Smoking and Passive Smoking
Russell V. Luepker, MD, MS
Introduction
The addictive cigarette smoking habit is a leading cause of death and disability from chronic diseases around the world. In industrialized countries, tobacco use contributes the largest number of years of life lost [1]. In the United States it is estimated that more than 480,000 deaths annually are associated with smoking, and cardiovascular diseases are a leading cause [2] (Figure 1). Although smoking rates have declined in wealthy countries,there are increasing rates of smoking in low- and middle-income countries [3] (Figure 2). Many people have quit smoking, but younger smokers are recruited; those who remain are addicted and are particularly difficult to treat [4]. Cigarette smoking also affects nonsmokers through passive or secondhand smoke [5]. The scientific evidence underlying the dangers of cigarette smoking and tobacco use are described herein along with trends in cigarette use and strategies for prevention and cessation of the cigarette-smoking habit.
Cigarette Smoking and Cardiovascular Disease
The causal relationship of lung cancer with cigarette smoking has been known for many decades.Cardiovascular diseases were first suggested as an outcome of cigarette smoking in the early 1960s.In 1962, epidemiologic studies from Framingham,Massachusetts, and Albany, New York, found an association between coronary heart disease and smoking among men [6, 7]. Further studies found a similar association among women and included other cardiovascular diseases [7]. It is now known that smoking is associated with all the major cardiovascular diseases, including coronary artery disease, myocardial infarction, sudden death, stroke,and peripheral artery disease [7]. These associations are found in all sex, age, ethnic, and racial groups. Smoking cessation can have a profound impact on reducing the incidence of these diseases[8, 9].
The Multiple Risk Factor Intervention Trial screened 316,099 men and demonstrated a graded relationship between the number of cigarettes smoked daily and the relative risk of death from coronary heart disease [10]. The relative risk is 2.1 for consumption of 1–25 cigarettes per day,rising to 2.9 for more than 25 cigarettes per day.The Multiple Risk Factor Intervention Trial and many other studies demonstrate that quitting smoking reduces incident cardiovascular disease morbidity and mortality [9, 11]. It is also known that those who quit smoking following an acute event such as a myocardial infarction have a signi ficantly improved prognosis [12].
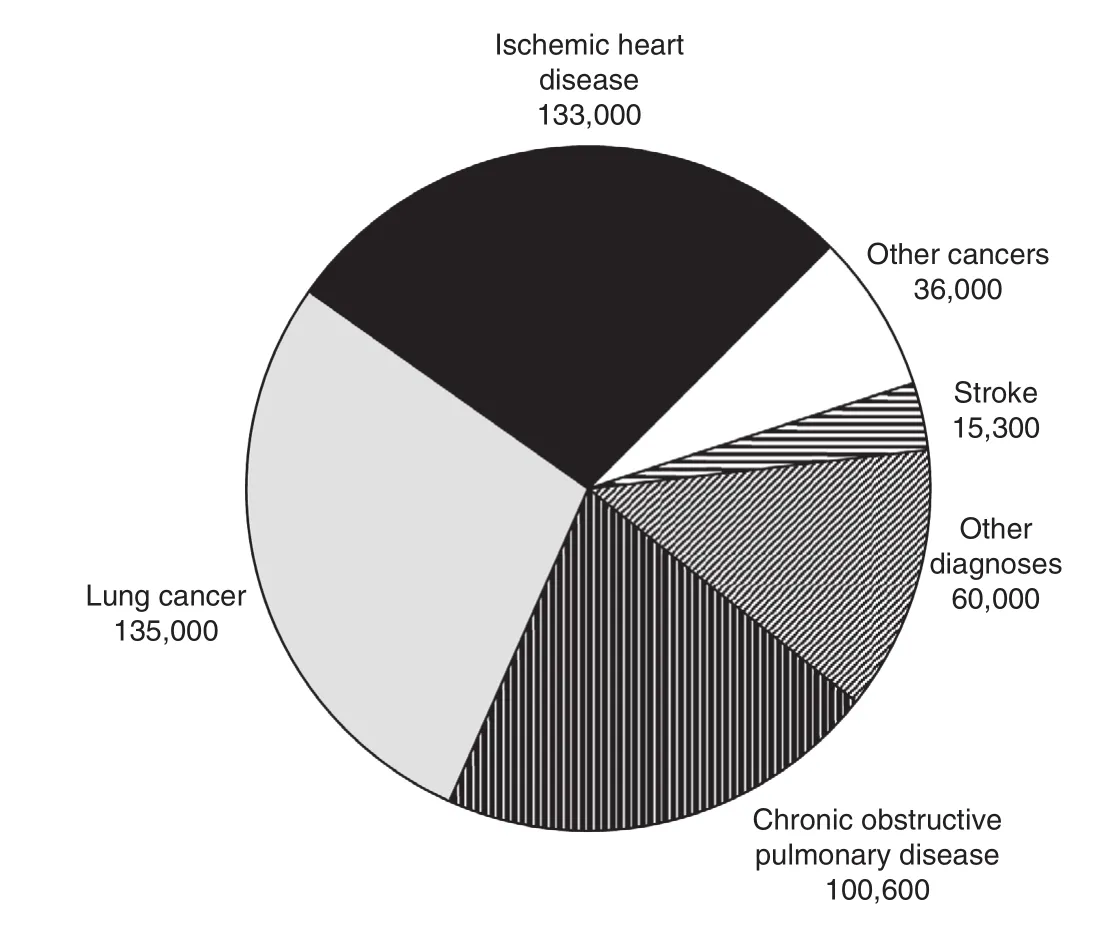
Figure 1: More than 480,000 US Deaths Each Year From Cigarette Smoking, Including Secondhand Smoke.Source: http://www.surgeongeneral.gov/library/reports/50-years-of-progress/sgr50-chap-12.pdf( accessed 2016 May 30).
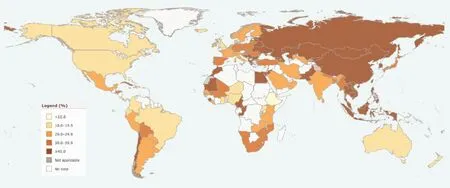
Figure 2: Prevalence of Tobacco Smoking. Age-Standardized Prevalence of Current Tobacco Smoking Among Males Aged 15 Years or Older (%), 2015.Source: http://gamapserver.who.int/gho/interactive_charts/tobacco/use/atlas.html.
The interaction of cigarette smoking with other established risk factors is also well described, with some suggesting the outcome is additive, whereas others argue there is a multiplier effect (Figure 2).Smoking adds to cardiovascular risk with hypertension, lipid abnormalities, diabetes, obesity,oral contraception use, and electrocardiogram abnormality [13–16]. Experiments in laboratory animals and humans have advanced our understanding of the mechanisms by which cigarette smoking can in fluence cardiovascular disease both acutely and chronically. The pharmacologic effects of nicotine are many, including sympathetic stimulation and coronary vasoconstriction[15]. Carbon monoxide in cigarette smoke binds to hemoglobin and reduces the oxygen-carrying ability of the blood. Other components of cigarette smoke increase platelet activation and other thrombotic factors. The many toxic chemicals found in cigarette smoke are associated with increased in flammation, endothelial dysfunction, and a prothrombotic state [16].
Secondhand Smoke
A 2006 US Surgeon General report entitled “Health consequences of involuntary exposure to tobacco smoke” is focused on environmental exposure [5].It describes signi ficant increases in the incidence of cardiovascular and other diseases among those exposed to secondhand tobacco smoke.
A subsequent review by the Institute of Medicine came to similar conclusions [17]. Exposure to secondhand smoke increases the risk of coronary heart disease by 25–30%. Other studies demonstrate that the incidence of myocardial infarctions decreased after a smoking ban was implemented, with decreases ranging from 6% to 47%. In addition to cardiovascular diseases, secondhand smoke is also associated with cancer and respiratory diseases [17].A comparison of home-based and worksite studies reported an overall increased risk of cardiovascular diseases associated with environmental smoke but found no differences between smoke exposure in the home or at work [18].
The mechanisms by which secondhand smoke affects others is debated; they probably resemble the pathway in the primary smoker but may have other effects. Mainstream smoke, which is inhaled by the primary smoker, differs from sidestream smoke, which is released into the environment [5].It is possible that sidestream smoke may be more toxic, and physiologic changes among nonsmokers who are regularly exposed to cigarette smoke could have widespread effects. These include lower levels of high-density lipoprotein cholesterol, increased atrial fibrillation, and platelet abnormality [5]. Also observed are endothelial dysfunction and lower exercise tolerance. All these factors are associated with increased incidence of cardiovascular disease and, coupled with the positive effects of smoking bans on nonsmokers, reinforce the importance of reducing exposure to secondhand smoke.
Trends in Cigarette Smoking
Following World War II, cigarette smoking became common in the United States with the return of soldiers [6]. Cigarettes were provided as part of food rations (K-rations) used by the military [6]. Women gradually attained equivalency with men in smoking rates. By 1965 cigarette smoking was a habit of 42.4% of adults [19]. Since that peak in 1965,cigarette smoking has steadily declined nationally with smokers quitting and many never acquiring the habit [19]. By 2014, 17% of the adult population aged 18 years or older were regular smokers.Trends in smoking by sex and race are depicted in Figure 3. Declines in smoking have been observed in all groups but higher rates continue to be observed in white and black men and white women. The rates for Hispanics/Latinos and Asians are the lowest [20]. The trend of decline is likely to continue as most smokers describe an interest in quitting and approximately half attempted to quit during the previous year [19]; however, only 6%were successful.
Historically, smoking begins in middle school and becomes regular in high school [4]. Smokers became addicted as they grew older and more liberated from the constraints of home and school. However, more recent data show cigarette smoking among those aged 12–17 years has fallen signi ficantly, with the percentage of adolescents using tobacco products decreasing from 15.2% in 2003 to 7.8% in 2013.New regulations led the tobacco industry to focus more on young adults who are able to legally smoke and have the economic resources to buy cigarettes.This approach has had some success, with men and women aged 18–44 years having higher smoking rates than the general population [20]. Many in this group are certain that they will not become addicted and can quit later in life.
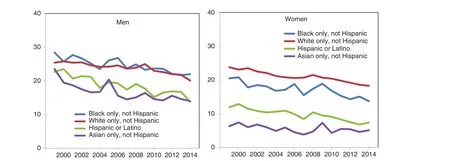
Figure 3: Current Cigarette Smoking Among Adults Aged 18 Years or Older, by Sex and Race and Hispanic Origin:United States, 1999–2014.Source: Centers for Disease Control and Prevention/National Center for Health Statistics, National Health Interview Survey.
Lowering Tobacco Use Among Youth
The tobacco smoking habit begins among youth and young adults. Research was initially described in the 1994 Surgeon General’s report on preventing tobacco use among young people, and more recent research is summarized in the Surgeon General’s report of 2012 [4]. Use of mass media is one approach, with messages presented multiple times over media channels viewed by this age group.These messages are mainly on television and radio[4]. Media strategies that are aimed at adults also have an effect on youth.
Regulatory approaches are also useful in reducing tobacco use among youth. Youth are particularly sensitive to increased cigarette prices resulting from tobacco taxes. Increased costs reduce the likelihood of youth starting smoking and reduce the number of cigarettes smoked. Young smokers are affected by regulations eliminating tobacco use in public places. A combination of increased taxation, use of mass media, restriction of public smoking, and prevention programs in schools has been shown to be effective in reducing cigarette smoking among youth as shown by the steady decline of cigarette use in this age group [21].
Although the smoking of cigarettes among youth is falling, a new trend is emerging to take its place, the use of electronic cigarettes (e-cigarettes)among middle and high school students [22]. In 2015, e-cigarettes became the most commonly used tobacco product among middle (5.3%) and high (16%) school students. The use of hookahs also increased in this age group. Although marketed as a safe cigarette and a way to quit smoking,e-cigarettes are a path to addiction. The use of fruit and other flavors suggests that youth are the targeted audience. Unfortunately, these products are new and less is known about the long-term health effects or conversion rates to regular tobacco use.Many have called for increasing regulation of these new alternatives [23].
Smoking Cessation Approaches
Most current smokers report a desire to quit the habit. In 2013 approximately two-thirds of adult smokers reported they had attempted to quit in the previous year [24]. Unfortunately only a small proportion (6%) reported a successful quit attempt.Numerous programs are available in communities to aid in quit attempts. These include behavioral approaches, pharmacologic intervention,and other strategies. Many resources are available to help individuals who wish to quit smoking.They include the Centers for Disease Control and Prevention Helping Quit Smoking Program (http://www.cdc.gov/tobacco/quit_smoking/how_to_quit/index.htm), resources from the American Heart Association (http://www.heart.org/HEARTORG/HealthyLiving/QuitSmoking/QuittingResources/Resources-to-Help-You-Quit-Smoking_UCM_307934_Article.jsp#.V1rWfdddQ4t), and resources from the National Institutes of Health(https://www.nlm.nih.gov/medlineplus/healthtopics.html).
Behavioral Strategies
Nicotine is an addictive substance, and behavioral approaches to smoking cessation are critical tools. Successful programs, including those using nicotine replacement or other pharmaceuticals, are best when combined with behavioral treatment components. Many behavioral approaches have been tested alone with differing degrees of success.Specific behavioral components include aversive smoking, intratreatment social support, problem solving skills training, quit date setting, specific social support, weight control, nutrition, exercise,contingency contracts, relaxation techniques, and cigarette fading. Although many of these strategies are not very effective alone, they may work in combination.
Pharmacologic Interventions
Environmental cues and triggers encourage smoking for all smokers. These can be addressed in behavioral programs; however, nicotine addiction is a common theme in many patients [25]. A number of pharmacologic agents are recognized as effective by the Food and Drug Administration(FDA), and these will be discussed below. There are also agents that have been used “off label” or without FDA approval. These will not be discussed here. Many of the agents involve some form of nicotine replacement: nicotine gum, nicotine inhaler,nicotine lozenges, nicotine nasal spray, and nicotine patches. Each has its advantages and disadvantages. All may result in a new dependency among some smokers.
The nicotine patch is convenient and needs to be applied once each day. It allows flexible dosing, and once it has been placed on the skin, the delivery of nicotine is consistent but slow. Nicotine gum allows flexible dosing but can be more difficult to use correctly. Many gum users do not adequately dose themselves with this medication.Nicotine nasal spray has the advantage of flexible dosing plus it provides faster delivery of the drug.For many users, nasal and eye irritation is a problem as frequent use may be necessary to build an adequate nicotine dose. The nicotine inhaler allows more flexible dosing and mimics the hand-to-mouth behavior of smoking. The inhaler also has fewer side effects. The nicotine lozenge is convenient and allows flexible dosing. Nicotine replacement therapy has been found to be effective in randomized trials [26]. Some nicotine replacement therapies are available without a prescription, whereas others require a physician’s approval.
Bupropion hydrochloride is approved by the FDA for smoking cessation and is available in tablet form. It appears to act on brain chemistry to mimic the effects of nicotine among smokers. There is evidence to suggest that a combination of a nicotine patch and bupropion use may be more effective than use of either alone [27]. Bupropion has been available for many years as an antidepressant, however,it works well in smokers without the symptoms of depression. It has the potential side effects of all antidepressants, including suicidality, depression,anxiety, panic attacks, insomnia, and irritability.Monitoring patients for these symptoms is recommended, along with social support for cessation of smoking.
Several nicotine receptor partial agonists are used for smoking cessation. These stimulate nicotine receptors and help to reduce the craving. Only varenicline is approved by the FDA in the United States.It is a pill available by a prescription. Varenicline should not be used with other quit smoking products.Common side effects include nausea and insomnia but serious behavioral side effects have also been observed. Varenicline received a black box warning in 2009 because of side effects including agitation,depression, and suicidality [28].
Clinical Approaches
Clinicians have many opportunitiesto advocate smoking cessation. The hospital, where nonsmoking is mandated, can be a good place to begin the cessation program. An acute illness such as myocardial infarction may provide that unique opportunity. A recent Cochrane review of interventions for smoking cessation in hospitalized patients revealed a number of important observations [29]. High-intensity behavioral interventions beginning during the hospital stay and continuing for at least one month after discharge were successful in achieving smoking cessation. Other interventions with lower intensity have little effect. The addition of nicotine replacement therapy to counseling signi ficantly increased cessation rates compared with those achieved by counseling alone. No data were found to suggest that addition of bupropion or varenicline treatment to intensive counseling increases cessation rates over those achieved by counseling alone [29].
The outpatient clinic visit is also an opportunity to advocate smoking cessation. Many clinics ask about smoking and other behaviors along with allergies at every patient visit. The answer is usually the same,but this emphasizes the importance of smoking cessation to an individual’s health. It also provides an opportunity for the clinician to advocate smoking cessation and referral to cessation resources.
The overall strategy is as follows:
1. Tobacco dependence is a chronic disease that often requires repeated intervention and multiple attempts to quit. Effective treatments exist,however, that can signi ficantly increase rates of long-term abstinence.
2. It is essential that clinicians and health care delivery systems consistently identify and document tobacco use status and treat every tobacco user seen in a health care setting.
3. Tobacco dependence treatments are effective across a broad range of populations. Clinicians should encourage every patient willing to make a quit attempt to use the counseling treatments and medication recommended.
4. Brief tobacco dependence treatment is effective.Clinicians should offer every patient who uses tobacco treatments shown to be effective.
5. Individual, group, and telephone counseling are effective, and their effectiveness increases with treatment intensity. Two components of counseling are especially effective, and clinicians should use these when counseling patients making a quit attempt:
a. Practical counseling (problem solving/skills training)
b. Social support delivered as part of treatment 6. Numerous effective medications are available for tobacco dependence, and clinicians should encourage their use by all patients attempting to quit smoking – except when their use is medically contraindicated or with a specific population for which there is insufficient evidence of effectiveness (i.e. pregnant women,smokeless tobacco users, light smokers, and adolescents):
a. Seven first-line medications ( five nicotine
and two non-nicotine) reliably increase long
term smoking abstinence rates:
i. Bupropion
ii. Nicotine gum
iii. Nicotine inhaler
iv. Nicotine lozenge
v. Nicotine nasal spray
vi. Nicotine patch
vii. Varenicline
b. Clinicians also should consider the use of certain combinations of medications identified as effective.
7. Counseling and medication are effective when used by themselves for treating tobacco dependence. The combination of counseling and medication, however, is more effective than use of either alone. Thus clinicians should encourage all individuals attempting to quit smoking to use both counseling and medication.
8. Telephone quitline counseling is effective with diverse populations and has a broad reach. Therefore clinicians and health care delivery systems should both ensure patient access to quitlines and promote quitline use.
9. Tobacco dependence treatments are both clinically effective and highly cost-effective relative to interventions for other clinical disorders. Providing coverage for these treatments increases quit rates. Insurers and purchasers should ensure that all insurance plans include the counseling and medication identified as effective as covered bene fits.
Clinicians have greater success in achieving smoking cessation in patients than most believe. The five hints for smoking cessation counseling by physicians are as follows:
1. Ask: systematically identify all tobacco users at every visit.
2. Advise: strongly urge all smokers to quit.
3. Attempt: identify smokers willing to try to quit.
4. Assist: aid the patient in quitting.
5. Arrange: schedule follow-up contact.
The amount of time required to do this is minimal and the potential for health improvement great [30].
Conclusions
Tobacco smoking is causally related to cardiovascular disease. Nearly a half million deaths annually are attributed to tobacco smoking in the United States. The economic cost, medical expenses, and indirect costs are enormous. The human cost in suffering exceeds the economic costs. Environmental smoke as inhaled as secondhand smoke is also an important cause of up to 40,000 deaths annually from cardiovascular disease. For adults, behavioral treatments, self-help approaches, and pharmacologic therapy are readily available. These measures, in combination with regulatory, community, and public health approaches, provide the potential for eliminating use of tobacco, one of the greatest health-impairing behaviors affecting humans.
Conflict of Interest
The author declare no Conflict of interest.
REFERENCES
1. World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009.
2. Centers for Disease Control and Prevention, Of fice on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion. http://www.cdc.gov/tobacco/data_statistics/fact_sheets/ [accessed 2016 June 17].
3. Jamal A, Homa DM, O’Connor E, Babb SD, Caraballo RS, Singh T, et al. Current cigarette smoking among adults – United States,2005–2014. MMWR Morb Mortal Wkly Rep 2015;64:1233–40.[accessed 2016 June 4].
4. US Department of Health and Human Services. Preventing tobacco use among youth and young adults: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion,Of fice on Smoking and Health;2012.
5. US Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. Atlanta,GA: US Department of Health and Human Services, Centers for Disease Control and Prevention,Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Of fice on Smoking and Health; 2006.
6. Filion KB, Luepker RV. Cigarette smoking and cardiovascular disease: lessons from Framingham.Global Heart 2013;8:35–41.
7. US Department of Health and Human Services. The health consequences of smoking: cardiovascular disease: a report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service,Of fice on Smoking and Health,DHHS publication no. (PHS)84-50204; 1983.
8. National Cancer Institute. Smoking and tobacco control monograph 8.Bethesda, MD: U.S. Department of Health and Human Services,National Institutes of Health,National Cancer Institute. Changes in cigarette-related disease risks and their implication for prevention and control. NIH publication no. 97-4213; 1997.
9. US Department of Health and Human Services. The health bene fits of smoking cessation: a report of the Surgeon General. Rockville,MD: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Of fice on Smoking and Health. DHHS publication no.(CDC) 90-8416; 1990.
10. Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease: overall findings and differences by age for 316,099 white men. Arch Intern Med 1992;152:56–64.
11. The Multiple Risk Factor Intervention Trial Research Group.Mortality after 16 years for participants randomized to the multiple risk factor intervention trial.Circulation 1996;94:946–51.
12. Hermanson B, Omenn GS, Kronmal RA, Gersh BJ. Bene ficial six-year outcome of smoking cessation in older men and women with coronary artery disease: results from the CASS registry. N Engl J Med 1988;319:1365–9.
13. Pooling Project Research Group.Relationship of blood pressure,serum cholesterol, smoking habit,relative weight, and-ECG abnormalities to incidence of major coronary events: final report of the Pooling Project. J Chronic Dis 1978;31:201–306.
14. Suarez L, Barrett-Connor E.Interaction between cigarette smoking and diabetes mellitus in the prediction of death attributed to cardiovascular disease. Am J Epidemiol 1984;120:670–5.
15. Benowitz NL. Cigarette smoking and cardiovascular disease: pathophysiology and implications for treatment. Prog Cardiovasc Dis 2003;46:91–111.
16. US Department of Health and Human Services. How tobacco smoke causes disease: the biology and behavioral basis for smokingattributable disease: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion,Of fice on Smoking and Health;2010.
17. Institute of Medicine. Secondhand smoke exposure and cardiovascular effects: making sense of the evidence. Washington, DC: The National Academy of Sciences,Institute of Medicine; 2009.[accessed 2016 June 6].
18. Wells AH. Heart disease from passive smoking in the workplace. J Am Coll Cardiol 1998;31:1–9.
19. Malarcher A, Dube S, Shaw L,Babb S, Kaufmann R. Quitting smoking among adults – United States, 2001–2010. MMWR Morb Mortal Wkly Rep 2011;60:1513–9.
20. National Center for Health Statistics. Health, United States,2015: with special feature on racial and ethnic health disparities.Hyattsville, MD. 2016. Available from: http://www.cdc.gov/nchs/data/hus/hus15.pdf [accessed 2016 June 6].
21. Mozaffarian D, Benjamin EJ,Go AS, Arnett DK, Blaha MJ,Cushman M, et al. Heart disease and stroke statistics – 2016 update: a report from the American Heart Association. Circulation 2016;134:e38–360. doi:10.1161/CIR.0000000000000350. Epub 2015 Dec 16.
22. Singh T, Arrazola RA, Corey CG,Husten CG, Neff LJ, Homa DM,et al. Tobacco use among middle and high school students – United States, 2011-2015. MMWR Morb Mortal Wkly Rep 2016;65:361–7.
23. US Department of Health and Human Services. Extending authorities to all tobacco products, including e-cigarettes, cigars and hookah. US Food and Drug Administration, Protecting and Promoting Your Health. http://www.fda.gov/TobaccoProducts/Labeling/RulesRegulationsGuidance/ucm388395.htm [accessed 2016 June 15].
24. Lavinghouze SR, Malarcher A, Jama A, Neff L, Debrot K, Whalen L.Trends in quit attempts among adult cigarette smokers – United States,2001–2013. MMWR Morb Mortal Wkly Rep 2015;64:1129–35.
25. Benowitz NL. Nicotine addiction.N Engl J Med 2010;362:2295–303.
26. Stead LF, Perera R, Bullen C,Mant D, Hartmann-Boyce J,Cahill K, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2012;11:CD000146.doi:10.1002/14651858.CD000146.pub4.
27. Hurt RD, Sachs DPL, Glover ED,Offord KP, Johnston JA, Dale LC,et al. A comparison of sustainedrelease buproprion and placebo for smoking cessation. N Engl J Med 1997;337:1195–202.
28. Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 2012;4:CD006103.doi:10.1002/14651858.CD006103.pub6.
29. Rigotti NA, Clair C, Munafò MR, Stead LF. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst Rev 2012;16:CD001837. doi:10.1002/14651858.CD001837.pub3.
30. Fiore MC, Jaén CR, Baker TB,Bailey WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD:US Department of Health and Human Services. Public Health Service; 2008.
 Cardiovascular Innovations and Applications2016年3期
Cardiovascular Innovations and Applications2016年3期
- Cardiovascular Innovations and Applications的其它文章
- Outcome Trials in the Therapeutic Management of Hypertension in East Asians
- In flammasomes and Atherosclerosis
- The Gut Microbiota and Atherosclerosis:The State of the Art and Novel Perspectives
- Psychosocial Risk Factors and Cardiovascular Disease: Epidemiology, Screening, and Treatment Considerations
- Management of Hypertension: JNC 8 and Beyond
- ACC/AHA Guidelines for Cardiovascular Disease Prevention and Cholesterol Management:Implications of New Therapeutic Agentsa
