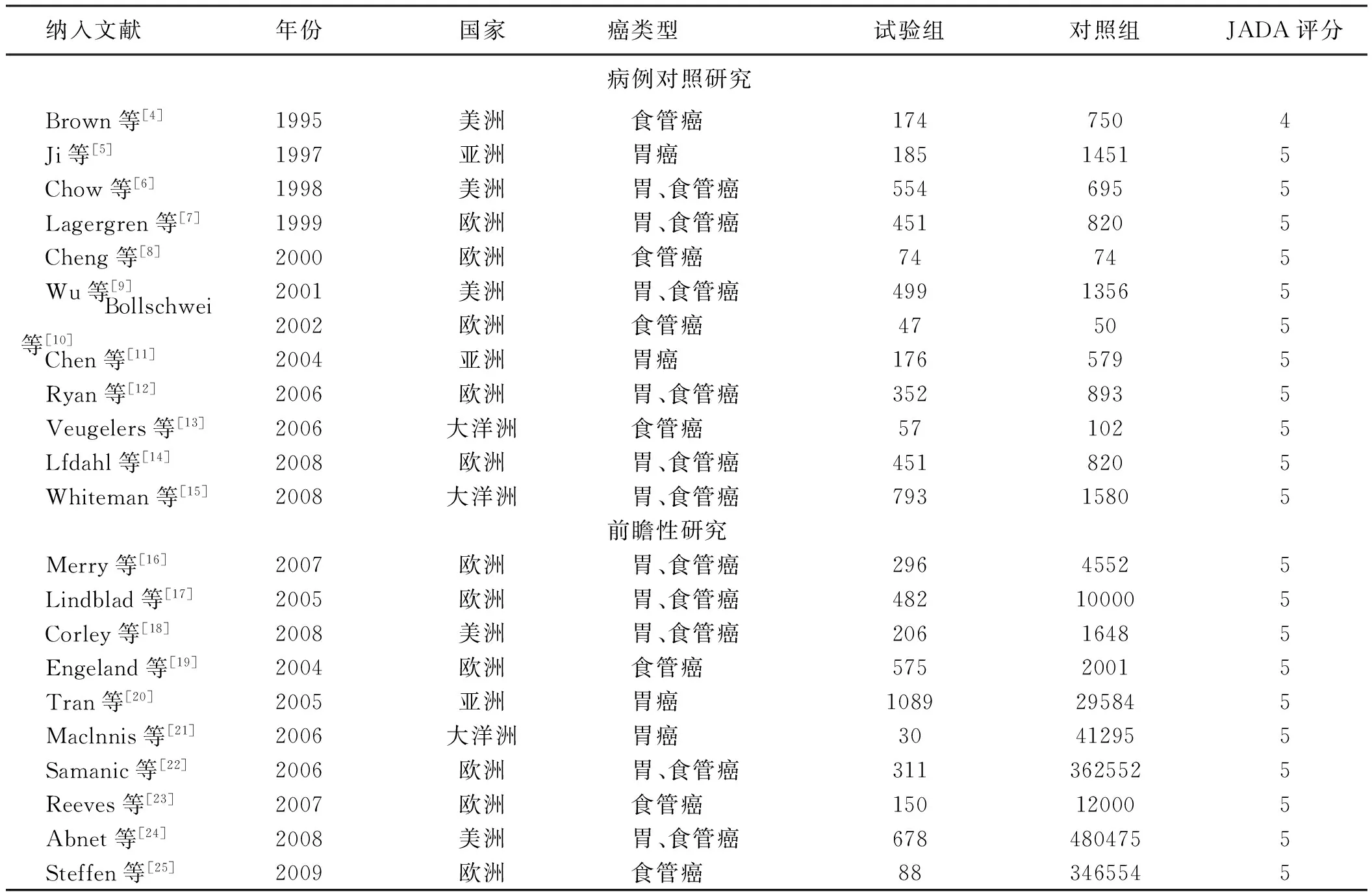
表1 纳入研究的资料特征Tab 1 Characteristics of included studies
2.2 Meta分析结果 BMI 25~30 kg/m2:贲门、食管腺癌发病相对风险分析中I2=65.7%,采用固定效用模型,贲门、食管腺癌发病相对风险RR=1.56,95%CI:1.46~1.68,差异有统计学意义(P=0.000)。(1)部位分层:食管癌变发生风险I2=57.7%,采用固定效用模型相对风险RR=1.82,95%CI:1.57~2.11,差异有统计学意义(P=0.00);贲门癌变发生风险I2=18.9%,采用随机效用模型RR=3.47,95%CI:1.93~6.25,差异有统计学意义(P=0.000);贲门、食管同时癌变发生风险I2=64.5%,采用固定效用模型RR=1.47,95%CI:1.35~1.59,差异有统计学意义(P=0.000)(见图1);(2)地域分层:美洲发生风险I2=28.6%,采用随机效用模型相对风险RR=1.53,95%CI:1.36~1.72,差异有统计学意义(P=0.000);亚洲发生风险I2=50.4%,采用随机效用模型RR=3.93,95%CI:1.97~7.81,差异有统计学意义(P=0.00);欧洲发生风险I2=71.0%,采用随机效用模型RR=1.65,95%CI:1.49~1.82,差异有统计学意义(P=0.00);大洋洲发生风险I2=14.7%,采用随机效用模型RR=1.14,95%CI:0.90~1.43,差异无统计学意义(P=0.284)(见图2);(3)性别分层:男性发生风险I2=82.4%,采用随机效用模型相对风险RR=1.75,95%CI:1.54~2.00,差异有统计学意义(P=0.000);女性发生风险I2=0,采用随机效用模型RR=1.64,95%CI:1.30~2.07,差异有统计学意义(P=0.00);未分男女研究发生风险I2=58.7%,采用固定效用模型RR=1.47,95%CI:1.34~1.61,差异有统计学意义(P=0.00)(见图3)。BMI≥30 kg/m2贲门、食管腺癌发病相对风险分析中I2=53.6%,采用随机效用模型,发病相对风险RR=2.19,95%CI:1.96~2.45,差异有统计学意义(P=0.000)。(1)部位分层:贲门及食管同时发生癌变分析I2=73.0%,采用固定效用模型,发病相对风险RR=2.11,95%CI:1.86~2.39,差异有统计学意义(P=0.000);贲门癌变发生风险I2=0,采用随机效用模型RR=2.58,95%CI:1.24~5.35,差异有统计学意义(P=0.011);食管癌变发生风险I2=0,采用固定效用模型RR=2.49,95%CI:1.95~3.17,差异有统计学意义(P=0.000)(见图4);(2)地域分层:欧洲发生风险I2=66.5%,采用随机效用模型相对风险RR=2.36,95%CI:2.01~2.76,差异有统计学意义(P=0.000);大洋洲发生风险I2=18.3%,采用随机效用模型RR=2.11,95%CI:1.64~2.71,差异有统计学意义(P=0.000);美洲发生风险I2=0,采用随机效用模型RR=2.00,95%CI:1.64~2.44,差异有统计学意义(P=0.000)(见图5);(3)性别分层:男性发生风险I2=72.3%,采用随机效用模型相对风险RR=2.07,95%CI:1.58~2.72,差异有统计学意义(P=0.000);女性发生风险I2=0,采用随机效用模型RR=2.30,95%CI:1.62~3.25,差异有统计学意义(P=0.00);未分男女研究发生风险I2=63.1%,采用固定效用模型RR=2.20,95%CI:1.94~2.51,差异有统计学意义(P=0.006)(见图6)。

图1 BMI 25~30 kg/m2时贲门、食管腺癌相对风险部位分层分析
Fig 1 Site stratification analysis of the relative risk of esophageal and gastric cardia adenocarcinoma when BMI was 25~30 kg/m2

图2 BMI 25~30 kg/m2时贲门、食管腺癌相对风险洲际分层分析
Fig 2 Intercontinental stratification analysis of the relative risk of esophageal and gastric cardia adenocarcinoma when BMI was 25~30 kg/m2

图3 BMI 25~30 kg/m2时贲门、食管腺癌相对风险性别分层分析
Fig 3 Gender stratification analysis of the relative risk of esophageal and gastric cardia adenocarcinoma when BMI was 25~30 kg/m2
图4 BMI≥30 kg/m2时贲门、食管腺癌相对风险部位分层分析
Fig 4 Site stratification analysis of the relative risk of esophageal and gastric cardia adenocarcinoma when BMI was more than 30 kg/m2

图5 BMI≥30 kg/m2时贲门、食管腺癌相对风险洲际分层分析
Fig 5 Intercontinental stratification analysis of the relative risk of esophageal and gastric cardia adenocarcinoma when BMI was more than 30 kg/m2

图6 BMI≥30 kg/m2时贲门、食管腺癌相对风险性别分层分析
Fig 6 Gender stratification analysis of the relative risk of esophageal and gastric cardia adenocarcinoma when BMI was more than 30 kg/m2
2.3 偏倚识别 漏斗图显示基本对称,Begg’s检验P=0.058,表示发表偏倚小,可信度高,分析结果可靠,客观性强,统计学意义大(见图7)。

图7 纳入文献的漏斗图Fig 7 Funnel plot of included stuides
3 讨论
食管、贲门腺癌有多种病因,烟草使用、Barrett’s食管是公认的危险因素,其他因素如饮食、胆囊切除、下食管括约肌松弛、哮喘药物、阿司匹林、非甾体类抗炎药物的使用和家族史也可能引起食管、贲门腺癌,另外,肥胖也同食管、贲门腺癌发病关系密切。我们通过对文献的综合分析,研究BMI同贲门、食管腺癌发病风险发现,BMI 25~30 kg/m2时,贲门、食管交界癌发生风险升高46%~68%,平均升高57%,BMI≥30 kg/m2时,食管、贲门腺癌风险增加两倍。
我们分析体质量增加导致食管、贲门腺癌风险上升主要有以下几方面原因:超重和肥胖能促进食管上皮细胞增生和分化形成Barrent’s食管,继续发展有可能成为食管癌[26]。另外,肥胖本身腹部压力大,对贲门、食管有挤压作用,胃酸被挤压后容易突破食管下括约肌压力进入食管,刺激下段食管黏膜引起食管上皮分化[27]。肥胖患者堆积的脂肪组织过多,过多的脂肪组织增加内源性激素的浓度,包括性激素、胰岛素和胰岛素生长因子1,这些激素能加速细胞增殖,延缓细胞凋亡,从而导致细胞增生凋亡障碍造成组织过度增生[28]。肥胖是世界上一个公认的促炎因子,它通过增加炎症介质的释放,促进肿瘤细胞的快速生长[29]。肥胖者因腹内压和胸腔内压增加导致食管内食物不易通过食管进入胃部,食物同食管上皮接触时间自然延长,食品中可能致癌的成分可能促进食管、贲门部黏膜的增殖及异常分化[30]。
综上所述,随着体质量增加,食管、贲门腺癌发病风险大幅度增加,预防肥胖、控制体质量、健康饮食显得尤为重要。本研究尚有以下不足:(1)纳入的文献数量少;(2)总病例数不大,缺乏临床多中心研究;(3)各个研究之间存在偏倚。期待更多的研究及更大的样本量、更广泛的资料佐证本研究的结论。
[1]Bosetti C,Levi F,Ferlay J,et al. Trends in oesophageal cancer incidence and mortality in Europe [J]. Int J Cancer,2008,122(5): 1118-1129.
[2]Holmes RS,Vaughan TL. Epidemiology and pathogenesis of esophageal cancer [J]. Semin Radiat Oncol,2007,17(1): 2-9.
[3]Olsen CM,Pandeya N,Green AC,et al. Population attributable fractions of adenocarcinoma of the esophagus and gastroesophageal junction [J]. Am J Epidemiol,2011,174(5): 582-590.
[4]Brown LM,Swanson CA,Gridley G,et al. Adenocarcinoma of the esophagus: role of obesity and diet [J]. J Natl Cancer Inst,1995,87(2): 104-109.
[5]Ji BT,Chow WH,Yang G,et al. Body mass index and the risk of cancers of the gastric cardia and distal stomach in Shanghai,China [J]. Cancer Epidemiol Biomarkers Prev,1997,6(7): 481-485.
[6]Chow WH,Blot WJ,Vaughan TL,et al. Body mass index and risk of adenocarcinomas of the esophagus and gastric cardia [J]. J Natl Cancer Inst,1998,90(2): 150-155.
[7]Lagergren J,Bergström R,Nyrén O. Association between body mass and adenocarcinoma of the esophagus and gastric cardia [J]. Ann Intern Med,1999,130(11): 883-890.
[8]Cheng KK,Sharp L,McKinney PA,et al. A case-control study of oesophageal adenocarcinoma in women: a preventable disease [J]. Br J Cancer,2000,83(1): 127-132.
[9]Wu AH,Wan P,Bernstein L. A multiethnic population-based study of smoking,alcohol and body size and risk of adenocarcinomas of the stomach and esophagus (United States) [J]. Cancer Causes Control,2001,12(8): 721-732.
[10] Bollschweiler E,Wolfgarten E,Nowroth T,et al. Vitamin intake and risk of subtypes of esophageal cancer in Germany [J]. J Cancer Res Clin Oncol,2002,128(10): 575-580.
[11]Chen MJ,Wu DC,Ko YC,et al. Personal history and family history as a predictor of gastric cardiac adenocarcinoma risk: a case-control study in Taiwan [J]. Am J Gastroenterol,2004,99(7): 1250-1257.
[12]Ryan AM,Rowley SP,Fitzgerald AP,et al. Adenocarcinoma of the oesophagus and gastric cardia: male preponderance in association with obesity [J]. Eur J Cancer,2006,42(8): 1151-1158.
[13]Veugelers PJ,Porter GA,Guernsey DL,et al. Obesity and lifestyle risk factors for gastroesophageal reflux disease,Barrett esophagus and esophageal adenocarcinoma [J]. Dis Esophagus,2006,19(5): 321-328.
[14]Löfdahl HE,Lu Y,Lagergren J. Sex-specific risk factor profile in oesophageal adenocarcinoma [J]. Br J Cancer,2008,99(9): 1506-1510.
[15]Whiteman DC,Sadeghi S,Pandeya N,et al. Combined effects of obesity,acid reflux and smoking on the risk of adenocarcinomas of the oesophagus [J]. Gut,2008,57(2): 173-180.
[16]Merry AH,Schouten LJ,Goldbohm RA,et al. Body mass index,height and risk of adenocarcinoma of the oesophagus and gastric cardia: a prospective cohort study [J]. Gut,2007,56(11): 1503-1511.
[17]Lindblad M,Rodríguez LA,Lagergren J. Body mass,tobacco and alcohol and risk of esophageal,gastric cardia,and gastric non-cardia adenocarcinoma among men and women in a nested case-control study [J]. Cancer Causes Control,2005,16(3): 285-294.
[18]Corley DA,Kubo A,Zhao W. Abdominal obesity and the risk of esophageal and gastric cardia carcinomas [J]. Cancer Epidemiol Biomarkers Prev,2008,17(2): 352-358.
[19]Engeland A,Tretli S,Bjrge T. Height and body mass index in relation to esophageal cancer; 23-year follow-up of two million Norwegian men and women [J]. Cancer Causes Control,2004,15(8): 837-843.
[20]Tran GD,Sun XD,Abnet CC,et al. Prospective study of risk factors for esophageal and gastric cancers in the Linxian general population trial cohort in China [J]. Int J Cancer,2005,113(3): 456-463.
[21]Maclnnis RJ,English DR,Hopper JL,et al. Body size and composition and the risk of gastric and oesophageal adenocarcinoma [J]. Int J Cancer,2006,118(10): 2628-2631.
[22]Samanic C,Chow WH,Gridley G,et al. Relation of body mass index to cancer risk in 362,552 Swedish men [J]. Cancer Causes Control,2006,17(7): 901-909.
[23]Reeves GK,Pirie K,Beral V,et al. Cancer incidence and mortality in relation to body mass index in the Million Women Study: cohort study [J]. BMJ,2007,335(7630): 1134.
[24]Abnet CC,Freedman ND,Hollenbeck AR,et al. A prospective study of BMI and risk of oesophageal and gastric adenocarcinoma [J]. Eur J Cancer,2008,44(3): 465-471.
[25]Steffen A,Schulze MB,Pischon T,et al. Anthropometry and esophageal cancer risk in the European prospective investigation into cancer and nutrition [J]. Cancer Epidemiol Biomarkers Prev,2009,18(7): 2079-2089.
[26]Travier N,Agudo A,May AM,et al. Smoking and body fatness measurements: a cross-sectional analysis in the EPIC-PANACEA study [J]. Prev Med,2009,49(5): 365-373.
[27]Lubin JH,Cook MB,Pandeya N,et al. The importance of exposure rate on odds ratios by cigarette smoking and alcohol consumption for esophageal adenocarcinoma and squamous cell carcinoma in the Barrett’s Esophagus and Esophageal Adenocarcinoma Consortium [J]. Cancer Epidemiol,2012,36(3): 306-316.
[28]McMillan DC,Sattar N,McArdle CS. ABC of obesity. Obesity and cancer [J]. BMJ,2006,333(7578): 1109-1111.
[29]Travier N,Agudo A,May AM,et al. Smoking and body fatness measurements: a cross-sectional analysis in the EPIC-PANACEA study [J]. Prev Med,2009,49(5): 365-373.
[30]Peleteiro B,La Vecchia C,Lunet N. The role of Helicobacter pylori infection in the web of gastric cancer causation [J]. Eur J Cancer Prev,2012,21(2): 118-125.
(责任编辑:陈香宇)
Meta-analysis of body mass index and esophageal and gastric cardia adenocarcinoma
WANG Junhua1,JIANG Qian2,SUN Jingfeng2,ZHOU Guozhi2
1. Department of Gastroenterology,the Fourth Hospital of Xi’an,Xi’an 710004; 2. Center of the Tumor,Affiliated Yifu Hospital of Nanjing Medical University,China
Objective To evaluate the relationship of body mass index (BMI) with esophageal and gastric cardia adenocarcinoma.Methods Related articls (1990-2015) were searched in Medline,PubMed,Embase,WOS. The qualities of the included studies were evaluated by the Jadad scale.RRand 95%CIwere evaluated by Meta-analysis.Results A total of 22 studies were adopted,and the number of cases was 1 307 549,experimental group had 7 718 cases,control group had 1 299 831 cases. The Meta-analysis showed that: when BMI was 25-30 kg/m2,esophageal or gastric cardia adenocarcinomaRRwas 1.56 (95%CI: 1.46-1.68,P=0.000); esophageal adenocarcinomaRRwas 1.82 (95%CI: 1.57-2.11,P=0.00); gastric cardia adenocarcinomaRRwas 3.47 (95%CI: 1.93-6.25,P=0.000); esophageal and gastric cardia adenocarcinomaRRwas 1.47 (95%CI: 1.35-1.59,P=0.000). BMI was more than 30 kg/m2,esophageal or gastric cardia adenocarcinomaRRwas 2.19 (95%CI: 1.96-2.45,P=0.000); esophageal and gastric cardia adenocarcinomaRRwas 2.11 (95%CI: 1.86-2.39,P=0.000); gastric cardia adenocarcinomaRRwas 2.58 (95%CI: 1.24-5.35,P=0.011); esophageal adenocarcinomaRRwas 2.49 (95%CI: 1.95-3.17,P=0.000). Conclusion The morbidity of esophageal and gastric cardia adenocarcinoma is high when BMI is more than 25 kg/m2.
Body mass index; Esophageal adenocarcinoma; Gastric cardia adenocarcinoma; Meta-analysis; Obesity; Overweight
10.3969/j.issn.1006-5709.2016.04.022
王君化,主治医师,研究方向:消化内科疾病基础及临床。E-mail:7868137586@qq.com
周国志,硕士,主任医师,研究方向:肿瘤疾病的基础及临床。E-mail:124278956@qq.com
R735
A
1006-5709(2016)04-0439-05
2015-08-03