Cyclical mastalgia: Prevalence and associated determinants in Hamadan City, Iran
Cyclical mastalgia: Prevalence and associated determinants in Hamadan City, Iran
Fatemeh Shobeiri1*, Khodayar Oshvandi1, Mansour Nazari21Mother and Child Care Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
2Department of Medical Entomology, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
Human disease http://dx.doi.org/10.1016/j.apjtb.2015.12.008
Tel: +98 9183169936
E-mail: fshobeiri@yahoo.com
The study protocol was performed according to the Helsinki declaration and approved by Research Ethics Committee of Hamadan University of Medical Sciences, Hamadan, Iran. Informed written consent was obtained from all participants.
Foundation Project: Supported by Research Deputy of Hamadan University of Medical Sciences, Hamadan, Iran (Grant No. 16.35.1.1642).
Peer review under responsibility of Hainan Medical University. The journal implements double-blind peer review practiced by specially invited international editorial board members.
2221-1691/Copyright©2016 Hainan Medical University. Production and hosting by Elsevier B.V. This is an open access article under the CC BY-NC-ND license (http:// creativecommons.org/licenses/by-nc-nd/4.0/).
ARTICLE INFO
Article history:
Received 15 Oct 2015
Received in revised form 8 Nov 2015 Accepted 30 Nov 2015
Available online 31 Dec 2015
Keywords:
Cyclical mastalgia
Iran
Prevalence
Case-control study
Associated determinants
ABSTRACT
Objective: To assess prevalence of cyclical mastalgia and its main determinants in women who attended in health centers of Hamadan City, Iran.
Methods: This case-control study was conducted on 400 women (case: cyclical mastalgia, n = 240; control: without cyclical mastalgia, n = 160) who attended family planning clinic for routine follow-up in health centers. The cluster sampling was used. Information was collected by interviewing and using a standardized validated questionnaire. Severity of mastalgia was assessed through using visual analog scaling. Data processing and statistical analysis were performed by using SPSS 19.0.
Results: Theresultsrevealedthatmajorityofwomen(60.0%)experiencedcyclicalmastalgia. Out of these, 22.5% and 37.5% were mild and moderate-to-severemastalgia, respectively. No association was revealed in experience of depression and anxiety in mastalgia group. In a multivariablelogisticregressionmodel,theincreasingage,ageofmarriage,historyofabortion and history of premenstrual syndrome were main determinants of mastalgia, while use of oral contraceptive and regular exercise was associated with lower incidence of mastalgia.
Conclusions: Most of women with breast discomfort suffered cyclical mastalgia which severitycanbedeterminedbyadvancedage,ageofmarriage,historyofabortionandhistory of premenstrual syndrome, but inversely by oral contraceptive use and exercise activity.
1. Introduction
Cyclical mastalgia affects up to two-thirds of women at some time during their reproductive lives. It is usually benign, but the fear of underlying breast cancer has become one of the most frequent reasons for consultation. Cyclic mastalgia is a common symptom experienced by women of reproductive age. It may be caused by the normal monthly changes in hormones. This pain usually occurs in both breasts. The pain is usually the most severe before a menstrual period and is often relieved when this period ends. Most cyclic pain relieves without treatment and usually disappears at menopause[1]. In most of the women who suffered from this phenomenon, reassurance is the only advice required because of its self-limited nature emerging gradually and spontaneously within a few months. However, in some of them, suggesting different types of lifestyles such as adopting regular exercise, weight reduction, modifying dietary regimens, and quitting smoking should be scheduled [2-4].
The prevalence of this complaint has been widely varied because of inter-individual differences and social features. The study by Coskun et al. reported the prevalence of mastalgia in womenattendingin breast screening program to be69%[5]. Amin etal.alsorevealedthat30%ofpremenstrualwomensufferedfrom cyclical mastalgia lasting for more than 5 days a month [6]. In another report by Ader et al., 68% of women aged 18-44 years experienced cyclical breast symptoms; 22% experienced moderate-to-extreme discomfort (classified as cyclical mastalgia) [7]. Another report showed that 15% was frequent mastalgia[8].
Mastalgia can be associated with premenstrual syndrome (PMS),fibrocystic breast disease, psychologic disturbance and, rarely, breast cancer. The majority of women can be reassured after a clinical evaluation. Approximately, 15% women with cyclical mastalgia require pain-relieving therapy. Mechanical breast support, a low-fat, high-carbohydrate diet and topical nonsteroidal anti-inflammatory agents are reasonable first-line treatments. Hormonal agents, such as bromocriptine, tamoxifen anddanazol,havedemonstratedefficacyinthetreatmentofmastalgia. Sixty percent of cyclic mastalgia recurs after treatment[1,3].
This variation in the prevalence of cyclical mastalgia not only depends on personal and social characteristics, but also is dependant to various determinant factors such as smoking, age, social and physical activities, and even psychological disturbances that should be identified to proper management of this phenomenon in each population [1]. Besides, because of its probable association with breast cancer, identifying risk factors of cyclical mastalgia is necessary.
This study aimed to assess prevalence of cyclical mastalgia and its main determinants in women who attended in health centers of Hamadan City, Iran in 2013.
2. Materials and methods
2.1. Study sample
This case-control study was carried out on 400 women aged 15-60 years who attended family planning clinic for routine follow-up in health centers of Hamadan City, Iran in 2013. The study included case subjects (n = 240) who had cyclical mastalgia. The control subjects (n = 160) were women who did not have cyclical mastalgia. The cluster sampling was used. Firstly, the Hamadan City was divided into 4 regions and then from each region, four health centers were selected. Ten women of each center who did not have cyclical mastalgia were selected as a control group and 15 women who had cyclical mastalgia were selected as a case group. The subjects were chosen randomly according to their cyclical mastalgia. Inclusion criteria were: age ranging from 15 to 45 years with a diagnosis of benign breast disorder (It is generally described as a heaviness or soreness that radiates to the armpit and arm), not pregnant, not breast feeding; and the exclusion criteria were: women with age below 15 and above 45 years, pregnancy, lactation, allergy to drugs, use of drugs (hormonal, danazol, aspirin and bromocriptine), no previous history of breast malignancies.
All relevant information was collected by interviewing and using a standardized validated questionnaire including demographic characteristics, marital state, occupational condition, anthropometric parameters, educational level, characteristics related to mastalgia such as its time and duration, characteristics related to menstrual cycles, results of diagnostic interventions (breast sonography and mammography), and also previous history of psychological disorders including depression or anxiety. Self-reported height and weight were assessed and body mass index was calculated as weight (kg)/m2. In this study, the diagnosis of depression and anxiety was made by using the Diagnostic and Statistical Manual of Mental Disorders IV.
Cyclical mastalgia was defined as a bilateral painful breast swelling, lasting for more than 4 days and up to 3 weeks, always preceding menses, and subsiding progressively during menstruation [9]. Furthermore, severity of mastalgia was assessed by using visual analog scaling that scored between 0 and 10 and higher scores indicated higher pain severity.
2.2. Ethical considerations
The study was performed according to the Helsinki declaration protocol. The objectives of the study were explained to the women, and informed consent was obtained from all participants. Women could leave the study at any time. The study was approved by the Ethical Committee of Hamadan University of Medical Sciences.
2.3. Statistical analysis
Results were reported as mean±SD for the quantitative variables and percentages for the categorical variables. The groups were compared by using the student's t-test for the continuous variables and the Chi-square test (or Fisher's exact test if required) for the categorical variables. Multivariate logistic regression analysis was taken to investigate their independence predictors. P-values less than 0.05 were considered statistically significant. Data processing and statistical analysis were performed by using SPSS version 19.0.
3. Results
The presence of cyclical mastalgia was reported in 60.0% of studied women. Out of these, 22.5% women had mild and 37.5% moderate-to-severe mastalgia, respectively. In mastalgia group, average duration of mastalgia was (5.52±3.39) years and 95.8% of them, mastalgia was appeared before menstrual period. The mean score of mastalgia was 3.22±2.97. Majority of women (14%) had mastalgia“5”according visual analog scaling (Figure 1). A summary of women characteristics with or without mastalgia is shown in Table 1. No significant differences were found as far as marital status, educational level, number of parity, breast feeding, regularity of menstrual cycles, prevalence of chronic pelvic pain, family history of breast cancer, body mass index, age at menarche, as well as duration and interval of menstrual cycles. With regard to other characteristics, those who suffered from mastalgia were older, had higher mean marital age, experienced higher number of abortions, and suffered more from PMS in comparison with another group. Also, women with mastalgia expressed to have more regular exercise activity and have higher experience of breast sonography and mammography. Regarding psychological states, no discrepant was revealed in experience of depression; however anxiety was slightly more prevalent in mastalgia group. There was also significant difference in method of contraception in which the use of withdrawal method was more observed in mastalgia group, while using oral contraceptive (OCP) was more found in control group (Figure 2).
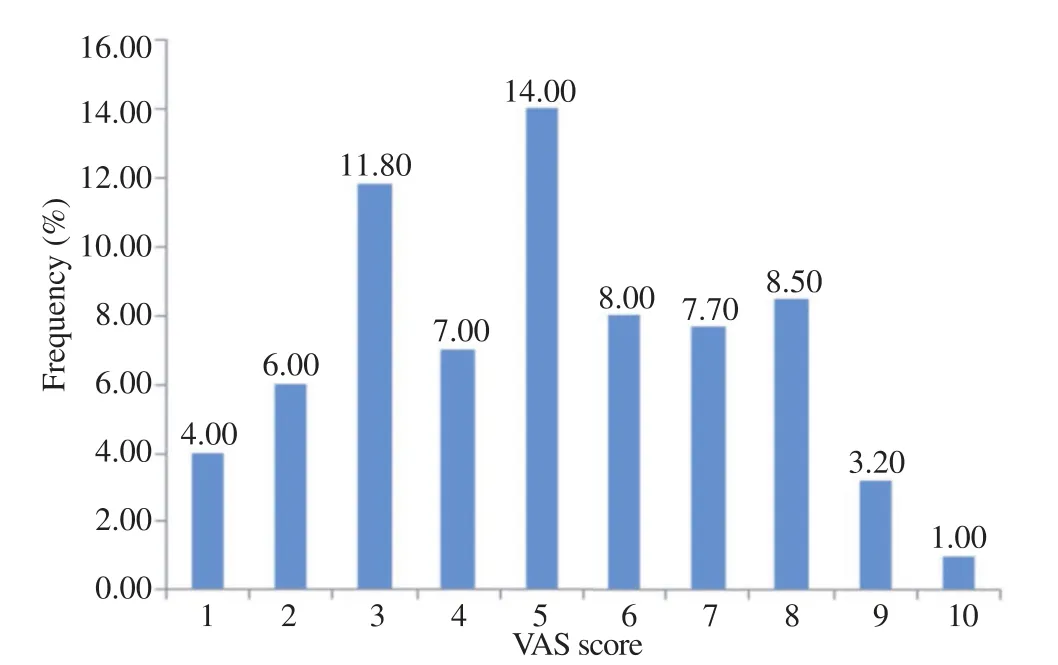
Figure 1. Distribution of pain severity in mastalgia group. VAS: Visual analog scaling.
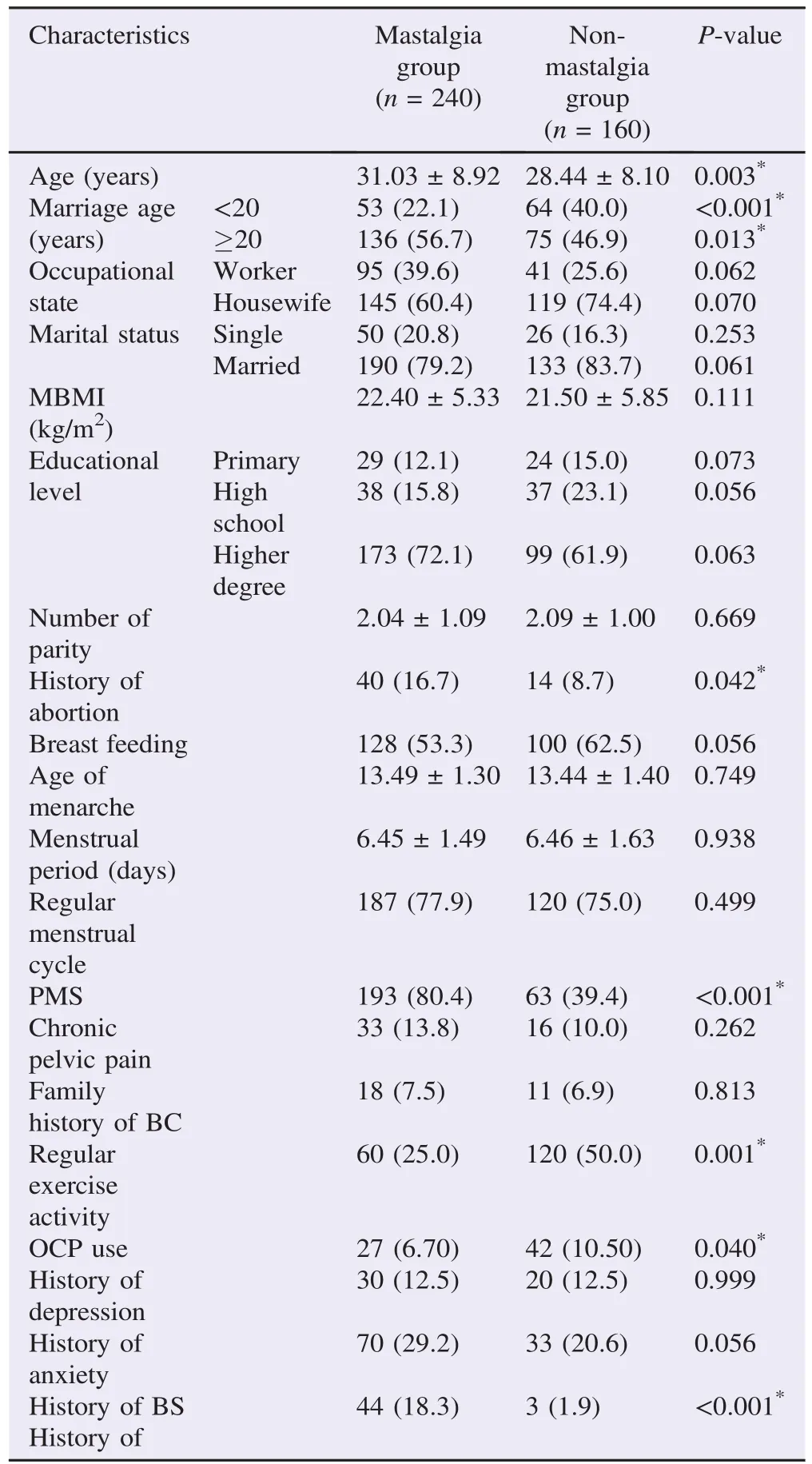
Table 1 Baseline characteristics and clinical data of study population. n (%).
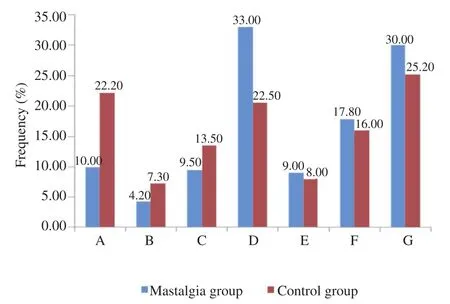
Figure 2. The frequency of method used of contraception in mastalgia and control groups.A: OCP; B: DMPA; C: IUD; D: Withdrawal; E: Surgery; F: Kandom; G: Others.
For determining indicators of the appearance of mastalgia and in a multivariable logistic regression model, advanced age, age of marriage, and history of PMS were main determinants of mastalgia, while use of OCP was associated with lower incidence of mastalgia (Table 2). Meanwhile, in a multivariate linear regression analysis, severity of mastalgia was positively related to high age, high marriage age, history of abortion, suffering from PMS, whereas it was adversely associated with regular exercise activity and use of OCP (Table 3).
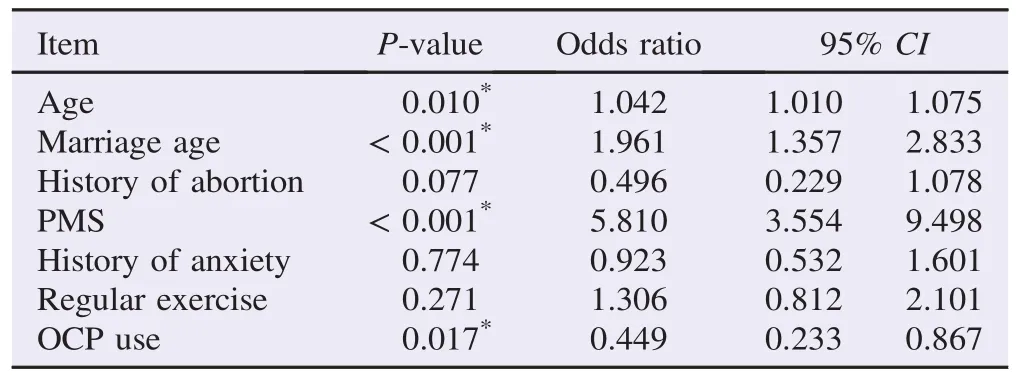
Table 2 Multivariate logistic regression model for determinants of mastalgia.
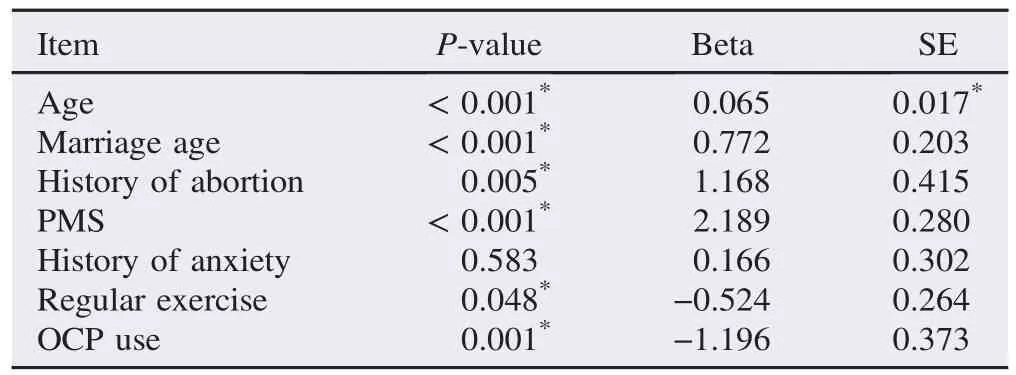
Table 3 Multivariate linear regression model for determinants of severity of mastalgia.
4. Discussion
According to our findings, 60.0% of our women suffered from cyclical mastalgia and in most of them the pain was appeared before menstrual period. Regarding main indicators of this phenomenon, multivariable regression modeling showed increasing age, age of marriage, history of abortion and history of PMS were main determinants of mastalgia, while use of OCP and regular exercise was associated with lower incidence of mastalgia. No association was revealed with experience of depression and anxiety in mastalgia group. While another report showed that frequent mastalgia is strongly associated with post traumatic stress disorder and other psychiatric conditions. Clinicians seeing patients with frequent mastalgia should inquire about anxiety, depression, alcohol misuse, and trauma history[8,9].
The study by Ader et al. showed that 30% of premenstrual women suffered from cyclical mastalgia lasting for more than 5 days a month[7], which was of sufficient severity to interfere with sexual, physical, social and work-related activities. Furthermore, Brown et al. [10], found the prevalence of mastalgia in women attending a breast screening program to be 69%. In another survey, it was reported that 68% of women experienced cyclical breast symptoms and 22% of these women experienced moderate-to-extreme discomfort [11]. Hormonal contraceptive usage was associated with significantly less mastalgia and PMS. While, smoking, caffeine consumption and perceived stress were associated with mastalgia. Also, younger womenwith mastalgia were more likely to have had a mammogram than those without mastalgia (20.2% versus 9.9%). Also, they also reported in another observation that mastalgia was not significantly associated with PMS so 82% of women with clinical cyclical mastalgia did not have this syndrome [12]. The literatures have revealed that in another countries, mastalgia is a common complaint that may affect up to 70% of women in their lifetime [13,14]. Interestingly, it is less common in Asian cultures, affecting as few as 5% [15]. Cyclical mastalgia affects up to 40% of women before menopause, most often in their thirties [16]. In approximately 8% of these women had severe pain which interfered with their normal activities. A minority of women with the most severe pain experienced it during menstruation [17]. The pain can continue for many years but will usually disappear after menopause. Comparing our results with previous observations in both eastern and western societies showed that the pattern of cyclical mastalgia in our community is following similar patterns in western countries, indicating high incidence of mastalgia in affected women, especially before menstrual period.
The exact cause of cyclical mastalgia is poorly understood, but based on our results and other similar findings, the link to the menstrual cycle makes a hormonal connection likely. On the other hand, the use of OCPs could effectively reduce pain and discomfort severity in affected women. It has been demonstrated that when breast pain occurs in women taking OCPs, it often resolves after a few cycles [18,19]. In a randomized controlled trial, of 1417 women comparing contraceptives, breast pain was cited by 18% of those using transdermal therapy versus 5.8% of those using oral therapy, and was described by 85% as mild-moderate in severity. A multi-institutional cross-section prevalence study found that women receiving long-acting parenteral progesterones for contraception were significant less breast pain than those of the control group. It is unclear whether OCPs relieve or cause cyclic mastalgia [19].
Regarding psychological states, no discrepant was revealed in experience of depression; however anxiety was slightly more prevalent in mastalgia group. In fact, women with anxiety background might suffer from mastalgia more than other women. In a study by Shrestha and Sen[20], compared to women without mastalgia, women with frequent mastalgia were more likely to screen positive for major depression, panic disorder, eating disorder, alcohol misuse, and domestic violence. Another study [21], which compared several groups of women, reported the high levels of mood disturbance in women with severe mastalgia.
Most of women with breast discomfort suffer cyclical mastalgia which severity can be determined by advanced age, age of marriage, history of abortion and history of PMS, but inversely by OCP use and exercise activity. Whether stress is a result of the pain or a contributing factor, psychological assessment and support is an integral part of the management of mastalgia.
Conflict of interest statement
We declare that we have no conflict of interest.
Acknowledgments
The authors sincerely acknowledge the Hamadan University of Medical Sciences in Iran for their valuable support and participation. The paper was funded by Research Deputy of Hamadan University of Medical Sciences, Hamadan, Iran. Grant number and ethical committee code was: 16.35.1.1642.
References
[1] Iddon J, Dixon JM. Mastalgia. BMJ 2013; 347: f3288.
[2] Joyce DP, Alamiri J, Lowery AJ, Downey E, Ahmed A, McLaughlin R, et al. Breast clinic referrals: can mastalgia be managed in primary care? Ir J Med Sci 2014; 183(4): 639-42.
[3] Shobeiri F, Jenabi E. The effects of vitamin E on muscular pain reduction in students affected by premenstrual syndrome. Iran J Obstet Gynecol Infertil 2014; 17(96): 1-5.
[4] Duflos C, Plu-Bureau G, Thibaud E, Kuttenn F. Breast diseases in adolescents. Endocr Dev 2012; 22: 208-21.
[5] Coskun AK, Harlak A, Mentes O. Breast clinic referrals: can mastalgia be managed in primary care? Ir J Med Sci 2014; 183(3): 509.
[6] Amin AL, Purdy AC, Mattingly JD, Kong AL, Termuhlen PM. Benign breast disease. Surg Clin North Am 2013; 93(2): 299-308.
[7] Ader DN, South-Paul J, Adera T, Deuster PA. Cyclical mastalgia: prevalence and associated health and behavioral factors. J Psychosom Obstet Gynaecol 2001; 22(2): 71-6.
[8] Shobeiri F, Oshvandi K, Nazari M. Clinical effectiveness of vitamin E and vitamin B6 for improving pain severity in cyclic mastalgia. Iran J Nurs Midwifery Res 2015; 20(6): 723-7.
[9] Plu-Bureau G, Lˆe MG, Sitruk-Ware R, Thalabard JC. Cyclical mastalgia and breast cancer risk: results of a French cohort study. Cancer Epidemiol Biomarkers Prev 2006; 15(6): 1229-31.
[10] Brown N, White J, Brasher A, Scurr J. The experience of breast pain (mastalgia) in female runners of the 2012 London Marathon and its effect on exercise behaviour. Br J Sports Med 2014; 48(4): 320-5.
[11] Kataria K, Dhar A, Srivastava A, Kumar S, Goyal A. A systematic review of current understanding and management of mastalgia. Indian J Surg 2014; 76(3): 217-22.
[12] Edelman A, Micks E, Gallo MF, Jensen JT, Grimes DA. Continuous or extended cycle vs. cyclic use of combined hormonal contraceptives for contraception. Cochrane Database Syst Rev 2014; http://dx.doi.org/10.1002/14651858.CD004695.pub3.
[13] Fan Y, Pei X, Liu Z, Xia Z, Zhang D, Song A, et al. Effectiveness of external Sanjierupi Gao on mastalgia caused by mammary gland hyperplasia: a placebo controlled trial. J Tradit Chin Med 2013; 33(5): 603-7.
[14] Vaziri F, Zamani Lari M, Samsami Dehaghani A, Salehi M, Sadeghpour H, Akbarzadeh M, et al. Comparing the effects of dietary flaxseed and omega-3 Fatty acids supplement on cyclical mastalgia in Iranian women: a randomized clinical trial. Int J Fam Med 2014; http://dx.doi.org/10.1155/2014/174532.
[15] Salzman B, Fleegle S, Tully AS. Common breast problems. Am Fam Physician 2012; 86(4): 343-9.
[16] Rogulski L, Bi nczyk J. Estimated breast cancer risk and screening outcomes among premenopausal women with non-cyclic mastalgia. Ginekol Pol 2013; 84(9): 754-7.
[17] Khan SA, Apkarian AV. The characteristics of cyclical and noncyclical mastalgia: a prospective study using a modified McGill pain questionnaire. Breast Cancer Res Treat 2002; 75(2): 147-57.
[18] Tehranian N, Shobeiri F, Pour FH, Hagizadeh E. Risk factors for breast cancer in Iranian women aged less than 40 years. Asian Pac J Cancer Prev 2010; 11(6): 1723-5.
[19] Audet MC, Moreau M, Koltun WD, Waldbaum AS, Shangold G, Fisher AC, et al. Evaluation of contraceptive efficacy and cycle control of a transdermal contraceptive patch vs an oral contraceptive: a randomized controlled trial. JAMA 2001; 285(18): 2347-54.
[20] Shrestha S, Sen T. Analysis of mastalgia cases presented at Manipal Teaching Hospital, Pokhara, Nepal. Nepal Med Coll J 2004; 6(2): 129-32.
[21] Kyranou M, Paul SM, Dunn LB, Puntillo K, Aouizerat BE, Abrams G, et al. Differences in depression, anxiety, and quality of life between women with and without breast pain prior to breast cancer surgery. Eur J Oncol Nurs 2013; 17(2): 190-5.
*Corresponding author:Fatemeh Shobeiri, Associate Professor, Mother and Child Care Research Center, Hamadan University of Medical Sciences, Hamadan, Iran.
 Asian Pacific Journal of Tropical Biomedicine2016年3期
Asian Pacific Journal of Tropical Biomedicine2016年3期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- Natural antibacterial remedy for respiratory tract infections
- Quantitative determination of vitexin in Passiflora foetida Linn. leaves using HPTLC
- Screening and antibacterial efficacy of selected Indian medicinal plants
- Anti-herpes simplex virus activities of monogalactosyl diglyceride and digalactosyl diglyceride from Clinacanthus nutans, a traditional Thai herbal medicine
- Analgesic and anti-inflammatory potential of aerial parts of the Daphne mucronata Royle extract in mice: Opioid-independent action
- Sub-chronic effects of a Phthirusa pyrifolia aqueous extract on reproductive function and comparative hormone levels in male rats
