新辅助化疗后中低位直肠癌的腹腔镜治疗评价
但操 刘雪君 卢建华 程新豹

[摘要] 目的 探讨新辅助化疗后中低位直肠癌的腹腔镜治疗效果。 方法 选取2014年7月~2015年6月我院收治的100例中低位直肠癌患者,随机分为观察组和对照组各50例,所有患者均行新辅助化疗,对照组在化疗后实施开腹手术,观察组患者在化疗后实施腹腔镜治疗,对比两组患者的手术指标、术后并发症情况。结果 观察组手术时间、术中出血量、肛门排气时间、住院时间分别为(209.7±44.2)min、(55.1±5.5)mL、(1.9±0.6)d、(11.4±3.2)d,与对照组的(205.4±39.6)min、(109.4±22.6)mL、(3.5±0.7)d、(12.1±4.0)d相比,术中出血量、肛门排气时间均显著低于对照组(P<0.05);观察组术后并发症发生率为20.0%,显著低于对照组的34.0%(P<0.05);观察组清扫淋巴结数量为(8.7±2.4)枚,对照组清扫数量为(9.1±3.0)枚,两组对比差异无统计学意义(P>0.05);观察组近端切除长度为(13.4±0.6)cm,远端切除长度为(3.0±0.4)cm,对照组近端切除长度为(13.1±0.6)cm,远端切除长度为(2.8±0.3)cm,两组对比差异无统计学意义(P>0.05)。 结论 中低位直肠癌患者在新辅助化疗后实施腹腔镜手术的近期疗效确切,具有创伤小、恢复快、并发症少的优势,值得在临床上推广应用。
[关键词] 中低位直肠癌;新辅助化疗;腹腔镜手术;近期疗效;术中出血量
[中图分类号] R574.6 [文献标识码] B [文章编号] 1673-9701(2016)09-0043-03
[Abstract] Objective To investigate the clinical efficacy of laparoscopic treatment of middle and low rectal cancer after neoadjuvant chemotherapy. Methods 100 patients with middle and low rectal cancer who were admitted in our hospital from July 2014 to June 2015 were selected as the subjects and randomly assigned into observation group and control group with 50 patients in each group. All the patients received neoadjuvant chemotherapy and patients from observation group received laparotomy after the chemotherapy while patients from control group received laparoscopic treatment. Operative indexes and postoperative complications of the patients from both groups were compared. Results The operation time, bleeding amount during the operation, the time of anal exsufflation and hospitalization time of the observation group were respectively (209.7±44.2) min, (55.1±5.5) mL, (1.9±0.6) d and (11.4±3.2) d, while those of the control group were (205.4±39.6) min, (109.4±22.6) mL, (3.5±0.7) d and (12.1±4.0) d. Compared with the control group, observation group had obviously less bleeding amount and shorter time of anal exsufflation(P<0.05); the occurrence of postoperative complications was 20.0%, significantly lower than the 34.0% of the control group (P<0.05); the number of lymph node dissection of the observation group were 8.7±2.4 while the number of the control group were 9.1±3.0 and there was no significant differences(P>0.05); the length of proximal resection and distal resection of the observation group were respectively 13.4±0.6cm and(3.0±0.4) cm, while the length of the proximal resection and distal resection of the control group were respectively (13.1±0.6) cm and (2.8±0.3) cm and there was no significant difference(P<0.05). Conclusion Laparoscopic surgery have definite short-term clinical efficacy in the treatment of patients with middle and low rectal cancer after neoadjuvant chemotherapy with advantages like small injury, quick recover and less complications, which deserves clinical recommendation and application.
[Key words] Middle and low rectal cancer; Neoadjuvant chemotherapy; Laparoscopic surgery; Short-term efficacy; Bleeding amount during the operation
直肠癌是常见的消化道恶性肿瘤之一,大量的循证医学证据表明新辅助化疗能够有效降低直肠癌的局部复发,提高根治性切除效果,同时也提高了低位直肠癌的保肛率,改善了患者的生存质量[1]。在手术方案选择上,腹腔镜手术是否安全可行临床尚存在一定争议,但也有研究表明直肠癌新辅助化疗后行腹腔镜手术是可行的。本文就新辅助化疗后腹腔镜手术治疗中低位直肠癌的近期疗效进行分析,现报道如下。
1 资料与方法
1.1 一般资料
本次采用前瞻性研究,研究对象选取为2014年7月~2015年6月我院收治的100例中低位直肠癌患者,男52例,女48例,年龄44~76岁,平均(65.1±6.9)岁。采用数字表法随机分为观察组和对照组各50例,两组年龄、性别等一般资料差异无统计学意义(P>0.05),均知情同意参与本次研究。
1.2 纳入及排除标准
纳入标准:①年龄44~76岁;②病理检验确诊为直肠癌;③肿瘤下缘距肛缘≤10 cm;④术前行新辅助化疗且可行根治性手术;⑤首次接受手术治疗;⑥知情同意。排除标准:①腺瘤性息肉病、大肠多源癌;②恶性淋巴瘤、黑色素瘤;③发生远端转移;④合并其他严重脏器功能障碍。
1.3 治疗方法
1.3.1 新辅助化疗 两组患者均给予同样方案的新辅助化疗,包括奥沙利铂(江苏奥赛康药业有限公司,国药准字H20064297)130 mg/m2静脉输注2 h,d1,卡培他滨(上海罗氏制药有限公司,国药准字J20080101)1000 mg/(m2·次),2次/d,d1~14,休息7 d,每3周为1个周期。
1.3.2 手术方案 观察组实施腹腔镜手术,患者取膀胱截石位,气管插管全麻,脐上1 cm穿刺建立气腹,维持负压12 mmHg,在右下腹髂前上棘内2横指部位穿刺做12 mm主操作孔,平脐位置向右5 cm穿刺做5 mm辅助操作孔,可根据患者体型适当将操作孔上移2~3 cm,根据从远到近的原则进行腹腔探查,最后观察病灶部位,中央入路,将右结肠旁沟进行切开,沿着间隙进行分离,游离腹主动脉,向上逐层剥离肠系膜、膜下动静脉,夹闭后离断血管,沿着Toldt间隙逐渐将乙状结肠及其系膜进行分离,过程中注意避免损伤尿管,遵循先后、再侧、最后前的顺序进行盆壁筋膜、直肠前壁和生殖器组织的分离,最后游离提肛肌平面,根据术式不同完成肠段切除和重建。手术过程中如果发现肿瘤无法完整切除或首先无法安全切缘者,则立刻转为开腹手术。对照组患者实施开腹手术,手术过程略。
1.4 观察指标
手术时间、术中出血量、排气时间、住院时间、保肛率、清扫淋巴结总数、肿瘤段切除长度及术后并发症。
1.5 统计学方法
采用SPSS19.0进行统计学处理,计量资料用(x±s)表示,组间对比采用t检验,计数资料采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1 两组手术指标比较
两组患者的手术时间、住院时间比较差异无统计学意义(P>0.05);但观察组患者的术中出血量、肛门排气时间均显著低于对照组(P<0.05)。见表1。
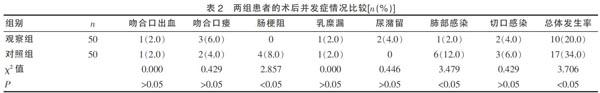
2.2 两组患者的术后并发症情况比较
观察组术后肠梗阻、肺部感染及总体并发症发生率均显著低于对照组(P<0.05)。见表2。
2.3 两组肿瘤根治性比较
所有患者术后均未发现环周及远端切缘阳性病例,均为R0切除。观察组清扫淋巴结数量为(8.7±2.4)枚,对照组清扫数量为(9.1±3.0)枚,两组对比差异无统计学意义(t=0.706,P>0.05);观察组近端切除长度为(13.4±0.6)cm,远端切除长度为(3.0±0.4)cm,对照组近端切除长度为(13.1±0.6)cm,远端切除长度为(2.8±0.3)cm,两组对比差异无统计学意义(t=0.468、0.913,P>0.05)。
3 讨论
新辅助化疗的提出为直肠癌的治疗提供了更多的选择。新辅助化疗不但能够进一步降低局部复发率,更能提高直肠癌的保肛率和生存质量,卫生部制定的《结直肠癌诊疗规范(2010版)》[2]中明确指出新辅助化疗属于局部进展期而无综合治疗禁忌直肠癌患者的标准疗法。近年来的研究也证实了,新辅助化疗后中低位直肠癌采用根治术治疗的疗效。但临床对于新辅助化疗后中低位直肠癌是否可行腹腔镜治疗仍存在争议。有学者[3]认为术前的新辅助化疗除了会引发骨髓抑制、消化系统反应等外,还会导致局部组织炎性浸润,纤维组织增生,导致解剖结构不清,腹腔镜手术难度增大。但也有学者[4]进行了新辅助放化疗后直肠癌患者的手术方案研究对照,结果显示腹腔镜手术的近期疗效与开腹手术相当,且具有并发症少的优势。从本次研究对比来看,观察组患者的手术出血量、肛门排气时间均显著低于对照组(P<0.05),说明腹腔镜手术损伤更小,术后肠道恢复更早。
在术后并发症的研究方面,临床报道腹腔镜与开腹手术的发生率分别在20%~65%、24%~56%之间[5],从本研究情况来看,观察组患者的术后总体并发症发生率为20.0%,对照组为34.0%,与报道基本一致,但两组对比结果显示,观察组术后肠梗阻、肺部感染及总体并发症发生率均显著低于对照组(P<0.05),考虑原因一方面是由于腹腔镜手术创伤小,相对于开腹手术对组织的而干扰更小,所以腹膜和浆膜的炎性反应更小,术后梗阻的可能性降低,而腹腔镜患者术后恢复更快,患者能够早期拔管、下床活动,便于咳嗽,减少了呼吸道感染的发生率[6]。从根治性对比来看,两组患者的淋巴结清扫数量、肠管切除长度对比均无显著差异,这个研究结论和Sebag等[7-15]的研究相一致,肯定了腹腔镜手术在肿瘤学根治性上的价值。
综上所述,中低位直肠癌患者在新辅助化疗后实施腹腔镜手术的近期疗效确切,具有创伤小、恢复快、并发症少的优势,值得在临床上推广和应用。
[参考文献]
[1] Sauer R,Becker H,Hohenberger W,et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer[J].N Engl J Med,2004,351(17):1731-1740.
[2] 卫生部医政司,结直肠癌诊疗规范专家工作组. 结直肠癌诊疗规范(2010年版)[J]. 中华胃肠外科杂志,2010,13(11):865-875.
[3] 黄美近,彭慧,王辉,等. 直肠癌腹腔镜与开腹手术肿瘤清除及远期疗效的随机对照试验荟萃分析[J]. 中华胃肠外科杂志,2011,14(8):606-610.
[4] Roh MS,Colangelo LH,O'Connell MJ,et al. Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum:NSABP R-03[J]. J Clin Oncol,2009,27(31):5124-5130.
[5] 陈一林,池畔. 腹腔镜和开腹直肠癌根治术的安全性及远期疗效比较[J]. 中华消化外科杂志,2012,11(5):462-466.
[6] Sauer R,Liersch T,Merkel S,et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer:Results of the German CAO/ARO/AIO-94 randomized phase Ⅲ trial after a median follow-up of 11 years[J]. J Clin Oncol,2012,30(16):1926-1933.
[7] Sebag-Montefiore D,Stephens RJ,Steele R,et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer(MRC CR07 and NCIC-CTG C016):A multicentre,randomised trial[J]. Lan-cet,2009,373(9666):811-820.
[8] Louhimo J,Carpelan-Holmstrom M,Alfthan H,et al. Serum HCG beta,CA72-4 and CEA are independent prognostic factors in colorectal cancer[J]. Int J Cancer,2012,101(6):545-548.
[9] Gunkel L,Mylonas I,Richter DU,et al. Immunohistochemical studies of mucinous mammary carcinomas and their metastases[J]. Anticancer Res,2015,25(3A) :1755-1759.
[10] Nakagoe T,Sawai T,Tsuji T,et al. Preoperative serum level of CA199 predicts recurrence after curative surgery in node-negative colorectal cancer patients[J]. Hepatogastroenterology,2013,50(51):696-699.
[11] Sari R,Yildirim B,Sevinc A,et al. The importance of serum and ascites fluid alphafetoprotein carcinoembryonic antigen,CA199 and CA125 levels in differential diagnosis of ascites etiology[J]. Hepatogastroenterology,2011, 48(12):1616-1621.
[12] Zhan T,Gu J,Li M,et al. Intermediate-fraction neoadjuvant radiotherapy for rectal cancer[J]. Dis Colon Rectum,2013,56(4):422-432.
[13] Heald RJ. Total mesorectal excision is optimal surgery for rectal cancer:A Scandinavian consensus[J]. Br J Surg,2015,82(10):1297-1299.
[14] 陈金湖. 中低位直肠癌新辅助放化疗后行腹腔镜与开腹根治术的疗效比较[D]. 福建医科大学,2013.
[15] Julien LA,Thorson AG. Current neoadjuvant strategies in rectal cancer[J]. J Surg Oncol,2014,101(4):321-326.
(收稿日期:2016-01-07)