Coronary Calcium Scoring in 2017
Kazuhiro Osawa, MD, Rine Nakanishi, MD and Matthew Budoff, MD
Introduction
Coronary artery calci fication (CAC) is a strong predictor of coronary heart disease (CHD) and a wellvalidated risk strati fication tool [1–3]. CAC can occur in the advanced process of atherosclerosis and re flects a linear estimate of the total plaque burden of coronary artery atherosclerosis. The presence of greater CAC is associated with increasingly higher risk of adverse cardiovascular events and all-cause death [1, 2, 4, 5] and thus patients with excessive CAC should be considered as high-risk patients,whereas a CAC score of zero is associated with a very low event rate [6]. CAC assessment in asymptomatic adults was incorporated in the American College of Cardiology Foundation/American Heart Association(AHA) guidelines with class IIa, level of evidence B status in 2010 and was recommended for patient risk assessment in asymptomatic adults at intermediate risk and for all patients older than 40 years with diabetes mellitus [7]. Clinically, the importance and use of CAC assessment has been increasing significantly.Not only the CAC score itself but also the CAC score in addition to traditional risk factors increases the diagnostic accuracy of the cardiovascular risk,especially in the asymptomatic population. One of the major areas of progress of research on CAC is more than 10 years of follow-up studies, which have been recently reported by several investigators. It is important for clinicians to know that the CAC score can provide a predictive value of coronary atherosclerosis and it could give us the long-term prognosis of individuals. In this review, we describe the key data supporting the use of CAC assessment based on publications from the past few years.
The Power of CAC in Risk Strati fication
Can we predict the patient’s cardiovascular events in advance? If we can do so, the number of patients with fatal cardiovascular disease (CVD) could decrease.The Framingham risk score (FRS) or the new atherosclerotic CVD (ASCVD) risk score of the American College of Cardiology (ACC)/AHA has to date been used as an established risk scoring method for primary prevention based on conventional risk factors for cardiovascular events in asymptomatic individuals. The FRS predicted the 10-year cardiovascular risk of individuals and categorized individual risk of developing CVD as low (10-year risk of less than 10%), intermediate (10-year risk of 10–20%) and high (10-year risk of more than 20%) [8]. Although the FRS is an important advance in the primary prevention of CVD, the risk strati fication algorism is not perfect [9–11]. The limitations of the FRS include a substantial underestimation of lifetime risk (especially in women), misclassi fication of high-risk individuals as low-risk or intermediate-risk individuals,and misclassi fication of very low risk individuals into a higher risk stratum [10]. In a contemporary novel study of more than 307,000 participants, the new pooled cohort equation (ASCVD risk score) showed gross overestimation of risk, so virtually every group is fourfold less likely to experience an event than anticipated. This leads to significant overtreatment,and can contribute to low adherence [12]. CAC scoring can improve the risk strati fication of CVD over the pooled cohort equation and the FRS (Figure 1A)[3, 13–16]. Recently, several studies have reported the incremental prognostic value of CAC over traditional risk factors after a long follow-up. Kelkar et al. [17] revealed that CAC could effectively identify high-risk women with low to intermediate FRS and improve risk detection algorisms based on traditional risk factors (net reclassi fication improvement of CAC 0.155, P=0.002). Hoffmann et al. [18]demonstrated that CAC improved discrimination and risk reclassi fication for CHD and CVD beyond traditional risk factors in an asymptomatic population in the Framingham Offspring Study. They found that addition of log CAC to the FRS significantly increased the discriminatory ability for major CHD over 8 years of follow-up (c-statistic for FRS alone 0.78 vs. 0.82 for FRS + log CAC, P<0.05) and CAC could reclassify more than half of the participants at intermediate 10-year risk of major CHD based on the FRS as having low risk (observed event rate 0%) or high risk (observed event rate 8%) [18].Yeboah et al. [16] found that CAC in addition to the FRS provided superior discrimination especially in intermediate-risk individuals after 9 years of followup as opposed to thoracic aorta calcium, aortic valve calci fication, mitral annular calci fication, pericardial adipose tissue volume, or liver attenuation in addition to the FRS for incident CHD/CVD, and moreover,afforded the greatest decrease in the area under the curve (AUC) for detecting incident CHD as 0.712,0.645, 0.651, 0.643, 0.643 and 0.641 respectively.McClelland et al. [19] reported a novel risk score to estimate 10-year CHD risk using CAC and traditional risk factors based on the Multi-Ethic Study of Atherosclerosis (MESA) data with validation in the Heinz Nixdorf Recall (HNR) study and the Dallas Heart Study (DHS). They demonstrated that CAC in addition to traditional risk factors could improve the risk prediction compared with traditional risk factors alone (c-statistic 0.80 vs. 0.75, P<0.0001). External validation in both the HNR study and the DHS provided evidence of very good discrimination and calibration, and Harrell’s c-statistic was 0.779 in the HNR study and 0.816 in the DHS [19]. Moreover,Blaha et al. [20] reported the clinical implication of the location and distribution pattern of CAC in addition to the CAC score for the prediction of CHD/CVD events. They revealed that addition of the number of vessels with CAC significantly improved the capability to predict CHD and CVD events in survival analysis (hazard ratio [HR] 1.9–3.5 for four-vessel CAC vs. one-vessel CAC), AUC analysis (c-statistic improvement of 0.01–0.033), and net reclassi fication improvement analysis (categoryless net reclassi fication improvement of 0.10–0.45) [20].
These studies and others demonstrate that we can predict patient’s cardiovascular events robustly if we use the CAC score for patient risk strati fication. At present, the CAC score in addition to traditional risk factors is the best method for patient risk strati fication and risk prediction for CHD and CVD. The new ACC/AHA prevention guidelines state “assessing CAC is likely to be the most useful of the current approaches to improving risk assessment among individuals found to be at intermediate risk after formal risk assessment” [21].
CAC Score Greater than Zero Equals Increased Risk of Atherosclerosis
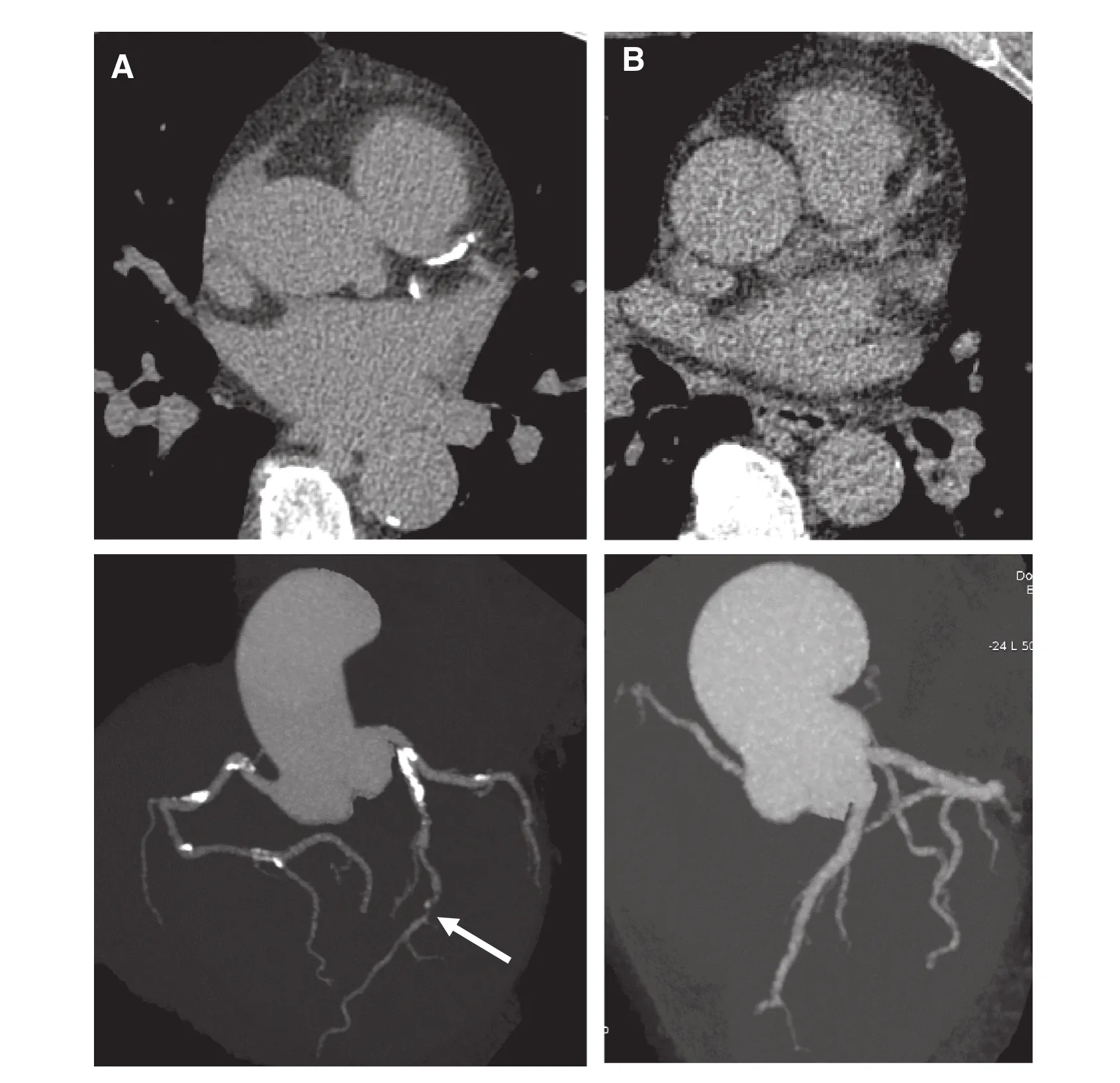
Figure 1 Examples of the Utility of CAC Scoring in Patient’s Risk Assessment.(A) A 60-year-old Caucasian woman. She had a history of hypertension and dyslipidemia without antihypertensive drugs and antidyslipidemia drugs. The total cholesterol level was 248 mg/dL and the high-density lipoprotein (HDL) cholesterol level was 44 mg/dL. The systolic blood pressure was 150 mmHg. The coronary artery calci fication (CAC) score was 867. CAC could be detected in all three vessels. The left anterior descending artery showed significant stenosis (white arrows). The estimated 10-year coronary heart disease (CHD) event risk for this patient with this risk factor pro file including CAC was 17.8%.The estimated 10-year risk of having a CHD event for this patient without inclusion of CAC would be 6.3%. (B) A 62-year-old African American man. He had a history of hypertension and dyslipidemia with antihypertensive drugs and antidyslipidemia drugs. He also had a family history of myocardial infarction. The total cholesterol level was 179 mg/dL and the HDL cholesterol level was 54 mg/dL. The systolic blood pressure was 136 mmHg. The CAC score was zero. There was no CAC in all three vessels. The estimated 10-year CHD event risk for this patient with this risk factor pro file including CAC was 4.2%. The estimated 10-year risk of having a CHD event for this patient without inclusion of CAC would be 11.0%.
A CAC score greater than zero indicates a greater risk of coronary artery disease (CAD) and CHD. As the CAC score increases, the risk of CAD and CHD increases [1, 22–24]. Long term follow-up data of more than 10 years in terms of CAC have recently been validated in multiple studies, demonstrating the significant association between increased CAC and higher incidence of outcomes among a population-based cohort [19, 25, 26], the general population [27], the elderly [27], women [17,27], and in individuals with low risk factors [17,28] and diabetes [29] or family history [30]. Shaw et al. [25] reported the ability of CAC to predict long-term mortality in 9715 asymptomatic patients.They revealed that overall mortality was 3, 6, 9, 14,21 and 28% respectively for CAC subgroups with scores of 0, 1–10, 11–100, 101–399, 400–999, and 1000 or greater (P<0.001) at a mean follow-up of 14.6 years and the CAC score was highly predictive of all-cause death in Cox models after adjustment for CAD risk factors (P<0.001) [25]. Valenti et al.[26] reported that a CAC score greater than zero was the strongest predictor of death beyond cardiovascular risk factors, the FRS and the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) score, and was independently associated with nearly threefold risk of death(HR 2.67, 95% con fidence interval [CI] 2.29–3.11).Compared with the base models of the FRS or the NCEP ATP III score alone, discrimination improved significantly when CAC score greater than zero was added to the FRS or the NCEP ATP score III (AUC 0.64 vs. 0.71 and 0.64 vs. 0.72 for the FRS and the NCEP ATP III score respectively; P<0.001 for both) [26]. Among 13,092 asymptomatic individuals undergoing CAC scan, our group demonstrated that CAC was strongly associated with risk of dea th during a median follow-up of 11 years in young and middle-aged groups, in both men and women,while the risk predictive value of CAC was slightly reduced in older individuals [27]. We reported that in 5584 asymptomatic and very low CVD risk individuals, mortality increased according to increasing CAC scores of 1–99 (HR 1.9, 95% CI 1.2–3.1),100–399 (HR 2.1, 95% CI 1.2–3.6) and 400 or greater (HR 2.8, 95% CI 1.6–4.8) compared with that in patients with a CAC score of zero during a mean follow-up of 10.4 years [28]. In MESA, we also reported that a CAC score greater than zero was a strong and graded predictor of incident ASCVD at a median follow-up of 10.2 years [31]. In comparison to a CAC score of zero, CAC 1-100 (HR 2.1,95% CI 1.6–2.6), 101-300 (HR 3.1, 95% CI 2.4–4.0) and more than 300 (HR 4.5, 95% CI 3.5–5.8)were all predictive of ASCVD events at 10 years[32]. Moreover, in a meta-analysis, Bavishi et al.[33] revealed a significant relationship between the magnitude of CAC and stress-induced myocardial ischemia. They showed a stepwise increase in the frequency of ischemia according to CAC abnormality. The average frequency of myocardial ischemia was 6.6% among individuals with a CAC score of zero and 23.6% among those with a CAC score of 400 or greater. However, there was a wide variance in the frequency of ischemia ranging from 0 to 24.1% among patients with a CAC score of zero,and ranging from 12.4 to 57.1% among patients with a CAC score of 400 or greater. Compared with those with a CAC score of zero, the pooled odds ratio (OR) for myocardial ischemia increased substantially for each increasing category of CAC abnormality: OR 1.7 (95% CI 1.04–2.2) for a for CAC score of 1–100; OR 3.3 (95% CI 1.4–8.2) for a CAC score of 101–399; and OR 6.9 (95% CI 3.5–13.4) for a CAC score of 400 or greater [33].
What are the risk factors for progression of CAC?Studies [34–39] have revealed the association between CAC progression and risk factors such as greater age, male sex, Caucasian race, higher body mass index, history of hypertension, dyslipidemia,diabetes, and metabolic syndrome, being a smoker,and a family history of myocardial infarction. Two studies have recently reported the clinical importance of family history of CHD for predicting the incidence and progression of CAC in asymptomatic individuals [30, 40]. Mulders et al. [40] reported that individuals with a family history of premature CAD had an increased risk of increased CAC (OR 2.23, 95% CI 1.48–3.36; P<0.05) compared with those without a family history, and the event rate was also low in those without a family history after 3.5 years of follow-up. Knapper et al. [30] revealed the prognostic utility of CAC scoring among cohorts of young and older patients with and without a family history of CAD. For patients older than 60 years with a family history of CAD, there was a significant decrease in the AUC with CAC over CAD risk factors (AUC 0.539 vs. 0.725, P<0.001);however, a decrease was not seen among patients younger than 60 years with a family history of CAD(AUC 0.636 vs. 0.626, P=0.67) [30]. Furthermore,a study of the relationship between air pollution and CAC has been reported from MESA. Kaufman et al. [41] revealed that fine particulate matter less than 2.5 µm in diameter (PM2.5) and nitrogen oxides(NOx) were associated with progression of CAC in the 10-year prospective cohort study. After adjustment for potential confounders, CAC progressed by 4.1 Agatston units per year (95% CI 1.4–6.8 Agatston units per year) for each 5 µg PM2.5/m3increase and by 4.8 Agatston units per year (95%CI 0.9–8.7 Agatston units per year) for each 40-ppb NOxincrease.
It is important to recognize that while statin therapy may induce slight progression of CAC (thought to be by stabilizing plaque), significant CAC progression remains a major risk factor for cardiovascular events. In a large cohort of 4609 asymptomatic patients, after adjustment for baseline score, age,sex, and time between scans, CAC progression was associated with a 3.34-fold risk of all-cause death(HR 3.34, 95% CI 2.65–4.21, P<0.0001) [42]. This study observed graded relationships of CAC progression and CHD event risk, strongly suggesting that the functions are linear, with greater CAC progression associated with greater risk. MESA studied 6778 people who had baseline and follow-up CAC scans approximately 2.5 years apart [24]. The median follow-up duration from the baseline was 7.6 years (maximum 9.0 years). Among participants with baseline CAC, those with annual progression of more than 300 units had adjusted HRs of 3.8(1.5–9.6) for total CHD and 6.3 (1.9–21.5) for hard CHD compared with those without progression.This demonstrates that progression of CAC is associated with total and hard CHD risk; these relationships remained significant after adjustment for risk factors and baseline calcium level.
The Impact of Zero CAC Score
Nothing is more reassuring than a CAC score of zero for clinicians in patient risk strati fication. Clinical evidence of the association between a CAC score of zero and CHD has been reported. A clinical asymptomatic population with a CAC score of zero can be considered as having very low risk of CHD (Figure 1B) [1, 22, 43, 44]. Recently, the long-term prognostic value of a CAC score of zero for asymptomatic individuals has been described in several studies.Valenti et al. [26] reported that a CAC score of zero conferred a 15-year warranty period against death for individuals at low to intermediate risk by the FRS and the NCEP ATP III score that was unaffected by age and sex. A CAC score of zero showed the lowest mortality rates among the low-risk categories such as FRS less than 10%, NCEP ATP III score less than 10%, no cardiovascular risk, and a CAC score of zero.The risk of all-cause death was greater in individuals with a CAC score greater than zero plus a low FRS or a low NCEP ATP III score (CAC score greater than zero plus low FRS, HR 3.3, 95% CI 2.49–4.32;CAC score greater than zero plus low NCEP ATP III score, HR 3.09, 95% CI 2.45–3.90) compared with those with a CAC score of zero plus a high FRS or a high NCEP ATP III score (CAC score of zero plus high FRS, HR 2.8, 95% CI 2.05–3.92; CAC score of zero plus high NCEP ATP III score, HR 2.94, 95%CI 2.15–4.01). They demonstrated that a CAC score of zero was associated with a vascular age that was 30 years less than chronological age for older individuals and was associated with a significantly lower annual mortality rate than for the equivalent chronological age category [26]. Similarly, our group demonstrated that the risk of death in patients without evidence of CAC was significantly lower compared with that in the general US population across various age groups regardless of sex [27]. A CAC score of zero was shown to be a stronger negative risk predictor for all CAD and CVD events after a mean followup of 10.3 years among negative atherosclerotic risk factors such as carotid intima-media thickness less than the 25th percentile, absence of carotid plaque,brachial flow-mediated dilation change of more than 5% change, ankle-brachial index greater than 0.9 and less than 1.3, high-sensitivity C-reactive protein level less than 2 mg/L, homocysteine level less than 10 µmol/L, N-terminal pro-brain natriuretic peptide level less than 100 pg/mL, no microalbuminuria, no family history of CHD (any/premature), absence of metabolic syndrome, and a healthy lifestyle [45]. A CAC score of zero resulted in the greatest reduction in posttest risk among all negative risk markers and had stable risk factor–adjusted diagnostic likelihood ratios across adverse clinical situations: 0.36 (SD,0.09) in men and 0.46 (SD, 0.12) in women for CHD events; 0.49 (SD, 0.10) in men and 0.59 (SD, 0.12) in women for CVD events [45].
In contrast, a CAC score of zero does not always guarantee the long-term lowest mortality rate in individuals with diabetes mellitus [29]. Among 9715 asymptomatic individuals, including 810 diabetic individuals, the rate of all-cause death was similarly low between diabetic and nondiabetic individuals with a CAC score of zero during the initial 5 years(2.6 vs. 1.2%, P=0.06). However, at 15 years of follow-up, the concomitant existence of diabetes and a CAC score of zero was associated with an almost 2.5-fold increased risk of death compared with no diabetes with a CAC score of zero [29]. New recommendations from the ACC suggest CAC assessment in the setting of asymptomatic individuals with diabetes, as this affords the best risk strati fication of the current assessment tools [46].
As described, a CAC score of zero implies the lowest risk of cardiovascular events, especially in nondiabetic individuals, for extended periods.Consequently, how can we maintain a CAC score of zero? In MESA, the proportion with a persistent CAC score of zero was examined during the median 9.6 years of follow-up in 1850 individuals with a CAC score of zero at the baseline. Participants with a CAC score of zero were significantly likelier to be younger, be female, and have fewer traditional risk factors; meanwhile, there was no single risk factor or specific low-risk factor phenotype that markedly improved the discrimination of a persistent CAC score of zero over demographic variables. A CAC score of zero may be predominantly in fluenced by the long-term maintenance of low risk factors for CVD or genetic factors rather than the absence of any specific risk factors in late adulthood [47].Furthermore, as might be expected, unhealthy lifestyle habits could be a major contributor to CAC[48]. A combination of regular exercise, healthy diet, avoidance of smoking, and weight maintenance was associated with lower coronary calcium incidence, slower calci fication progression, and lower all-cause mortality over 7.6 years [49]. As a specific solution, Imran et al. [50] recommended daily walking. They reported the inverse association between physical activity and CAC. The more than 15 to 22.5 metabolic equivalent hours per week group had a 46% lower prevalence of CAC compared with the reference group (<3.75 metabolic equivalent hours per week) after adjustment for age,sex, race, smoking, alcohol use, total physical activity, and familial clustering [50]. Habitual physical activity can prevent the development of CAD. Daily healthy food choices could also have a great impact on arterial health. Miedema et al. [51] reported that higher intake of fruit and vegetables during young adulthood was associated with lower odds of prevalent CAC after 20 years of follow-up. Spring et al.[52] reported that healthy lifestyle change during young age (18–30 years old) could be associated with decreased odds of detectable CAC and lower intima-media thickness in middle age.
The Utility of the CAC Score for Patient Treatment
In 2013 the ACC/AHA released updated CVD prevention guidelines [21, 53]. These guidelines changed the outcome from CHD to ASCVD including stroke.Moreover, the guidelines moved away from LDL cholesterol level and instead recommended a statin for individuals with a 10-year ASCVD risk of greater than 7.5%, which was lower than the former threshold, and the numbers of individuals eligible for statin therapy increased greatly. With the new guidelines,it is clear that a lot of future ASCVD events could be prevented; however, there could potentially be overestimation of patients at lower ASCVD risk[54–56]. DeFilippis et al. [55] showed the discriminative capability of the new 2013 guidelines in 4227 MESA participants aged 50–74 years and without diabetes at the baseline. They revealed the new guidelines overestimated cardiovascular events (predicted events 9.16% vs observed events 5.16%) and 78% discordance. Discordance between observed and expected risk was found throughout the risk continuum, including those at moderate risk. In men with an ASCVD risk score of 7.5–10%, the actual event rate was only 3.0% (predicted events 8.7%vs observed events 3.0%). Among women with an ASCVD risk score of 7.5–10%, the actual event rate was only 5.1% (predicted events 8.7% vs. observed events 5.1%) [55]. It is easy to image that risk overestimation could lead to increased use of preventive medications such as statin therapy, potentially exposing some patients to the unnecessary risks of these drugs and result in greater health care costs. Nasir et al. [56] evaluated the utility of the CAC score in reclassifying ASCVD populations by each risk stratum in which statins were recommended according to the guidelines in 4758 MESA participants.According to the guidelines, 2377 participants were recommended for moderate-intensity to high-intensity statin therapy. However, 41% of the 2377 participants had a CAC score of zero, with only 5.2 events per 1000 person-years. Among 589 participants considered for moderate-intensity statin, 338 (57%) had a CAC score of zero, with an ASCVD event rate of only 1.5 per 1000 person-years. From these results,almost 50% of the patients recommended for statin treatment had low event rates and actually had low risk (<7.5% 10-year risk). Thus a CAC score of zero could reclassify approximately half of candidates as not eligible for statin therapy [56].
A concern about CAC scoring is that it might lead to increased unnecessary downstream testing and intervention and increased health care costs for the public [57]. In the Early Identi fication of Subclinical Atherosclerosis by Noninvasive Imaging Research(EISNER) study [31], the rates of additional cardiovascular testing, invasive coronary angiography,and coronary revascularization were higher in participants with severely elevated CAC scores; however, CAC scoring showed no significant increase of overall estimated health care expenditures because a minimal CAC score (CAC score less than 10) or a CAC score of zero was associated with significantly lower rates of subsequent cardiovascular testing and costs. Individuals with a CAC score of zero showed lower rates of initiation of new lipid-lowering medication, in contrast, a progressive increase in new lipid-lowering medications occurred with increasing baseline CAC scores, with 19, 35, 43 and 65%respectively for CAC subgroups with scores of 0,1–99, 100–399, and 400 or greater (P<0.001) [58].
In the 2013 guidelines, CAC scores of either greater than the 75th percentile for age and sex or 300 or greater were considered as high risk and warrant high-dose statin therapy. On the basis of studies from MESA, a CAC score of more than 100 was more predictive of events than a score greater than the 75th percentile, and indicates high cardiovascular risk, so we recommend use of a CAC score greater than 100 rather than either a CAC score of greater than 300 or greater than the 75th percentile [23]. Figure 2 shows our suggested flowchart for primary prevention of ASCVD. To summarize,individuals with a 10-year risk of 2.5–7.5% should be evaluated for the CAC score. If they have a CAC score greater than 100, they should be treated with statins as having a high risk of ASCVD. In addition,the CAC score may be promising for guiding aspirin use for the primary prevention of ASCVD. On the basis of an assessment of 4229 individuals from the MESA population without diabetes, Meiedema et al. have reported that individuals with a CAC score of 100 or greater had an estimated net treatment bene fit from aspirin, whereas individuals with a CAC score of zero were estimated to be two to four times likelier to experience a major bleed from aspirin use.
CAC can robustly identify individuals who could be bene fit from antiatherosclerotic therapies and aspirin and can also identify those who may not need treatment.
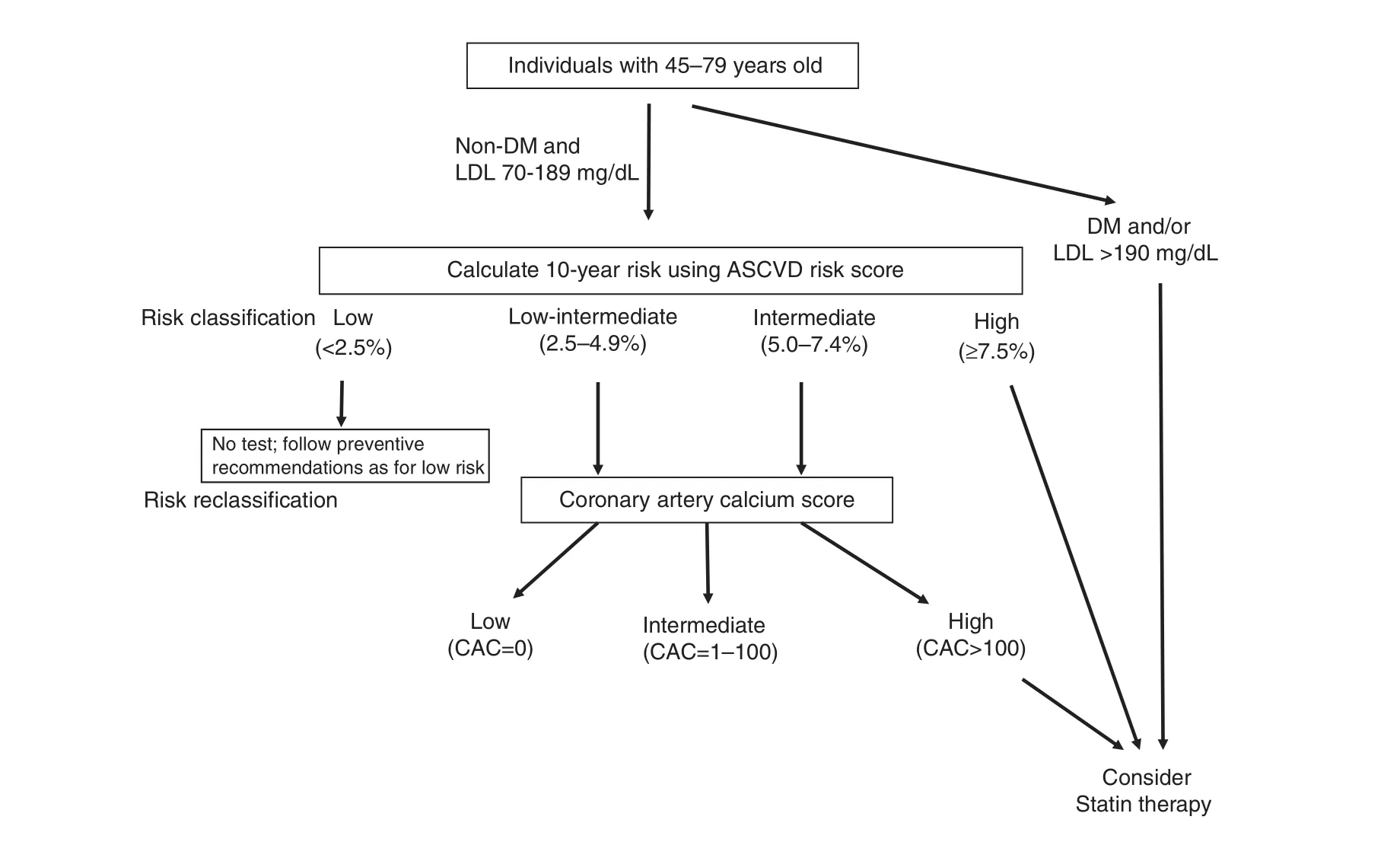
Figure 2 Summary of the Proposed Protocol for Including Coronary Artery Calci fication (CAC) Scores When Determining Atherosclerotic Cardiovascular Disease (ASCVD) Risk and Preventive Treatment. Individuals with Diabetes Mellitus (DM) or a Low-density Lipoprotein (LDL) Cholesterol Level of 190 mg/dL or Greater Should Be Treated with Statins.Nondiabetic individuals with LDL cholesterol levels of 70–189 mg/dL first need to be assessed for ASCVD risk, and a treatment strategy should be decided on according to risk strati fication.
Conclusion
In this review we have described the clinical signi fi-cance of CAC based on the current available data.In long-term follow-up studies, CAC in addition to traditional risk factors could adequately classify patients at risk compared with traditional risk factors alone. With increasing CAC scores, there is a greater likelihood of myocardial ischemia, and the risk of CVD events also increases significantly. In contrast,those with a CAC score of zero, especially without diabetes, could be considered as having very low risk with a 15-year warranty. For treatment, stratification according to the results of CAC scoring is robust to identify individuals who will bene fit from antiatherosclerotic and aspirin therapy. The clinical role of the CAC score has been solidi fied as part of our 2010 screening and 2013 cholesterol guidelines.The CAC score will be likely play an increasingly important role in health care management, especially among the preventive community.
Conflict of Interest
Matthew J Budoff has received research funds from NIH and GE Health Care. The other authors have no Conflict of interest.
REFERENCES
1. Detrano R, Guerci AD, Carr JJ,Bild DE, Burke G, Folsom AR,et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. New Engl J Med 2008;358:1336–45.
2. Polonsky TS, McClelland RL,Jorgensen NW, Bild DE, Burke GL, Guerci AD, et al. Coronary artery calcium score and risk classi fication for coronary heart disease prediction. JAMA 2010;303:1610–6.
3. Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA 2012;308:788–95.
4. Vliegenthart R, Oudkerk M,Hofman A, Oei HH, van Dijck W,van Rooij FJ, et al. Coronary calci fication improves cardiovascular risk prediction in the elderly.Circulation 2005;112:572–7.
5. Greenland P, LaBree L, Azen SP,Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals.JAMA 2004;291:210–5.
6. Sarwar A, Shaw LJ, Shapiro MD,Blankstein R, Hoffman U, Cury RC, et al. Diagnostic and prognostic value of absence of coronary artery calci fication. JACC Cardiovasc Imaging 2009;2:675–88.
7. Greenland P, Alpert JS, Beller GA,Benjamin EJ, Budoff MJ, Fayad ZA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2010;56:e50–103.
8. Grundy SM, Pasternak R,Greenland P, Smith S, Jr., Fuster V. Assessment of cardiovascular risk by use of multiple-riskfactor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation 1999;100:1481–92.
9. Akosah KO, Schaper A, Cogbill C,Schoenfeld P. Preventing myocardial infarction in the young adult in the first place: how do the National Cholesterol Education Panel III guidelines perform? J Am Coll Cardiol 2003;41:1475–9.
10. Michos ED, Nasir K, Braunstein JB, Rumberger JA, Budoff MJ,Post WS, et al. Framingham risk equation underestimates subclinical atherosclerosis risk in asymptomatic women. Atherosclerosis 2006;184:201–6.
11. Schlendorf KH, Nasir K, Blumenthal RS. Limitations of the Framingham risk score are now much clearer.Prev Med 2009;48:115–6.
12. Rana JS, Tabada GH, Solomon MD, Lo JC, Jaffe MG, Sung SH,et al. Accuracy of the atherosclerotic cardiovascular risk equation in a large contemporary, multiethnic population. J Am Coll Cardiol 2016;67:2118–30.
13. Elias-Smale SE, Proenca RV,Koller MT, Kavousi M, van Rooij FJ, Hunink MG, et al. Coronary calcium score improves classi fication of coronary heart disease risk in the elderly: the Rotterdam study. J Am Coll Cardiol 2010;56:1407–14.
14. Erbel R, Mohlenkamp S, Moebus S, Schmermund A, Lehmann N,Stang A, et al. Coronary risk stratification, discrimination, and reclassi fication improvement based on quanti fication of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol 2010;56:1397–406.
15. Kavousi M, Elias-Smale S, Rutten JH, Leening MJ, Vliegenthart R,Verwoert GC, et al. Evaluation of newer risk markers for coronary heart disease risk classi fication:a cohort study. Ann Intern Med 2012;156:438–44.
16. Yeboah J, Carr JJ, Terry JG, Ding J, Zeb I, Liu S, et al. Computed tomography-derived cardiovascular risk markers, incident cardiovascular events, and all-cause mortality in nondiabetics: the Multi-Ethnic Study of Atherosclerosis. Eur J Prev Cardiol 2014;21:1233–41.
17. Kelkar AA, Schultz WM, Khosa F,Schulman-Marcus J, O’Hartaigh BW,Gransar H, et al. Long-term prognosis after coronary artery calcium scoring among low-intermediate risk women and men. Circ Cardiovasc Imaging 2016;9:e003742.
18. Hoffmann U, Massaro JM,D’Agostino RB, Sr., Kathiresan S, Fox CS, O’Donnell CJ.Cardiovascular event prediction and risk reclassi fication by coronary, aortic, and valvular calci fication in the Framingham Heart Study.J Am Heart Assoc 2016;5:e003144.
19. McClelland RL, Jorgensen NW,Budoff M, Blaha MJ, Post WS,Kronmal RA, et al. 10-year coronary heart disease risk prediction using coronary artery calcium and traditional risk factors: derivation in the MESA (Multi-Ethnic Study of Atherosclerosis) with validation in the HNR (Heinz Nixdorf Recall) study and the DHS (Dallas Heart Study). J Am Coll Cardiol 2015;66:1643–53.
20. Blaha MJ, Budoff MJ, Tota-Maharaj R, Dardari ZA, Wong ND, Kronmal RA, et al. Improving the CAC score by addition of regional measures of calcium distribution: Multi-Ethnic Study of Atherosclerosis. JACC Cardiovasc Imaging 2016;9:1407–16.
21. Goff DC, Jr., Lloyd-Jones DM,Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2935–59.
22. Budoff MJ, McClelland RL, Nasir K, Greenland P, Kronmal RA,Kondos GT, et al. Cardiovascular events with absent or minimal coronary calci fication: the Multi-Ethnic Study of Atherosclerosis (MESA).Am Heart J 2009;158:554–61.
23. Budoff MJ, Nasir K, McClelland RL, Detrano R, Wong N,Blumenthal RS, et al. Coronary calcium predicts events better with absolute calcium scores than age-sex-race/ethnicity percentiles: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2009;53:345–52.
24. Budoff MJ, Young R, Lopez VA,Kronmal RA, Nasir K, Blumenthal RS, et al. Progression of coronary calcium and incident coronary heart disease events: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2013;61:1231–9.
25. Shaw LJ, Giambrone AE, Blaha MJ, Knapper JT, Berman DS,Bellam N, et al. Long-term prognosis after coronary artery calcification testing in asymptomatic patients: a cohort study. Ann Intern Med 2015;163:14–21.
26. Valenti V, Ó Hartaigh B, Heo R, Cho I, Schulman-Marcus J, Gransar H,et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: a prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging 2015;8:900–9.
27. Nakanishi R, Li D, Blaha MJ,Whelton SP, Darabian S, Flores FR,et al. All-cause mortality by age and gender based on coronary artery calcium scores. Eur Heart J Cardiovasc Imaging 2016;17:1305–14.
28. Nakanishi R, Li D, Blaha MJ,Whelton SP, Matsumoto S, Alani A, et al. The relationship between coronary artery calcium score and the long-term mortality among patients with minimal or absent coronary artery risk factors. Int J Cardiol 2015;185:275–81.
29. Valenti V, Hartaigh BO, Cho I,Schulman-Marcus J, Gransar H,Heo R, et al. Absence of coronary artery calcium identi fies asymptomatic diabetic individuals at low near-term but not long-term risk of mortality: a 15-year follow-up study of 9715 patients. Circ Cardiovasc Imaging 2016;9:e003528.
30. Knapper JT, Khosa F, Blaha MJ,Lebeis TA, Kay J, Sandesara PB,et al. Coronary calcium scoring for long-term mortality prediction in patients with and without a family history of coronary disease. Heart 2016;102:204–8.
31. Shaw LJ, Min JK, Budoff M, Gransar H, Rozanski A, Hayes SW, et al.Induced cardiovascular procedural costs and resource consumption patterns after coronary artery calcium screening: results from the EISNER(Early Identi fication of Subclinical Atherosclerosis by Noninvasive Imaging Research) study. J Am Coll Cardiol 2009;54:1258–67.
32. Budoff MJ, Young R, Burke G, et al.Coronary artery calcium predicts atherosclerotic cardiovascular disease(ASCVD) at 10 years: the Multi-Ethnic Study of Atherosclerosis(MESA) (Abstract). J Am Coll Cardiol 2016;67(13 Suppl):2017.
33. Bavishi C, Argulian E, Chatterjee S, Rozanski A. CACS and the frequency of stress-induced myocardial ischemia during MPI: a meta-analysis. JACC Cardiovasc Imaging 2016;9:580–9.
34. Kronmal RA, McClelland RL,Detrano R, Shea S, Lima JA,Cushman M, et al. Risk factors for the progression of coronary artery calci fication in asymptomatic subjects: results from the Multi-Ethnic Study of Atherosclerosis (MESA).Circulation 2007;115:2722–30.
35. Nasir K, Budoff MJ, Wong ND,Scheuner M, Herrington D,Arnett DK, et al. Family history of premature coronary heart disease and coronary artery calci fication: Multi-Ethnic Study of Atherosclerosis (MESA).Circulation 2007;116:619–26.
36. Paramsothy P, Knopp RH, Bertoni AG, Blumenthal RS, Wasserman BA, Tsai MY, et al. Association of combinations of lipid parameters with carotid intima-media thickness and coronary artery calcium in the MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2010;56:1034–41.
37. McEvoy JW, Nasir K, DeFilippis AP, Lima JA, Bluemke DA,Hundley WG, et al. Relationship of cigarette smoking with in flammation and subclinical vascular disease: the Multi-Ethnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol 2015;35:1002–10.
38. Wong ND, Nelson JC, Granston T,Bertoni AG, Blumenthal RS, Carr JJ,et al. Metabolic syndrome, diabetes,and incidence and progression of coronary calcium: the Multiethnic Study of Atherosclerosis study. JACC Cardiovasc Imaging 2012;5:358–66.
39. Pandey AK, Blaha MJ, Sharma K,Rivera J, Budoff MJ, Blankstein R, et al. Family history of coronary heart disease and the incidence and progression of coronary artery calci fication: Multi-Ethnic Study of Atherosclerosis (MESA).Atherosclerosis 2014;232:369–76.
40. Mulders TA, Taraboanta C,Franken LC, van Heel E, Klass G,Forster BB, et al. Coronary artery calci fication score as tool for risk assessment among families with premature coronary artery disease.Atherosclerosis 2016;245:155–60.
41. Kaufman JD, Adar SD, Barr RG,Budoff M, Burke GL, Curl CL,et al. Association between air pollution and coronary artery calci fication within six metropolitan areas in the USA (the Multi-Ethnic Study of Atherosclerosis and Air Pollution):a longitudinal cohort study. Lancet 2016;388(10045):696–704.
42. Budoff MJ, Hokanson JE, Nasir K, Shaw LJ, Kinney GL, Chow D,et al. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging 2010;3:1229–36.
43. Budoff MJ, Shaw LJ, Liu ST,Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calci fi-cation: observations from a registry of 25,253 patients. J Am Coll Cardiol 2007;49:1860–70.
44. Blaha M, Budoff MJ, Shaw LJ,Khosa F, Rumberger JA, Berman D, et al. Absence of coronary artery calci fication and all-cause mortality. JACC Cardiovasc Imaging 2009;2:692–700.
45. Blaha MJ, Cainzos-Achirica M, Greenland P, McEvoy JW,Blankstein R, Budoff MJ, et al.Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA).Circulation 2016;133:849–58.
46. Budoff MJ, Raggi P, Beller GA,Berman DS, Druz RS, Malik S, et al.Noninvasive Cardiovascular Risk Assessment of the Asymptomatic Diabetic Patient: The Imaging Council of the American College of Cardiology. JACC Cardiovasc Imaging 2016;9:176–92.
47. Whelton SP, Silverman MG,McEvoy JW, Budoff MJ, Blankstein R, Eng J, et al. Predictors of longterm healthy arterial aging: coronary artery calcium nondevelopment in the MESA study. JACC Cardiovasc Imaging 2015;8:1393–400.
48. Delaney JA, Jensky NE, Criqui MH, Whitt-Glover MC, Lima JA, Allison MA. The association between physical activity and both incident coronary artery calci fication and ankle brachial index progression: the multi-ethnic study of atherosclerosis. Atherosclerosis 2013;230:278–83.
49. Ahmed HM, Blaha MJ, Nasir K,Jones SR, Rivera JJ, Agatston A,et al. Low-risk lifestyle, coronary calcium, cardiovascular events, and mortality: results from MESA. Am J Epidemiol 2013;178:12–21.
50. Imran TF, Patel Y, Ellison RC, Carr JJ, Arnett DK, Pankow JS, et al.Walking and calci fied atherosclerotic plaque in the coronary arteries: the National Heart, Lung, and Blood Institute Family Heart Study.Arterioscler Thromb Vasc Biol 2016;36:1272–7.
51. Miedema MD, Petrone A, Shikany JM, Greenland P, Lewis CE,Pletcher MJ, et al. Association of fruit and vegetable consumption during early adulthood with the prevalence of coronary artery calcium after 20 years of follow-up: the Coronary Artery Risk Development in Young Adults (CARDIA) study.Circulation 2015;132:1990–8.
52. Spring B, Moller AC, Colangelo LA, Siddique J, Roehrig M,Daviglus ML, et al. Healthy lifestyle change and subclinical atherosclerosis in young adults:Coronary Artery Risk Development in Young Adults (CARDIA) study.Circulation 2014;130:10–7.
53. Stone NJ, Robinson JG,Lichtenstein AH, Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2889–934.
54. Kavousi M, Leening MJ, Nanchen D,Greenland P, Graham IM, Steyerberg EW, et al. Comparison of application of the ACC/AHA guidelines,Adult Treatment Panel III guidelines,and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort.JAMA 2014;311:1416–23.
55. DeFilippis AP, Young R,Carrubba CJ, McEvoy JW,Budoff MJ, Blumenthal RS, et al.An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med 2015;162:266–75.
56. Nasir K, Bittencourt MS, Blaha MJ,Blankstein R, Agatson AS, Rivera JJ,et al. implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2015;66:1657–68.
57. Villines TC. Coronary artery calcium score, distribution, and future revascularization. JACC Cardiovasc Imaging 2014;7:487–9.
58. Rozanski A, Gransar H, Shaw LJ, Kim J, Miranda-Peats L,Wong ND, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identi fication of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol 2011;57:1622–32.
 Cardiovascular Innovations and Applications2016年4期
Cardiovascular Innovations and Applications2016年4期
- Cardiovascular Innovations and Applications的其它文章
- Do Modern Imaging Studies Trump Cardiovascular Physical Exam in Cardiac Patients?
- Fractional Flow Reserve Measurement by Coronary Computed Tomography Angiography:A Review with Future Directions
- Novel Approaches for the Use of Cardiac/ Coronary Computed Tomography Angiography
- Magnetic Resonance Imaging of Coronary Arteries: Latest Technical Innovations and Clinical Experiences
- T1 and ECV Mapping in Myocardial Disease
- The Role of Clinical Cardiac Magnetic Resonance Imaging in China: Current Status and the Future
