Do Modern Imaging Studies Trump Cardiovascular Physical Exam in Cardiac Patients?
C. Richard Conti, MD, MACC
When many older (seasoned) physicians trained,modern cardiovascular imaging e.g. cardiac ultrasound, nuclear studies, computed tomography,cardiac MR did not exist. Non-invasive imaging studies that were available to us included the ECG,stress exercise testing, and chest X-ray. Invasive studies such as hemodynamics and angiography were the only physiologic and anatomic studies available. Thus there were very few imaging studies used for clinical decision making to con firm the diagnosis, estimate prognosis, or plan therapy of the cardiac condition. The best of these was cardiac catheterization with ventricular and coronary angiography in adult patients and measurement of intracardiac pressure, oximetry and angiography in patients with congenital heart disease. This is still the case in 2016 with many more images added.
Modern clinical decision making depends heavily on modern cardiovascular imaging. Most physicians think of the cardiovascular exam as auscultation of murmurs and heart sounds. This is not the case. If we had to rely on the cardiovascular exam including auscultation to make decisions in complex cardiac cases we would not be precise and accurate in many instances.
I thought it might be useful to assess the role of imaging in several different types of patient conditions that are properly evaluated after being admitted to hospital or seen in the clinic. Table 1 summarizes several cardiac conditions that are seen by physicians.
What follows are several cardiac conditions that are often seen by physicians:
1.ST elevation myocardial infarction.Here the history including the family history is important.Cardiovascular auscultation rarely adds anything to make the diagnosis. Blood pressure, palpation and observation are important. Laboratory studies e.g. Troponin T is usually positive and abnormalities seen on the ECG include ST segment elevation, or the STEMI equivalent new onset of LBBB. The chest X-ray usually adds nothing unless pulmonary edema is present. The CT may or may not add something such as pleural effusions, ventricular dilation etc. Cardiac MR may detect LV thrombus, show evidence of regional LV dysfunction and ventricular wall abnormalities e.g. subendocardial to transmural Ischemic zones. Cardiac ultrasound can detect regional wall motion abnormalities and LV thrombus.Catheter based, coronary angiography is the key image and con firms the diagnosis of vessel occlusion and direct appropriate therapy.
2.Non-ST elevation myocardial infarction.The history is quite important including the family history. Cardiovascular examination adds next to nothing. Laboratory tests are abnormal, e.g. troponin. The electrocardiogram may show evidence of myocardial ischemia such as T-wave inversion, ST segment depression or arrhythmias, etc. The chest X-ray shows nothing in most instances. CT chest, in some instances may reveal a pleural effusion or ventricular dilation and may detect LV thrombus. Cardiac MR can reveal evidence of regional LV dysfunction and ventricular wall abnormalies e.g.sub endocardial ischemia. The cardiac echo, in many instances, reveals regional LV dysfunction. Coronary angiography con firms the presence of high grade coronary artery stenosis as the probable cause of the myocardial infarction.
3.Unstable angina.The history, including the family history is important. Cardiovascular auscultation adds next to nothing. Laboratory tests(TrT) are usually normal. ECG may reveal ST segment depression, especially during chest discomfort. The chest X-ray generally shows nothing. CT chest may not reveal any abnormalities.Cardiac MR can reveal a regional wall motion abnormality as can cardiac ultrasound. Coronary angiography con firms the presence of high grade coronary artery stenoses.
4.Valvular heart disease.The history may be important; for example, in patients who have had acute rheumatic fever, mitral stenosis or some other valvular heart disease might be suspected,but many patients with proven Mitral stenosis,have no recollection of acute rheumatic fever as a child. Patients who have had an aortic systolic or diastolic murmur since birth, may have a bicuspid aortic valve. The presence of a tricuspid diastolic flow murmur across a normal tricuspid valve or a systolic flow murmur across a normal pulmonary valve are findings consistent with an atrial septal defect. Cardiac auscultation is usually positive in patients with valvular heart disease, particularly if the murmur is harsh and loud, i.e., systolic ejection murmur of aortic stenosis, or harsh holosystolic murmur of mitral regurgitation. In the USA, mitral stenosis is not as common as it is in developing countries, therefore medical students and young doctors trained in the USA are not as familiar with the physical findings of mitral stenosis as are those trained in developing countries.The laboratory studies are usually normal but in the case of rheumatic mitral stenosis may be abnormal,e.g. anti-streptolysin O, (ASLO titers). The ECG may be abnormal, e.g, in mitral stenosis patients,P Mitrale may be seen in lead ll as well as a negative P-V1. Atrial fibrillation is a common finding.The chest X-ray may be abnormal, depending on whether or not there is pulmonary congestion,calci fied valves or abnormal cardiac silhouettes.Chest CT ampli fies the chest X-ray findings.Cardiac MR may also be revealing since it will show evidence of valvular disease manifested by abnormal flow characteristics across the valve.Cardiac echo also generally exhibits anatomic valve abnormalities and Doppler echo reveals abnormal flow across the valve. Right and left heart catheterization con firms the cardiac pressures and gradients across AV and semilunar valves.
5.Systolic heart failure.History is important. Cardiac auscultation may in some instance, reveal an S3, diminished heart sounds, mitral regurgitation,but in many cases, nothing specific is heard. Laboratory studies are usually normal, ECG may reveal arrhythmias e.g. VT, AF, SVT, PVC’s but usually nothing specific, chest X-Ray may reveal pulmonary congestion, as will CT chest. CMRcan assess LV size, LV wall abnormalities i.e.myocarditis, sarcoid, amyloid, in filtrative diseases of the myocardium, mitral regurgitation,ventricular thrombus etc. Cardiac ultrasound can easily detect abnormalities of ventricular volume and function, mitral regurgitation and ventricular clot. Coronary angiography can exclude epicardial coronary stenoses as the cause of LV failure.
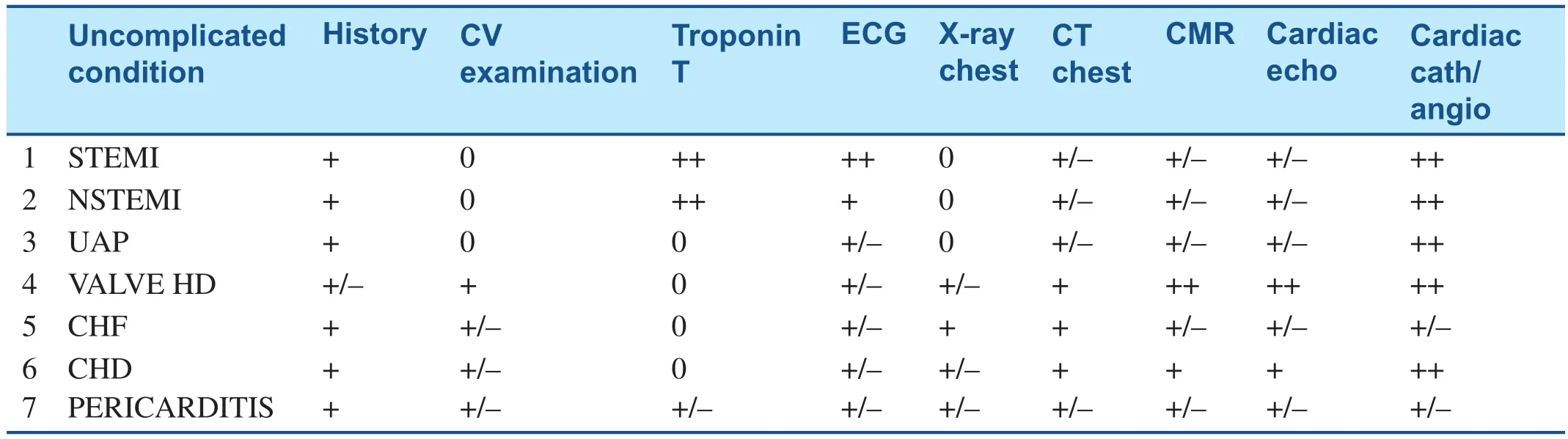
Table 1. Schematic to Illustrate Seven Cardiac Conditions and the Usefulness of Modern Imaging vs. Cardiac Examination in Arriving at the Correct Diagnosis. See Text for Details.
6.Congenital heart disease.History, including family history is important, since obviously the adult with congenital heart disease or the patient’s family will have known they had some heart disease at birth. The presence or absence of cyanosis is an important observation. In general, most of these patients have undergone cardiac surgery as a child and the operative note is an important piece of information revealing the original diagnosis. Cardiac auscultation usually reveals some murmur or abnormal heart sound but can be nondescript and not direct the examiner towards the correct diagnosis. Cardiovascular laboratory studies are generally not abnormal. ECG usually is abnormal but may not be diagnostic, e.g. RBBB,RAD etc. The chest X-ray usually is abnormal but may not be indicative of a specific cardiac disease. An example of an abnormal chest X-ray is seen in the patient who has a significant L to R shunt due to an ASD. The chest X-ray may show increased pulmonary blood flow in the lungs. In another example, there may be an X-ray silhouette suggesting coarctation of the aorta. The CT chest often con firms what was found on the chest X-ray and may also show abnormal silhouettes representing abnormal position of the great arteries. Cardiac MR is generally abnormal in that it will show aberrations such as ventricular inversion, valvular heart disease, abnormal blood flow in the great vessels, distention or lack of distention of neck veins and pulmonary veins. Cardiac ultrasound when performed by someone knowledgeable in the area of congenital heart disease can also detect anatomic and physiologic abnormalities in these patients. Only cardiac catheterization can determine intra cardiac pressures and oxygen saturations which may be key to decision making about diagnosis and therapy.
7.Pericarditis.History is important. Cardiac auscultation may or may not reveal a pericardial friction rub. Troponin T can be abnormal because of epi-myocarditis. ECG can be abnormal (generalized ST segment elevation) or normal. Chest X-ray generally is normal but at times can show enlarge cardiac silhouette (due to pericardial effusion). Chest CT can con firm pericardial effusion if present. Cardiac MR can do likewise. Cardiac echo can also con firm pericardial effusion if present. Coronary angiography can eliminate high grade coronary artery stenoses as the cause of ST segment elevation on the ECG and right heart catheterization can determine pressures consistent with cardiac tamponade if present.
SUMMARY
In summary, on the basis of all these examples, I do believe that modern imaging studies trump cardiovascular examination in most cardiac patients. But I do want to add the caveat that I do not think we should give up on cardiovascular physical examination, since physical examination does not just mean cardiac auscultation. It includes blood pressure, heart rate and rhythm measurement; Inspection, i.e. assessing the condition of the patient (stable, unstable), the presence of absence of cyanosis or other abnormalities, including the neck and peripheral veins; Palpation, feeling for abnormalities in the carotid arteries, assessing a parasternal lift, assessing abnormalities of the apical impulse and the abdominal aorta and peripheral arteries. In addition, the cardiovascular physical examination combined with the history directs the physician to perform many of the imaging modalities that are available to the modern cardiologist to con firm the cardiac diagnosis, estimate prognosis and direct therapeutic strategies. In my opinion, history and cardiac ultrasound seem to be the simplest and most useful ways to evaluate cardiac patients with symptoms related to heart failure.The ECG is best and simplest for arrhythmias. Catheter based coronary angiography, stress nuclear and stress echo studies are best for ischemic heart disease symptoms. But hard decision making in the individual patient is a combination of history, physical exam, and most importantly, laboratory abnormalities and modern imaging including the old standby,cardiac catheterization and angiography.
 Cardiovascular Innovations and Applications2016年4期
Cardiovascular Innovations and Applications2016年4期
- Cardiovascular Innovations and Applications的其它文章
- Fractional Flow Reserve Measurement by Coronary Computed Tomography Angiography:A Review with Future Directions
- Novel Approaches for the Use of Cardiac/ Coronary Computed Tomography Angiography
- Coronary Calcium Scoring in 2017
- Magnetic Resonance Imaging of Coronary Arteries: Latest Technical Innovations and Clinical Experiences
- T1 and ECV Mapping in Myocardial Disease
- The Role of Clinical Cardiac Magnetic Resonance Imaging in China: Current Status and the Future
