老年慢性心力衰竭患者甲状腺激素、氨基末端脑钠肽前体变化及其对预后的评估价值
刘建飞,彭宗清,夏 豪
441000湖北省襄阳市中心医院北区(刘建飞,彭宗清);武汉大学人民医院(夏豪)
·论著·
老年慢性心力衰竭患者甲状腺激素、氨基末端脑钠肽前体变化及其对预后的评估价值
刘建飞,彭宗清,夏 豪
441000湖北省襄阳市中心医院北区(刘建飞,彭宗清);武汉大学人民医院(夏豪)
【摘要】目的分析老年慢性心力衰竭(CHF)患者甲状腺激素、氨基末端脑钠肽前体(NT-proBNP)变化及其对预后的评估价值。方法选取2012年5月—2015年2月在襄阳市中心医院心内科住院的老年CHF患者120例作为CHF组,其中心功能Ⅱ级42例,心功能Ⅲ级47例,心功能Ⅳ级31例。另选取同期在本院体检健康的老年人120例作为对照组。比较两组受试者及不同心功能分级CHF患者血浆甲状腺激素〔三碘甲状腺原氨酸(T3)、甲状腺素(T4)、游离三碘甲状腺原氨酸(FT3)、游离甲状腺素(FT4)、促甲状腺激素(TSH)〕、NT-proBNP水平及左心室射血分数(LVEF),并分析CHF患者血浆NT-proBNP水平及LVEF与血浆甲状腺激素水平的相关性。根据CHF患者住院期间心血管事件发生情况分为心血管事件组42例和非心血管事件组78例,比较心血管事件组与非心血管事件组患者血浆甲状腺激素、NT-proBNP水平及LVEF。结果CHF组与对照组受试者血浆T4、FT4、TSH水平比较,差异无统计学意义(P>0.05);CHF组患者血浆T3、FT3水平及LVEF低于对照组,血浆NT-proBNP水平高于对照组(P<0.05)。不同心功能分级CHF患者血浆T4、FT4、TSH水平比较,差异无统计学意义(P>0.05);心功能Ⅲ级患者血浆FT3水平低于心功能Ⅱ级患者,血浆NT-proBNP水平高于心功能Ⅱ级患者(P<0.05);心功能Ⅳ级患者血浆T3、FT3水平及LVEF低于心功能Ⅱ、Ⅲ级患者,血浆NT-proBNP水平高于心功能Ⅱ、Ⅲ级患者(P<0.05)。Pearson相关性分析结果显示,血浆NT-proBNP水平与血浆T3、FT3水平呈负相关(r值分别为-0.335、-0.221,P<0.05),与血浆T4、FT4、TSH水平无直线相关性(r值分别为0.047、0.027、0.015,P>0.05)。LVEF与血浆T3、FT3水平呈正相关(r值分别为0.410、0.229,P<0.05),与血浆T4、FT4、TSH水平无直线相关性(r值分别为0.085、0.087、0.004,P>0.05)。心血管事件组与非心血管事件组患者血浆T4、FT4、TSH水平比较,差异无统计学意义(P>0.05);心血管事件组患者血浆T3、FT3水平低于非心血管事件组,血浆NT-proBNP水平高于非心血管事件组(P<0.05)。结论老年CHF患者血浆T3、FT3水平较低,血浆NT-proBNP水平较高,T3、FT3、NT-proBNP可作为评估CHF患者病情严重程度及预后的指标。
【关键词】心力衰竭;甲状腺激素类;氨基末端脑钠肽前体;预测
刘建飞,彭宗清,夏豪.老年慢性心力衰竭患者甲状腺激素、氨基末端脑钠肽前体变化及其对预后的评估价值[J].实用心脑肺血管病杂志,2016,24(1):7-11.[www.syxnf.net]
Liu JF,Peng ZQ,Xia H.Changes of thyroid hormones and NT-proBNP and the estimated value on prognosis of elderly patients with chronic heart failure[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2016,24(1):7-11.
慢性心力衰竭(CHF)是心血管疾病的终末阶段,是指由于血流动力学改变及神经内分泌系统紊乱而导致心室重塑,最终引起心排血量下降的临床综合征。CHF预后极差,1年病死率约为30%,10年病死率高达90%[1]。脑利钠肽(BNP)是由心室肌细胞分泌的一种心脏神经激素,心室肌细胞受到牵拉刺激后分泌氨基末端脑钠肽前体(NT-proBNP)。目前,NT-proBNP在诊断心力衰竭及评价心力衰竭患者预后方面的重要性已被证实[2-3]。甲状腺激素对维持心血管稳态起重要作用,有研究显示,甲状腺激素水平与CHF的发生发展关系密切。甲状腺激素尤其是三碘甲状腺原氨酸(T3)有明显的心血管效应,包括降低外周血管阻力及促进心肌舒张[4]。严重心力衰竭患者甲状腺功能障碍主要表现为“低T3综合征”,即总血清T3及游离三碘甲状腺原氨酸(FT3)水平降低,而甲状腺素(T4)、游离甲状腺素(FT4)及促甲状腺激素(TSH)水平无明显变化[5]。本研究旨在分析老年CHF患者甲状腺激素、NT-proBNP变化及其对预后的评估价值,现报道如下。
1资料与方法
1.1一般资料选取2012年5月—2015年2月在襄阳市中心医院心内科住院的老年CHF患者120例作为CHF组,均符合美国心脏病学会/美国心脏病协会(ACC/AHA)关于CHF的诊断和治疗指南中的诊断标准。CHF患者中心功能Ⅱ级42例,心功能Ⅲ级47例,心功能Ⅳ级31例。另选取同期在本院体检健康的老年人120例作为对照组。两组受试者年龄、性别、吸烟史阳性率、饮酒史阳性率比较,差异无统计学意义(P>0.05,见表1),具有可比性。排除标准:(1)肝肾功能不全者;(2)近1个月内服用过影响甲状腺激素分泌的药物者;(3)严重感染、创伤、肿瘤、结缔组织病、血液疾病、电解质代谢紊乱、甲状腺疾病、慢性阻塞性肺疾病、肺动脉栓塞者。本研究经襄阳市中心医院伦理委员会批准,受试者均知情同意并签署知情同意书。
表1CHF组与对照组受试者一般资料比较
Table 1Comparison of general information between CHF group and control group
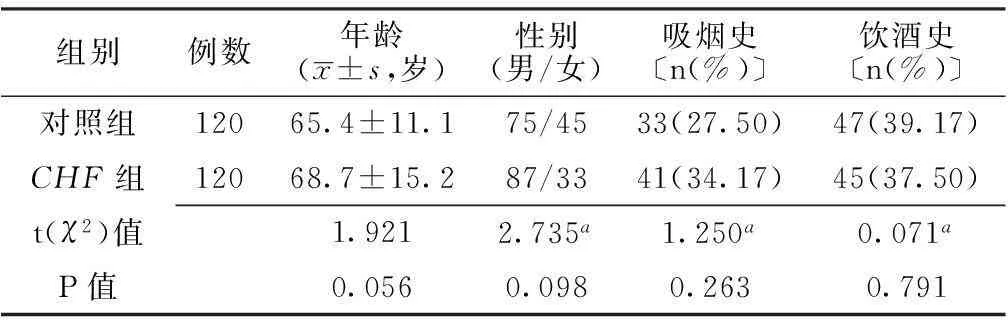
组别例数年龄(x±s,岁)性别(男/女)吸烟史〔n(%)〕饮酒史〔n(%)〕对照组12065.4±11.175/4533(27.50)47(39.17)CHF组12068.7±15.287/3341(34.17)45(37.50)t(χ2)值1.9212.735a1.250a0.071aP值0.0560.0980.2630.791
注:a为χ2值
1.2方法受试者于静息状态下(静息>30 min)抽取肘静脉血3 ml,加入预冷的含抑肽酶(500 U/ml)和10%乙二胺四乙酸30 μl的真空抗凝玻璃试管中,3 000 r/min离心10 min,取上清液。采用酶联免疫吸附试验(ELISA)检测血浆NT-proBNP水平,采用化学发光免疫测定法检测血浆T3、T4、FT3、FT4、TSH水平。采用西门子SEQUDIA心脏超声诊断仪进行二维超声心动图检查,探头频率为3~5 MHz,测量心脏各腔室大小,采用双平面辛普森法计算左心室射血分数(LVEF)。
1.3观察指标比较两组受试者及不同心功能分级CHF患者血浆甲状腺激素(T3、T4、FT3、FT4、TSH)、NT-proBNP水平及LVEF,并观察CHF患者NT-proBNP水平及LVEF与甲状腺激素水平的相关性。
根据CHF患者住院期间心血管事件发生情况分为心血管事件组42例和非心血管事件组78例,比较心血管事件组与非心血管事件组患者血浆甲状腺激素(T3、T4、FT3、FT4、TSH)、NT-proBNP水平及LVEF。其中心血管事件包括严重心力衰竭、心肌梗死再发、恶性心律失常、靶病变血管重建及心源性死亡。

2结果
2.1CHF组与对照组受试者血浆甲状腺激素、NT-proBNP水平及LVEF比较两组受试者血浆T4、FT4、TSH水平比较,差异无统计学意义(P>0.05);CHF组患者血浆T3、FT3水平及LVEF低于对照组,血浆NT-proBNP水平高于对照组,差异有统计学意义(P<0.05,见表2)。
2.2不同心功能分级CHF患者血浆甲状腺激素、NT-proBNP水平及LVEF比较不同心功能分级CHF患者血浆T4、FT4、TSH水平比较,差异无统计学意义(P>0.05);不同心功能分级CHF患者血浆T3、FT3、NT-proBNP水平及LVEF比较,差异有统计学意义(P<0.05);其中心功能Ⅲ级患者血浆FT3水平低于心功能Ⅱ级患者,血浆NT-proBNP水平高于心功能Ⅱ级患者,差异有统计学意义(P<0.05);心功能Ⅳ级患者血浆T3、FT3水平及LVEF低于心功能Ⅱ、Ⅲ级患者,血浆NT-proBNP水平高于心功能Ⅱ、Ⅲ级患者,差异有统计学意义(P<0.05,见表3)。
2.3CHF患者血浆NT-proBNP水平、LVEF与血浆甲状腺激素水平的相关性Pearson相关性分析结果显示,血浆NT-proBNP水平与血浆T3、FT3水平呈负相关(r值分别为-0.335、-0.221,P<0.05),与血浆T4、FT4、TSH水平无直线相关性(r值分别为0.047、0.027、0.015,P>0.05)。LVEF与血浆T3、FT3水平呈正相关(r值分别为0.410、0.229,P<0.05),与血浆T4、FT4、TSH水平无直线相关性(r值分别为0.085、0.087、0.004,P>0.05)。
2.4心血管事件组与非心血管事件组患者血浆甲状腺激素、NT-proBNP水平比较心血管事件组与非心血管事件组患者血浆T4、FT4、TSH水平比较,差异无统计学意义(P>0.05);心血管事件组患者血浆T3、FT3水平低于非心血管事件组,血浆NT-proBNP水平高于非心血管事件组,差异有统计学意义(P<0.05,见表4)。
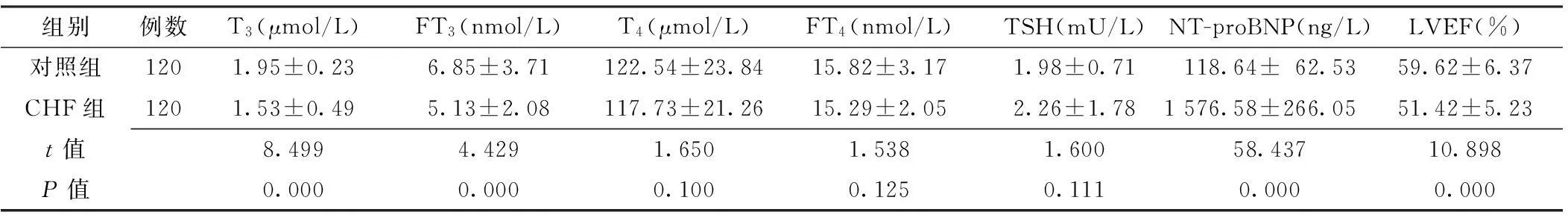
表2 CHF组与对照组受试者血浆甲状腺激素、NT-proBNP水平及LVEF比较
注:T3=三碘甲状腺原氨酸,FT3=游离三碘甲状腺原氨酸,T4=甲状腺素,FT4=游离甲状腺素,TSH=促甲状腺激素,NT-proBNP=氨基末端脑钠肽前体,LVEF=左心室射血分数

表3 不同心功能分级CHF患者血浆甲状腺激素、NT-proBNP水平及LVEF比较±s)
注:与心功能Ⅱ级比较,aP<0.05;与心功能Ⅲ级比较,bP<0.05

Table4ComparisonofplasmalevelsofthyroidhormonesandNT-proBNPbetweenCHFpatientscomplicatedwithanddidnotcomplicatewithcardiovascularevents
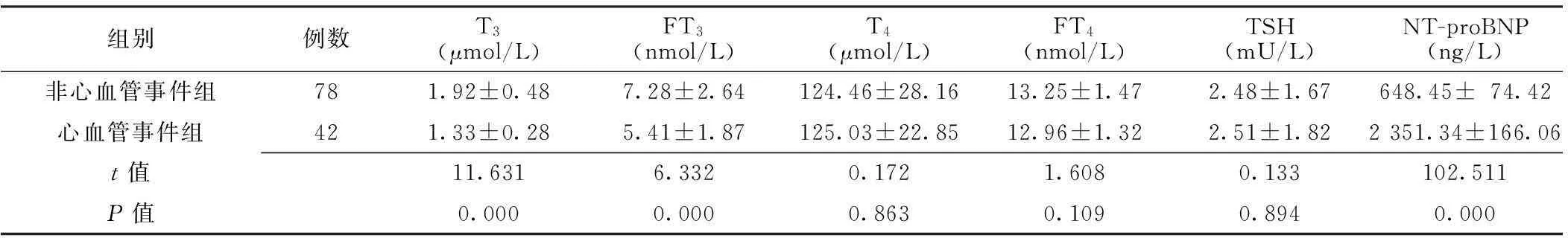
组别例数T3(μmol/L)FT3(nmol/L)T4(μmol/L)FT4(nmol/L)TSH(mU/L)NT-proBNP(ng/L)非心血管事件组781.92±0.487.28±2.64124.46±28.1613.25±1.472.48±1.67648.45±74.42心血管事件组421.33±0.285.41±1.87125.03±22.8512.96±1.322.51±1.822351.34±166.06t值11.6316.3320.1721.6080.133102.511P值0.0000.0000.8630.1090.8940.000
3讨论
心力衰竭不仅发病率高,也是心脏病患者的主要死因。CHF多因慢性原发性心肌疾病和长期心室压力和/或容量负荷过重导致心肌收缩力减弱而不能维持心排血量,是各种心血管疾病的终末阶段[6]。据统计我国中老年城乡居民CHF患病率约为0.9%,其中以老年患者多见[7]。
患者发生心力衰竭时全身性或局部性神经体液发生变化,主要包括交感神经激活、血管紧张素Ⅱ及BNP水平升高等[8]。BNP是心室肌细胞分泌的一种多肽类心脏神经激素,由32个氨基酸组成,其释放与心室压力负荷以及心室容积扩张关系密切[9]。心力衰竭时血浆BNP水平明显升高,其主要作用包括利尿及抑制肾素-血管紧张素-醛固酮系统等,对血压、血容量及心功能的维护均有重要影响。NT-proBNP无生物活性且在血浆中稳定存在,与BNP水平有良好的一致性,且较BNP更便于检测[10]。
甲状腺激素有增加Na+-K+-ATP酶及Ca2+-ATP酶活性、促进心肌细胞蛋白质合成、提高心肌收缩力等作用。心力衰竭患者甲状腺激素水平较低,从而导致心脏收缩功能下降,进一步加速疾病发展[11]。Selvaraj等[12]研究发现,血浆BNP水平与血浆T3水平呈正相关, LVEF与血浆T3水平呈负相关,且多因素logistic回归分析得出FT3是心血管疾病死亡的独立危险因素,分析原因可能如下:(1)心力衰竭时机体处于应激状态,儿茶酚胺及糖皮质激素分泌增加,抑制5′-脱碘酶合成,使T4向T3转化减少而导致血浆T3、FT3水平降低[13];(2)心力衰竭患者由于组织供氧不足、胃肠道淤血、营养物质吸收障碍、碘摄入量及甲状腺激素与球蛋白合成不足而导致甲状腺激素代谢异常[14];(3)甲状腺激素受体密度上调且与T3亲和力增强,从而导致T3水平降低[15];(4)心力衰竭发生时机体缺氧、酸中毒及心肌损伤使组织对T3利用度增加,从而导致血浆T3水平降低[16]。
本研究结果显示,CHF组患者血浆T3、FT3水平及LVEF低于对照组,NT-proBNP水平高于对照组;且在不同心功能分级CHF患者中,心功能Ⅲ级患者血浆FT3水平低于心功能Ⅱ级患者,血浆NT-proBNP水平高于心功能Ⅱ级患者;心功能Ⅳ级患者血浆T3、FT3水平及LVEF低于心功能Ⅱ、Ⅲ级患者,血浆NT-proBNP水平高于心功能Ⅱ、Ⅲ级患者;表明CHF患者的甲状腺激素水平低于正常人,血浆NT-proBNP水平高于正常人,且心功能分级越差的CHF患者,其血浆T3、FT3水平越低,血浆NT-proBNP水平越高。Pearson相关性分析结果显示,血浆NT-proBNP水平与血浆T3、FT3水平呈负相关,LVEF与血浆T3、FT3水平呈正相关。心血管事件组与非心血管事件组患者血浆T4、FT4、TSH水平间无差异,心血管事件组患者血浆T3、FT3水平低于非心血管事件组,血浆NT-proBNP水平高于非心血管事件组,表明甲状腺激素及血浆NT-proBNP水平对心血管疾病患者的预后具有一定的判断价值,但本研究未对其具体机制进行进一步分析,有待于在今后的研究中予以完善。本研究结果显示,心功能Ⅱ、Ⅲ级患者血浆T3水平间无差异,可能与检测误差有关,因此有待更严谨的研究。
综上所述,老年CHF患者血浆T3、FT3水平较低,血浆NT-proBNP水平较高,T3、FT3、NT-proBNP可作为判断CHF患者病情严重程度及预后的指标。临床应重视对老年CHF患者血浆甲状腺激素及NT-proBNP水平的监测,以改善老年CHF患者的预后及生存质量。
作者贡献:刘建飞进行实验设计与实施、资料收集整理、撰写论文、成文并对文章负责;彭宗清进行实验实施、评估、资料收集;夏豪进行质量控制及审校。
本文无利益冲突。
参考文献
[1]Chen S,Shauer A,Zwas DR,et al.The effect of thyroid function on clinical outcome in patients with heart failure[J].Eur J Heart Fail,2014,16(2):217-226.
[2]Curotto Grasiosi J,Peressotti B,Machado RA,et al.Improvement in functional capacity after levothyroxine treatment in patients with chronic heart failure and subclinical hypothyroidism[J].Endocrinol Nutr,2013,60(8):427-432.
[3]Triggiani V,Iacoviello M.Thyroid disorders in chronic heart failure:from prognostic set-up to therapeutic management[J].Endocr Metab Immune Disord Drug Targets,2013,13(1):22-37.
[4]Silva-Tinoco R,Carrasco Ortíz O,Castillo-Martínez L,et al.Persistence of thyroid hormones disorders in chronic heart failure outpatients:"hearthypothyroidism"[J].Int J Cardiol,2013,167(5):2359-2360.
[5]Du JB,Da CH,Zhao Y,et al.The role of brain natriuretic peptide and serum triiodothyronine in the diagnosis and prognosis ofchronic heart failure[J].Acta Cardiol,2012,67(3):291-296.
[6]D′Aloia A,Vizzardi E,Bugatti S,et al.Effect of short-term infusive dobutamine therapy on thyroid hormone profile and hemodynamic parameters in patients with acute worsening heart failure and low-triiodothyronine syndrome[J].J Investig Med,2012,60(6):907-910.
[7]Flores-Blanco PJ,Manzano-Fernández S,Pérez-Calvo JI,et al.Cystatin C-based CKD-EPI equations and N-Terminal pro-B-Type natriuretic peptide for predicting outcomes in acutely decompensated heart failure[J].Clin Cardiol,2015,38(2):106-113.
[8]Khand AU,Chew PG,Douglas H,et al.The effect of carvedilol on B-type natriuretic peptide and cardiac function in patients with heart failure and persistent atrial fibrillation[J].Cardiology,2015,130(3):153-158.
[9]Greene SJ,Maggioni AP,Fonarow GC,et al.Clinical profile and prognostic significance of natriuretic peptide trajectory following hospitalization for worsening chronic heart failure:findings from the ASTRONAUT trial[J].Eur J Heart Fail,2015,17(1):98-108.
[10]Liu Y,Wang Z,Xiao W,et al.Use of gated myocardial perfusion imaging to assess clinical value of xinmailong injection in chroniccongestive heart failure[J].J Tradit Chin Med,2014,34(5):555-559.
[11]Ling HZ,Flint J,Damgaard M,et al.Calculated plasma volume status and prognosis in chronic heart failure[J].Eur J Heart Fail,2015,17(1):35-43.
[12]Selvaraj A,Klein I,Danzi S,et al.Association of serum triiodothyronine with B-type natriuretic peptide and severe left ventricular diastolic dysfunction in heart failure with preserved ejection fraction[J].Am J Cardiol,2012,110(2):234-239.
[13]Gandhi PU,Szymonifka J,Motiwala SR,et al.Characterization and prediction of adverse events from intensive chronic heart failuremanagement and effect on quality of life:results from the pro-B-type natriuretic peptideoutpatient-tailored chronic heart failure therapy(PROTECT) study[J].J Card Fail,2015,21(1):9-15.
[14]Ueland T,Aukrust P,Nymo SH,et al.Novel extracellular matrix biomarkers as predictors of adverse outcome in chronic heart failure:association between biglycan and response to statin therapy in the CORONA trial[J].J Card Fail,2015,21(2):153-159.
[15]Grodin JL,Neale S,Wu Y,et al.Prognostic comparison of different sensitivity cardiac troponin assays in stable heart failure[J].Am J Med,2015,128(3):276-282.
[16]Ueland T,Aukrust P,Nymo SH,et al.Predictive value of endostatin in chronic heart failure patients with poor kidney function[J].Cardiology,2015,130(1):17-22.
(本文编辑:毛亚敏)
Changes of Thyroid Hormones and NT-proBNP and the Estimated Value on Prognosis of Elderly Patients With Chronic Heart Failure
LIUJian-fei,PENGZong-qing,XIAHao.
TheNorthDistrictofXiangyangCenteralHospital,Xiangyang441000,China
【Abstract】ObjectiveTo analyze the changes of thyroid hormones and NT-proBNP and the estimated value on prognosis of elderly patients with chronic heart failure(CHF).MethodsA total of 120 elderly patients with CHF were selected as case group in the Xiangyang Centeral Hospital from May 2012 to February 2015,including 42 cases with Ⅱ-grade cardiac function(served as A group),47 cases with Ⅲ-grade cardiac function(served as B group),31 cases with Ⅳ-grade cardiac function(served as C group);a total of 120 healthy old people admitted to this hospital for physical examination were selected as control group at the same time.Plasma levels of thyroid hormones(including T3,T4,FT3,FT4,TSH)and NT-proBNP,and LVEF were compared between case group and control group,in patients with different cardiac functional grading,and correlations between plasma levels of thyroid hormones and plasma NT-proBNP level,and LVEF were analyzed.According to the incidence of cardiovascular events,patients of case group were divided into D group(complicated with cardiovascular events,n=42)and E group(did not complicated with cardiovascular events,n=78),plasma levels of thyroid hormones and NT-proBNP,and LVEF were compared between D group and E group.ResultsNo statistically significant differences of plasma level of T4,FT4or TSH was found between case group and control group(P>0.05);plasma levels of T3and FT3,and LVEF of case group were statistically significantly lower than those of control group,while plasma NT-proBNP level of case group was statistically significantly higher than that of control group(P<0.05).No statistically significant differences of plasma level of T4,FT4or TSH was found among A,B and C groups(P>0.05);plasma FT3level of B group was statistically significantly lower than that of A group,while plasma NT-proBNP level of B group was statistically significantly higher than that of A group(P<0.05);plasma levels of T3and FT3,and LVEF of C group were statistically significantly lower than those of A group and B group,while plasma NT-proBNP level of C group was statistically significantly higher than that of A group and B group,respectively(P<0.05).Pearson correlation analysis showed that, plasma NT-proBNP level was negatively correlated with plasma level of T3(r=-0.335),of FT3(r=-0.221),respectively(P<0.05),was not linearly correlated with plasma level of T4(r=0.047),of FT4(r=0.027)or of TSH(r=0.015),respectively(P>0.05);LVEF was positively correlated with plasma level of T3(r=0.410),of FT3(r=0.229),respectively(P<0.05),was not linearly correlated with plasma level of T4(r=0.085),of FT4(r=0.087)or of TSH(r=0.004),respectively(P>0.05).No statistically significant differences of plasma level of T4,FT4or TSH was found between D group and E group(P>0.05);plasma levels of T3and FT3of D group were statistically significantly lower than those of E group,while plasma NT-proBNP level of D group was statistically significantly higher than that of E group(P<0.05).Conclusion Plasma levels of T3and FT3of elderly patients with CHF are significantly depressed,while plasma NT-proBNP level is significantly increased,T3,FT3and NT-proBNP play important roles in evaluating the severity of illness and prognosis.
【Key words】Heart failur;Thyroid hormones;N-terminal pro-B-type natriuretic peptide;Forecasting
(收稿日期:2015-09-13;修回日期:2016-01-11)
【中图分类号】R 541.6
【文献标识码】A
doi:10.3969/j.issn.1008-5971.2016.01.003
通信作者:彭宗清,441000湖北省襄阳市中心医院北区;E-mail:1845752066@qq.com
基金项目:国家自然科学基金资助项目(81270184);湖北省医学会中青年扶持计划(HW-2009BNO.018)
【编者按】近年来心力衰竭的诊断及治疗等方面的研究取得了巨大进展,但由于心力衰竭发病率、致残率及致死率较高,因此其仍是目前威胁人类健康的重大公共和社会问题之一,也是当前心血管疾病领域的热点问题和亟须解决的临床难题之一。随着我国人口老龄化进程加快,老年慢性心力衰竭患者数量在不断增多,准确评估老年慢性心力衰竭患者病情严重程度及预后对指导临床制定科学、合理、有效的治疗方案意义重大。刘建飞等所在课题组研究发现,老年慢性心力衰竭患者血浆三碘甲状腺原氨酸(T3)、游离三碘甲状腺原氨酸(FT3)水平较低,血浆氨基末端脑钠肽前体(NT-proBNP)水平较高,对老年慢性心力衰竭患者病情严重程度及预后具有一定评估价值,具有一定借鉴参考价值,敬请关注!