Fractional Flow Reserve Measurement by Coronary Computed Tomography Angiography:A Review with Future Directions
Asim Rizvi*, Ji Hyun Lee*, Bríain ó Hartaigh Donghee Han Mahn Won Park Hadi Mirhedayati Roudsari Bin Lu, Fay Y. Lin and James K. Min
1Dalio Institute of Cardiovascular Imaging, Department of Radiology, New York–Presbyterian Hospital and the Weill Cornell Medical College, New York, NY, United States
2State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, Beijing, China
*Asim Rizvi and Ji Hyun Lee contributed equally to this manuscript.
lntroduction
Fractional flow reserve (FFR) is a robust tool to determine the hemodynamic significance of a coronary lesion and aids in reducing unnecessary coronary intervention and downstream adverse events [1].Recent advancements in computed tomography(CT) technology have led to the rapid development of coronary CT angiography (CCTA), which can noninvasively detect coronary artery disease (CAD).Despite this, CCTA cannot independently determine the hemodynamic significance of coronary stenosis.However, recent innovations in computational fluid dynamics (CFD) have offered alternatives and enabled the calculation of CCTA-derived FFR from threedimensional imaging anatomic models. This review provides an overview related to FFR measurement by CCTA (FFRCT) for the noninvasive evaluation of hemodynamically significant coronary stenosis.
lnvasive FFR Measurement
Invasive FFR measurements performed during cardiac catheterization represent the current gold standard in physiologic assessment of obstructive CAD and facilitate determination of whether a particular coronary stenosis is responsible for causing myocardial ischemia [2]. The FFR measurement is based on the relationship between coronary artery pressure and blood flow, and is de fined as the ratio of maximal hyperemic blood flow through a stenotic artery to maximal hyperemic flow in the hypothetical normal coronary artery [3, 4]. An FFR value of 0.80 or less is currently considered the common threshold for revascularization to improve clinical outcomes.
Current guidelines assign a class IA recommendation to advocate FFR for identi fication of hemodynamically significant coronary lesions in patients with no noninvasive evidence of ischemia [5].Despite unequivocal evidence from numerous studies supporting the clinical bene fit of FFR [6–11],the uptake of the use of FFR has been con fined by the invasive nature of the procedure and the additional time and equipment needed for measurement of each vessel during pharmacologic vasodilation.
Noninvasive FFR Measurement
FFRCTis a novel imaging modality for the noninvasive assessment of the hemodynamically significant coronary artery stenosis. FFRCTcan precisely localize ischemia-causing coronary stenoses by applying CFD to the CCTA data. The coupling of FFRCTwith CCTA provides a one-stop shop for combined anatomic physiologic evaluation, wherein FFR of three coronary vessels can be calculated from typically acquired CCTA images without the need for additional imaging or vasodilators [12].
Mechanism and Principles of FFRCT
FFRCTapplies CFD to compute “three-vessel” FFR from previously acquired CCTA image data by using standard acquisition protocols, without the need for additional medication, imaging, or radiation. The scienti fic basis that determines this technology has been previously well described [12]. In brief, there are three main elements for the computation of CCTA-derived FFR: (1) construction of a three-dimensional patient-specific anatomic model from CCTA data, (2) boundary conditions to de fine physiologic relationships between variables at the boundaries of the region of interest, and (3) numerical solutions of the governing fluid dynamics using Navier-Stokes equations. Further still, calculation of CCTA-derived FFR usually requires five basic steps: (1) creation of patient-specific anatomic models from CCTA, (2) quanti fication of the total and vessel-specific baseline coronary artery flow in the hypothetical case where the supplying vessels are normal, (3) determination of the baseline myocardial microcirculatory resistance, (4) quanti fication of the changes in coronary resistance with hyperemia, and (5) application of CFD methods for calculation of coronary flow, pressure, and velocity at rest and hyperemia. The latter step-by-step methods for calculating CCTA-derived FFR are illustrated in detail in Figure 1 [13]. In addition, Figure 2 demonstrates an example case of CCTA and FFRCT.Commercially available products for calculation of CCTA-derived FFR are available from HeartFlow(Redwood City, CA, US).
Diagnostic Performance of FFRCT
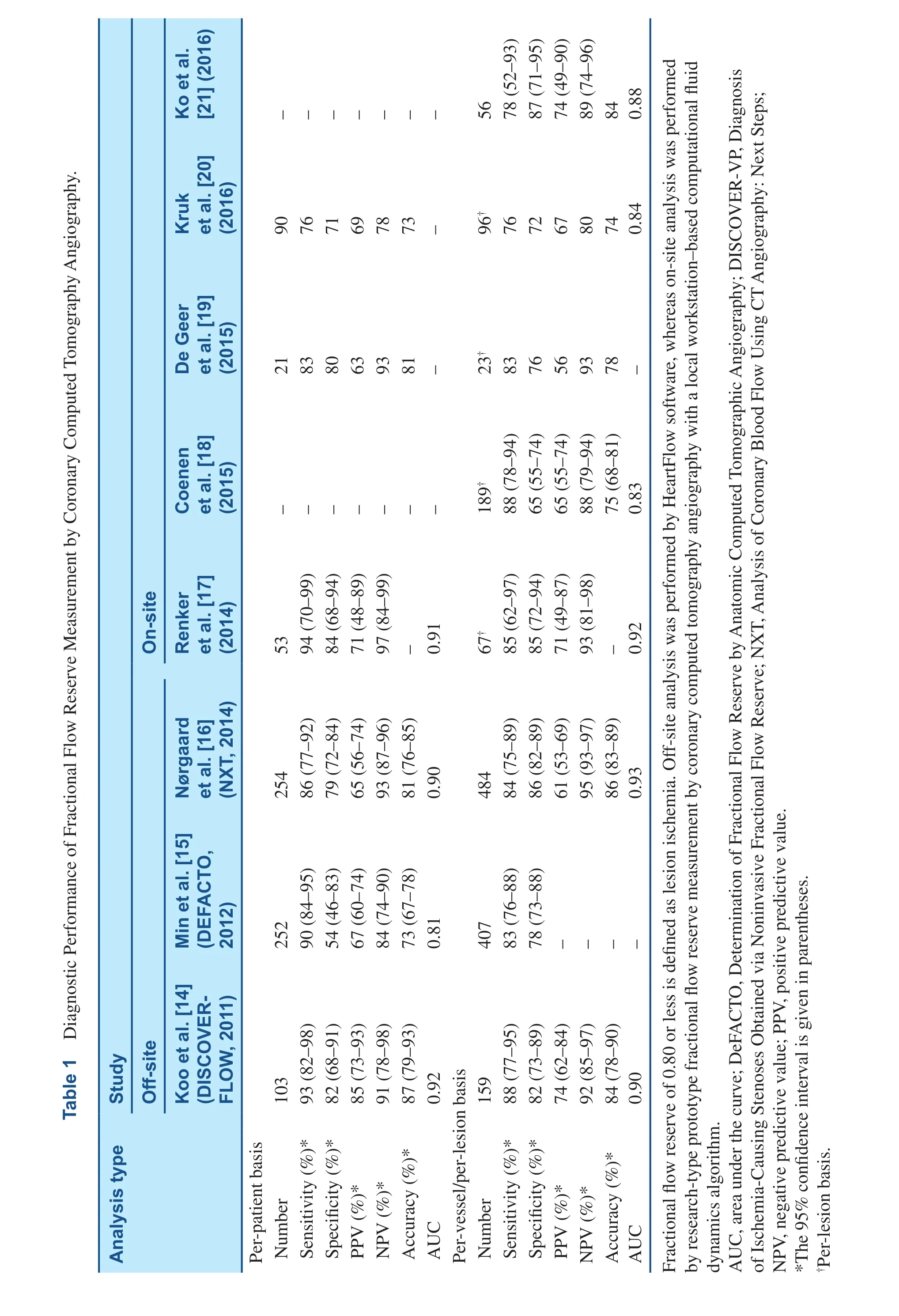
Three prospective multicenter trials, comprising more than 600 patients with masked core-laboratory analysis of 1050 vessels, have thus far investigated the diagnostic performance of FFRCTagainst invasive FFR measurement as the reference standard.These include the Diagnosis of Ischemia-Causing Stenoses Obtained via Noninvasive Fractional Flow Reserve (DISCOVER-FLOW), the Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography (DeFACTO), and the Analysis of Coronary Blood Flow Using CT Angiography: Next Steps (NXT). In these trials, FFRCThas proven to be superior to CCTA-determined stenosis alone for diagnosing ischemic lesions when compared with the reference standard,invasive FFR measurement (Table 1) [14–16].
The first trial to assess FFRCTtechnology against invasive coronary angiography (ICA) and invasive FFR measurement was the DISCOVER-FLOW study, in which FFRCTwas performed on 159 coronary vessels in 103 patients who underwent CCTA,ICA, and invasive FFR measurement from four sites in the United States, Europe, and Asia [14]. In this multicenter trial, ischemia was de fined as CCTA-derived FFR and FFR of 0.80 or less, whereas anatomically obstructive CAD was de fined by CCTA with stenosis of 50% or more. The accuracy, sensitivity, and specificity of FFRCTon a per-patient basis was 87% [95% con fidence interval (CI) 79–93%],93% (95% CI 82–98%), and 82% (95% CI 68.0–91.2%) respectively, compared with 61% (95% CI 51–71%), 94% (95% CI 85–99%), and 25% (95%CI 13–39%) for CCTA alone. In a per-vessel-based analysis, FFRCTdemonstrated higher accuracy,sensitivity, and specificity for ischemia-causing lesions of 84% (95% CI 78–90%), 88% (95% CI 77–95%), and 82% (95% CI 73–89%) respectively when compared with CCTA-determined stenosis alone, which exhibited accuracy, sensitivity, and specificity of 59% (95% CI 50–66%), 91% (95%CI 81–97%), and 40% (95% CI 30–50%) respectively. Notably, this study encountered its primary end point for detecting a relative improvement in diagnostic accuracy of 25% or more for FFRCT, as compared with CCTA-determined stenosis.
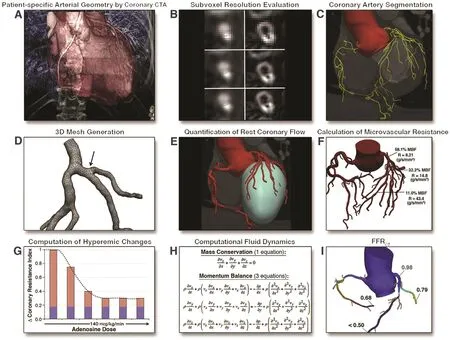
Figure 1 Step-by-Step Method for the Calculation of Fractional Flow Reserve Measured by Coronary Computed Tomography Angiography (FFRCT).(A) Acquisition of image by coronary computed tomography angiography (CTA). (B) Coronary artery segmentation to second-order and third-order vessels. (C) Application of subvoxel resolution techniques. In this example, a cross-section of a coronary artery shown with image intensity data (B, left) and image-gradient data (B, right) illustrates typical coronary CTA reconstruction with increasingly improved image resolution (B, middle and bottom) demonstrating subvoxel resolution techniques. (D) Discretization of mesh elements for calculation of computational fluid dynamics at millions of points in the coronary vascular bed. The tetrahedral vertices are reconstructed in three dimensions and are continuous even at the branch points to accurately calculate FFRCT at these areas commonly affected by plaque. Reduced-order methods that do not use threedimensional analyses are less accurate at these points. (E) Relationship of the location and size of coronary arteries to the left ventricular mass they subtend. (F) Relationship of coronary vessel caliber and flow and resistance. (G) Demonstration of reduced coronary resistance index at an adenosine dosage of 140 mcg/kg/min. (H) Navier-Stokes equations that govern the fluid dynamics of blood (nonlinear partial differential equations related to mass conservation and momentum balance are solved).(I) Example of a patient-specific FFRCT. MBF, myocardial blood flow.
The DeFACTO trial, which is a larger multicenter international study assessing FFRCTagainst CCTA for diagnostic accuracy of ischemia, was performed on 407 vessels in 252 patients from 17 centers in 5 countries who underwent CCTA, ICA, invasive FFR,and FFRCT[15]. In this study, FFR or CCTA-derived FFR of 0.80 or less was de fined as ischemia, whereas a stenosis of 50% or more was de fined as obstructive CAD. The investigators reported that the accuracy,sensitivity, and specificity of FFRCTon a per-patient basis were 73% (95% CI 67–78%), 90% (95% CI 84–95%), and 54% (95% CI 46–83%) respectively,compared with 64% (95% CI 58–70%), 84% (95%CI 77–90%), and 42% (95% CI 34–51%) for CCTA alone. The noninferiority end point was not achieved because the per-patient basis diagnostic accuracy of FFRCTplus CCTA did not exceed 70% of the lower bound of the 95% CI.
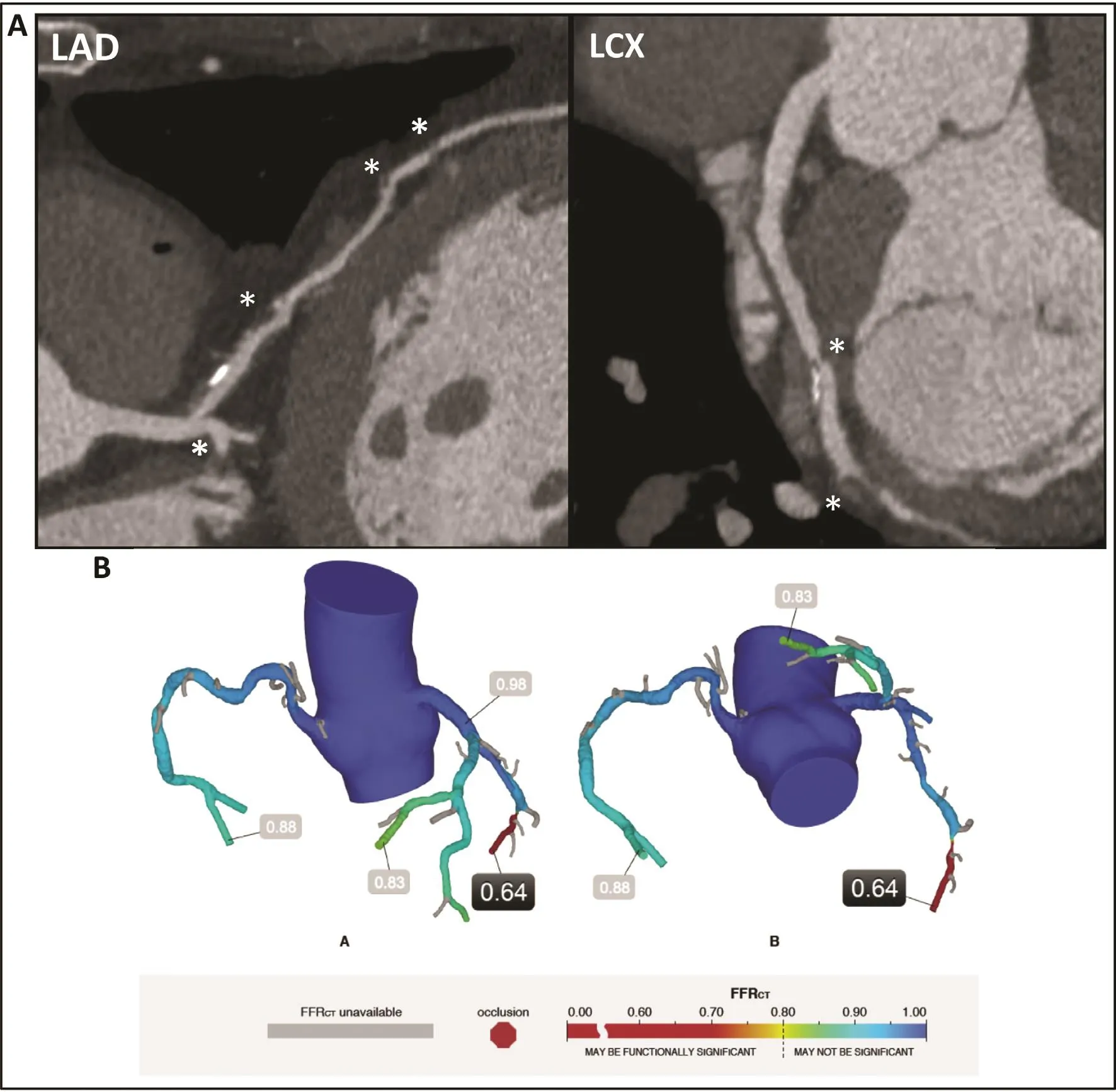
Figure 2 An Example Case of Coronary Computed Tomography Angiography (CCTA) and CCTA-derived Fractional Flow Reserve.(A) A 75-year-old white man presenting with exertional angina underwent CCTA. Multiplanar reformatting of CCTA data demonstrates moderate stenoses (asterisk) in the proximal and mid parts of the left anterior descending (LAD) artery, a severe stenosis in the left circum flex (LCX) artery, and a severe stenosis versus artifact in the distal part of the LCX artery. (B) The fractional flow reserves measured by coronary computed tomography angiography (FFRCT) of the LAD artery, the LCX artery,and the right coronary artery are 0.83, 0.64 and 0.88 respectively (>0.80 is normal). The value for the distal part of the LCX artery indicates significant ischemia.
?
Most recently, a third validation study, the NXT trial, was performed on 484 vessels in 254 patients from 10 sites in Europe, Australia, and Asia [16].The investigators used the most recent generation of FFRCTanalysis software (version 1.4) at HeartFlow with enhanced image quality and substantial re finements in physiologic models and image-processing methods. In this prospective international study of 254 patients (484 vessels) undergoing clinically indicated ICA because of suspected CAD, obstructive stenosis on CCTA was de fined as a greater than 50% lumen reduction, while ischemia was de fined as CCTA-derived FFR and FFR of 0.80 or less. The per-patient diagnostic accuracy, sensitivity, and specificity for FFRCTwere 81, 86, and 79% respectively versus 53% (P<0.001), 94% (P=0.058), and 34% (P<0.001)% for CCTA for identifying myocardial ischemia. Correspondingly, on a per-vessel basis, the diagnostic accuracy, sensitivity, and specificity were 86, 84, and 86% respectively for FFRCTagainst 65% (P<0.001), 83% (P=0.91), and 60%(P<0.001) for CCTA. Compared with the DeFACTO trial, the improved diagnostic power in the NXT trial likely re flects enhanced processing as well as increased focus on CCTA image quality, especially regarding heart rate control and nitroglycerin use[12, 22]. Accordingly, this trial revealed the high diagnostic performance of FFRCTas compared with invasive FFR measurement in identifying patients with hemodynamically significant obstructions with high sensitivity as well as high specificity.
In previous studies, the software application investigated was on the background of an off-site CT-based FFR algorithm, in which the dataset was delivered as a remote service that required the transfer of data, which would subsequently lead to several hours of processing. This method uses three-dimensional modeling with calculation of FFR values throughout the entire coronary vessels. Recently,several studies of an on-site research prototype using local workstation-based CFD algorithms have been developed, which use a simpli fied one-dimensional analysis using computational FFR (cFFR; Siemens Healthcare). This analysis potentially enables readers to compute cFFR values in selected locations of the coronary tree, which can then be compared with invasive FFR measurements. Among these investigations as shown in Table 1 [17–20], Kruk et al. [20]evaluated 96 lesions belonging to 90 patients, using a workstation-based calculation of cFFR for intermediate stenosis with invasive FFR measurement of 0.80 or less as the gold standard. They reported that the per-patient diagnostic accuracy, sensitivity,and specificity for cFFR were 73, 76, and 71%,compared with 47, 100, and 2% for CCTA. On a per-vessel basis, the diagnostic accuracy, sensitivity, and specificity were 74, 76, and 72% respectively, versus 44, 100, and 2% for CCTA. Unlike these studies using cFFR, an additional study using a reduced-order (one-dimensional) fluid model(CT-FFR; Toshiba Medical Systems) revealed that CT-FFR is reproducible and may accurately detect lesion-specific ischemia [21]. Although these findings are still in the preliminary stages, and require appropriate validation in a multicenter cohort, these studies have underscored the applicability of these software programs, which may allow the on-site evaluation of cFFR in cases as necessary in clinical practice, and within clinically viable time frames.
Diagnostic Performance of FFRCT in Patients with lntermediate Stenosis Severity
Among patients with intermediate stenosis severity(30–70%), differentiating between hemodynamically significant and nonsignificant coronary lesions is often challenging by either noninvasive imaging or ICA alone. Notably, the use of invasive FFR measurement is recommended as a class IIa indication in patients with intermediate lesions with less than 70% stenosis [23], as hemodynamically significant lesions are occasionally detected in these patients[1]. Nonetheless, given the lower prevalence of significant coronary lesions in this patient group when compared with those with severe stenosis in the Fractional Flow Reserve Versus Angiography for Multivessel Evaluation (FAME) study [1], FFRCTwould be more bene ficial for physiologic assessment of intermediate lesions and can potentially help avoid unnecessary invasive procedures. To this end, the DeFACTO study evaluated the diagnostic performance of FFRCTamong patients with intermediate stenosis severity. FFRCTdemonstrated a high diagnostic performance, with a greater than twofold increase in sensitivity over CCTA-determined stenosis alone [82% (95% CI 63–92%) vs. 37%(95% CI 22–56%)], without compromising specificity [66% (95% CI 53–77%) vs. 66% (95% CI 53–77%)]. The diagnostic accuracy of FFRCTversus CCTA was 71% (95% CI 61–80%) and 57% (95%CI 46–67%) respectively [24]. Further still, the NXT study displayed improved diagnostic power of FFRCTcompared with CCTA alone, with accuracy, sensitivity, and specificity of 80% versus 51%(P<0.0001), 85% versus 93% (P=0.058), and 79%versus 32% (P<0.0001) respectively [16].
Diagnostic Performance of FFRCT in Patients with Elevated Coronary Artery Calcium Scores
Heavily calci fied plaque with a severely elevated coronary artery calcium (CAC) score can cause blooming artifacts that can interfere with CCTA interpretation of stenosis, and can lead to reduced specificity and lower diagnostic accuracy. Studies have compared the diagnostic accuracy of FFRCTand CCTA for ischemia evaluation in patients with severely elevated CAC scores greater than 400, and have demonstrated that high calci fication does not affect FFRCTand it can maintain a high diagnostic accuracy, sensitivity, and specificity [16, 25, 26].In a subsequent substudy of the NXT trial, among patients with higher levels of coronary calci fication,the diagnostic accuracy, sensitivity, and specificity were higher for FFRCT[74% (95% CI 60–85%),88% (95% CI 62–98%), and 68% (95% CI 50–82%)respectively], as compared with CCTA alone [42%(95% CI 28–56%), 94% (95% CI 70–100%), and 19% (95% CI 8–35%) respectively] [26]. Similar findings with a high diagnostic performance for FFRCTcompared with CCTA were observed in a subanalysis of the DeFACTO trial (P>0.05) [25].
Clinical Utility and Cost-Effectiveness of FFRCT in Clinical Practice
The Prospective Longitudinal Trial of FFRCT:Outcome and Resource Impacts (PLATFORM) has evaluated the clinical utility of FFRCTto help guide clinical decision making among patients with suspected CAD [27]. In this prospective multicenter study, 584 patients with new-onset chest pain and intermediate CAD risk were referred to a standard care strategy (n=287), including a noninvasive test(n=100) or ICA (n=187), versus an FFRCT-guided diagnostic strategy (n=297). The primary end point was the rate of ICA normalcy, de fined as ICA findings without significant obstructive CAD, and important secondary end points were related to costs, resource utilization, quality of life, and radiation exposure. Among patients for whom ICA was planned (standard care, n=187; FFRCT-guided strategy, n=193), the study documented that ICA was cancelled in 61% of the latter group after FFRCThad been performed. Subsequently, no significant obstructive CAD was found in 73% of those who received the standard care strategy, while no significant obstructive CAD was found on ICA in only 12% of those who received the FFRCT-guided strategy, with both groups exposed to a similar cumulative radiation dose. Conversely, for those with the planned noninvasive test (standard care, n=100;FFRCT-guided strategy, n=104), there were no significant differences in the rate of no significant obstructive CAD by detected by ICA between the two strategies (6% vs. 13%, P=0.95). Importantly,this study suggests that FFRCTwas associated with a significantly lower rate of no obstructive CAD detected by ICA and likely provides a safer alternative to ICA, and may be considered as an alternative diagnostic tool for guiding clinical decision making in patients in whom ICA is planned. Follow-up after 1 year revealed too few major adverse cardiac events to evaluate the safety of the strategy [28].Larger studies will be needed to evaluate the safety of this promising strategy before its adoption in clinical practice.
More recently, Nørgaard et al. [29] aimed to assess the real-world clinical feasibility of FFRCTfor decision making among patients referred for FFRCTtesting with suspicion of CAD. They reported that CCTA-derived FFR of 0.80 or less correctly classified 73% of patients and 70% vessels using invasive FFR measurement of 0.80 or less as the reference standard. In contrast, patients with CCTA-derived FFR greater than 0.80 in whom ICA was being deferred did not experience adverse cardiac events during a median follow-up duration of 12 months.
Lately, although FFRCTwas commercially approved by the US Food and Drug Administration and received a CE mark in Europe in 2011, the evaluation of the cost-effectiveness of FFRCThas been an important issue in the context of the practical utility of this procedure. To this end, few investigations have evaluated the economic value of FFRCTover the ICA strategy [30–32]. In a substudy of DISCOVER-FLOW, Hlatky et al. [30] demonstrated that the use of FFRCTin the selection of patients for ICA and percutaneous coronary intervention (PCI)led to 30% lower costs at 1 year ($7674 per patient),when compared with ICA by visual assessment with PCI ($10,702 per patient). Similarly, in the NXT subanalysis study, an ICA-visual strategy showed the highest cost and projected 1-year death to myocardial infarction rate ($10,360 and 2.4%), whereas the strategy of initial CCTA with an FFRCT-guided strategy had a cost of $7222 and a projected 1-year death to myocardial infarction rate of 1.9% [31].Accordingly, use of the CCTA-FFRCTstrategy to select patients for PCI resulted in 30% lower medical costs and a 21% reduction in the death to myocardial infarction rate at 1 year when compared with the usual ICA-visual strategy [31]. More recently,a substudy of 584 patients from PLATFORM by Hlatky et al. [32] determined the effect of the use of FFRCTon cost and quality of life instead of standard care to assess stable patients with symptoms typical of CAD. In the invasive testing stratum,the FFRCTgroup showed a significant reduction of medical costs compared with the standard care group ($8619 vs. $10,734, P<0.0001), while in the noninvasive testing stratum, the FFRCTgroup had higher costs compared with the standard care group($2766 vs. $2137, P=0.02). However, the quality of life greatly improved in the FFRCTstrategy group as compared with the standard noninvasive strategy group (i.e., Seattle Angina Questionnaire 19.5 vs.11.4, P=0.003; EQ-5D 0.08 vs. 0.03, P=0.002; and visual analog scale 4.1 vs. 2.3, P=0.82) [32].
Further Studies Comparing FFRCT with Functional Stress lmaging Modalities
To date, the diagnostic performance of FFRCTfor prediction of ischemia has been assessed by many studies by use of invasive FFR measurement as the reference standard. However, studies evaluating the diagnostic performance of FFRCTin comparison with other stress imaging modalities are still lacking. To this end, several prospective multicenter trials are currently ongoing to test FFRCTagainst other methods of myocardial perfusion imaging. The Computed Tomographic Evaluation of Atherosclerotic Determinants of Myocardial Ischemia (CREDENCE) trial will determine the diagnostic performance of integrated CCTA plus FFRCTcompared with integrated myocardial perfusion imaging measures [33]. Further, two other multicenter trials, the Dual Energy CT for Ischemia Determination Compared to “Gold Standard” Non-Invasive and Invasive Techniques (DECIDE-Gold)trial and the Comparison Between Stress Cardiac Computed Tomography Perfusion Versus Fractional Flow Reserve Measured by Computed Tomography Angiography in the Evaluation of Suspected Coronary Artery Disease (PERFECTION) tial will investigate the diagnostic power of FFRCTagainst single- and dual-energy CT perfusion imaging modalities [34,35]. These studies will provide further insight into the clinical feasibility of FFRCT.
Limitations of FFRCT
An impaired CCTA image quality is a potential limitation that may not only affect the diagnostic performance of FFRCTbut may also in fluence the processing time of FFRCT. Numerous artifacts such as beam hardening from coronary calci fication,significant motion, misalignment, and increased image noise are important contributors to impaired image quality. Further, a high body mass index and an irregular or high heart rate can also impair image quality. Adherence to CCTA image acquisition guidelines [36] can help minimize these artifacts and can enhance the image quality, especially by controlling heart rate by use of beta-blockers and dilation of coronary arteries by sublingually administered nitrates. At present, the generalizability of FFRCTto a broader range of patient populations requires further elucidation, as most data are limited to stable patients without inclusion of those with acute coronary syndromes, or a history of coronary artery bypass surgery or PCI with suspected in-stent restenosis [37]. Moreover,the FFRCTprocessing and calculation in real-world clinical practice requires several hours for computation of CCTA-derived FFR. In this era of rapid technology, semiautomated and automated processes will likely overcome this limitation soon,thereby reducing the FFRCTprocessing time. In addition, the diagnostic performance of FFRCTamong patients with acute coronary syndrome,PCI, or coronary bypass graft surgery still needs to be explored. In this line, Gaur et al. [38] have recently documented that FFRCThas low diagnostic performance in patients with recent ST-segment elevation myocardial infarction. Accordingly, the clinical feasibility of FFRCTamong patients who have experienced recent acute coronary syndromes warrants further studies.
Future Directions and Applications of FFRCT
While the PLATFORM study reported on short-term outcomes, no studies have determined the long-term prognostic utility and the bene ficial effect of FFRCT-guided revascularization beyond CCTA findings– most likely because FFRCTwas only recently introduced. To this end, Assessing Diagnostic Value of Non-Invasive FFRCTin Coronary Care (ADVANCE)is a prospective multicenter longitudinal registry that will assess the prognostic utility of FFRCT-guided evaluation, and will include the clinical and economic impact of FFRCTas well as the potential reclassi fication of patients who have abnormal FFRCTfindings for adverse outcomes (NCT02499679) [13].
When compared with other noninvasive modalities, FFRCTmay potentially have the ability to simulate coronary vessel intervention so as to predict the bene fit of revascularization. To this end, the application of “virtual coronary stenting” is an emerging interest in the field of FFRCT. Kim et al. [39]determined the feasibility of FFRCTfor virtual stenting, wherein FFR was obtained by CCTA and CFD before and after virtual coronary stenting of the invasively treated coronary lesions. The computational model was modi fied to perform a virtual coronary intervention to enlarge the area of the target lesion in the coronary vessel according to the proximal and distal reference areas. Kim et al. reported a positive correlation between invasive FFR measurement and FFRCTbefore and after stenting, with 96% diagnostic accuracy of FFRCTafter stenting to predict ischemia (96% specificity, 100% sensitivity,50% positive predictive value, and 100% negative predictive value). In this pilot study, Kim et al. determined the utility of virtual stenting belonging to CT-derived computational models, thus indicating that this technology may be of value for determining an optimal revascularization plan and strategies before coronary intervention, and might also help reduce related costs by avoiding unnecessary revascularizations [30]. If con firmed by others, this novel technology may offset some of the other unnecessary factors such as additional procedure times, use of harmful contrast material, and unwanted radiation exposure.
Conclusion
As a novel noninvasive technology, FFRCTcan determine the physiologic significance of coronary stenosis along with anatomic CCTA image data. This computational analysis of FFRCTcan accurately identify coronary lesions that can cause myocardial ischemia.Prospective studies have shown higher diagnostic performance of FFRCTversus CCTA-determined stenosis alone. Undoubtedly, studies are warranted to fit this emerging modality into real-world clinical practice, while accounting for the cost-effectiveness of FFRCT-based strategies to help guide treatment decision making for improving patient care.
Conflict of lnterest
James K. Min serves as a consultant to HeartFlow and has received grant support from GE Healthcare.The other authors declare that they have no Conflicts of interest.
Funding
This review article was supported by a generous gift from the Dalio Institute of Cardiovascular Imaging (New York, NY, US) and the Michael Wolk Foundation (New York, NY, US).
REFERENCES
1. Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol 2010;55:2816–21.
2. Pijls NH, De Bruyne B. Coronary pressure measurement and fractional flow reserve. Heart 1998;80:539–42.
3. De Bruyne B, Baudhuin T, Melin JA, Pijls NH, Sys SU, Bol A, et al.Coronary flow reserve calculated from pressure measurements in humans. Validation with positron emission tomography. Circulation 1994;89:1013–22.
4. Pijls NH, Van Gelder B, Van der Voort P, Peels K, Bracke FA,Bonnier HJ, et al. Fractional flow reserve. A useful index to evaluate the in fluence of an epicardial coronary stenosis on myocardial blood flow. Circulation 1995;92:3183–93.
5. Windecker S, Kolh P, Alfonso F,Collet JP, Cremer J, Falk V, et al.2014 ESC/EACTS guidelines on myocardial revascularization:The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS).Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541–619.
6. Tonino PA, De Bruyne B, Pijls NH,Siebert U, Ikeno F, vant Veer M,et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. New Engl J Med 2009;360:213–24.
7. Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E,Bech JW, van’t Veer M, et al.Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER study. J Am Coll Cardiol 2007;49:2105–11.
8. Fearon WF, Bornschein B, Tonino PA, Gothe RM, De Bruyne B, Pijls NH, et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease.Circulation 2010;122:2545–50.
9. Li J, Elrashidi MY, Flammer AJ,Lennon RJ, Bell MR, Holmes DR, et al. Long-term outcomes of fractional flow reserve-guided vs.angiography-guided percutaneous coronary intervention in contemporary practice. Eur Heart J 2013;34:1375–83.
10. Park SJ, Ahn JM, Park GM, Cho YR, Lee JY, Kim WJ, et al. Trends in the outcomes of percutaneous coronary intervention with the routine incorporation of fractional flow reserve in real practice. Eur Heart J 2013;34:3353–61.
11. Van Belle E, Rioufol G, Pouillot C, Cuisset T, Bougrini K, Teiger E,et al. Outcome impact of coronary revascularization strategy reclassification with fractional flow reserve at time of diagnostic angiography:insights from a large French multicenter fractional flow reserve registry. Circulation 2014;129:173–85.
12. Taylor CA, Fonte TA, Min JK.Computational fluid dynamics applied to cardiac computed tomography for noninvasive quanti fication of fractional flow reserve:scienti fic basis. J Am Coll Cardiol 2013;61:2233–41.
13. Min JK, Taylor CA, Achenbach S,Koo BK, Leipsic J, Nørgaard BL,et al. Noninvasive fractional flow reserve derived from coronary CT angiography: clinical data and scienti fic principles. JACC Cardiovasc Imaging 2015;8:1209–22.
14. Koo BK, Erglis A, Doh JH, Daniels DV, Jegere S, Kim HS, et al.Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 2011;58:1989–97.
15. Min JK, Leipsic J, Pencina MJ, Berman DS, Koo BK, van Mieghem C, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 2012;308:1237–45.
16. Nørgaard BL, Leipsic J, Gaur S,Seneviratne S, Ko BS, Ito H, et al.Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J Am Coll Cardiol 2014;63:1145–55.
17. Renker M, Schoepf UJ, Wang R,Meinel FG, Rier JD, Bayer RR,et al. Comparison of diagnostic value of a novel noninvasive coronary computed tomography angiography method versus standard coronary angiography for assessing fractional flow reserve. Am J Cardiol 2014;114:1303–8.
18. Coenen A, Lubbers MM, Kurata A,Kono A, Dedic A, Chelu RG, et al.Fractional flow reserve computed from noninvasive CT angiography data: diagnostic performance of an on-site clinician-operated computational fluid dynamics algorithm.Radiology 2015;274:674–83.
19. De Geer J, Sandstedt M, Bjorkholm A, Alfredsson J, Janzon M, Engvall J,et al. Software-based on-site estimation of fractional flow reserve using standard coronary CT angiography data. Acta Radiol 2016;57:1186–92.
20. Kruk M, Wardziak L, Demkow M, Pleban W, Prgowski J,Dzieliska Z, et al. Workstationbased calculation of CTA-based FFR for intermediate stenosis. JACC Cardiovasc Imaging 2016;9:690–9.
21. Ko BS, Cameron JD, Munnur RK,Wong DT, Fujisawa Y, Sakaguchi T, et al. Noninvasive CT-derived FFR based on structural and fluid analysis: a comparison with invasive FFR for detection of functionally significant stenosis. JACC Cardiovasc Imaging 2016 (In press).
22. Gaur S, Achenbach S, Leipsic J,Mauri L, Bezerra HG, Jensen JM,et al. Rationale and design of the HeartFlowNXT (HeartFlow analysis of coronary blood flow using CT angiography: NeXt sTeps) study.J Cardiovasc Comput Tomogr 2013;7:279–88.
23. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011;124:e574–651.
24. Nakazato R, Park HB, Berman DS, Gransar H, Koo BK, Erglis A, et al. Noninvasive fractional flow reserve derived from computed tomography angiography for coronary lesions of intermediate stenosis severity: results from the DeFACTO study. Circulation Cardiovasc Imaging 2013;6:881–9.
25. Leipsic J, Yang TH, Thompson A,Koo BK, Mancini GJ, Taylor C,et al. CT angiography (CTA) and diagnostic performance of noninvasive fractional flow reserve:results from the Determination of Fractional Flow Reserve by Anatomic CTA (DeFACTO)study. AJR Am J Roentgenol 2014;202:989–94.
26. Nørgaard BL, Gaur S, Leipsic J,Ito H, Miyoshi T, Park SJ, et al.In fluence of coronary calci fication on the diagnostic performance of CT angiography derived FFR in coronary artery disease: a substudy of the NXT trial. JACC Cardiovasc Imaging 2015;8:1045–55.
27. Douglas PS, Pontone G, Hlatky MA, Patel MR, Norgaard BL, Byrne RA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFRCT: outcome and resource impacts study. Eur Heart J 2015;36:3359–67.
28. Douglas PS, De Bruyne B, Pontone G, Patel MR, Norgaard BL, Byrne RA, et al. 1-year outcomes of FFRCT-guided care in patients with suspected coronary disease:the PLATFORM study. J Am Coll Cardiol 2016;68:435–45.
29. Nørgaard BL, Hjort J, Gaur S,Hansson N, Bøtker HE, Leipsic J,et al. Clinical use of coronary CTA-derived FFR for decision-making in stable CAD. JACC Cardiovasc Imaging 2016 (In press).
30. Hlatky MA, Saxena A, Koo BK,Erglis A, Zarins CK, Min JK.Projected costs and consequences of computed tomography-determined fractional flow reserve. Clin Cardiol 2013;36:743–8.
31. Kimura T, Shiomi H, Kuribayashi S, Isshiki T, Kanazawa S, Ito H,et al. Cost analysis of non-invasive fractional flow reserve derived from coronary computed tomographic angiography in Japan. Cardiovasc Interv Ther 2015;30:38–44.
32. Hlatky MA, De Bruyne B, Pontone G, Patel MR, Norgaard BL, Byrne RA, et al. Quality-of-life and economic outcomes of assessing fractional flow reserve with computed tomography angiography:PLATFORM. J Am Coll Cardiol 2015;66:2315–23.
33. Rizvi A, Hartaigh BO, Knaapen P, Leipsic J, Shaw LJ, Andreini D, et al. Rationale and design of the CREDENCE trial: computed TomogRaphic evaluation of atherosclerotic DEtermiNants of myocardial IsChEmia. BMC Cardiovasc Disorders 2016;16:190.
34. Truong QA, Knaapen P, Pontone G,Andreini D, Leipsic J, Carrascosa P,et al. Rationale and design of the dual-energy computed tomography for ischemia determination compared to “gold standard” noninvasive and invasive techniques(DECIDE-Gold): a multicenter international ef ficacy diagnostic study of rest-stress dual-energy computed tomography angiography with perfusion. J Nucl Cardiol 2015;22:1031–40.
35. Pontone G, Andreini D, Guaricci AI,Guglielmo M, Mushtaq S, Baggiano A, et al. Rationale and design of the PERFECTION (comparison between stress cardiac computed tomography PERfusion versus Fractional flow rEserve measured by Computed Tomography angiography In the evaluation of suspected cOroNary artery disease) prospective study. J Cardiovasc Comput Tomogr 2016;10:330–4.
36. Nam CW, Mangiacapra F, Entjes R, Chung IS, Sels JW, Tonino PA,et al. Functional SYNTAX score for risk assessment in multivessel coronary artery disease. J Am Coll Cardiol 2011;58:1211–8.
37. Min JK, Koo BK, Erglis A, Doh JH, Daniels DV, Jegere S, et al.Usefulness of noninvasive fractional flow reserve computed from coronary computed tomographic angiograms for intermediate stenoses con firmed by quantitative coronary angiography. Am J Cardiol 2012;110:971–6.
38. Gaur S, Taylor CA, Jensen JM,Bøtker HE, Christiansen EH,Kaltoft AK, et al. FFR derived from coronary CT angiography in nonculprit lesions of patients with recent STEMI. JACC Cardiovasc Imaging 2016 (In press).
39. Kim KH, Doh JH, Koo BK, Min JK, Erglis A, Yang HM, et al. A novel noninvasive technology for treatment planning using virtual coronary stenting and computed tomography-derived computed fractional flow reserve. JACC Cardiovasc Interv 2014;7:72–8.
 Cardiovascular Innovations and Applications2016年4期
Cardiovascular Innovations and Applications2016年4期
- Cardiovascular Innovations and Applications的其它文章
- Do Modern Imaging Studies Trump Cardiovascular Physical Exam in Cardiac Patients?
- Novel Approaches for the Use of Cardiac/ Coronary Computed Tomography Angiography
- Coronary Calcium Scoring in 2017
- Magnetic Resonance Imaging of Coronary Arteries: Latest Technical Innovations and Clinical Experiences
- T1 and ECV Mapping in Myocardial Disease
- The Role of Clinical Cardiac Magnetic Resonance Imaging in China: Current Status and the Future
