急性冠状动脉综合征合并2型糖尿病患者应用氯吡格雷与替格瑞洛后残余血小板高反应性及对预后影响的比较
汪敏 双东思 苏晞
急性冠状动脉综合征合并2型糖尿病患者应用氯吡格雷与替格瑞洛后残余血小板高反应性及对预后影响的比较
汪敏 双东思 苏晞
目的 比较急性冠状动脉综合征(acute coronary syndrome,ACS)合并2型糖尿病患者应用氯吡格雷和替格瑞洛的残余血小板高反应性及对预后的影响。方法选取武汉亚洲心脏病医院2013年3月至2015年3月住院的ACS合并2型糖尿病患者175例,入院后均给予标准双联抗血小板治疗,分为氯吡格雷组(153例)和替格瑞洛组(22例)。采用光比浊法测量腺苷二磷酸诱导的血小板聚集率。定义血小板最大聚集率>46.0%为残余血小板高反应性。比较两组残余血小板高反应性的差异及残余血小板高反应性对3个月预后的影响。结果氯吡格雷组残余血小板高反应性的发生率显著高于替格瑞洛组,差异有统计学意义[64.7%(99/153)比36.4%(8/22),P=0.011]。随访3个月,残余血小板高反应组发生支架内血栓事件3例(2.8%,3/107),均发生于使用氯吡格雷患者,残余血小板正常反应组无一例发生,两组的差异有统计学意义(P=0.016);两组患者的主要事件复合终点、全因死亡、心肌梗死、卒中、出血事件等发生率分别比较,差异均无统计学意义(均P>0.05)。结论 ACS合并2型糖尿病患者应用替格瑞洛较氯吡格雷显著降低治疗后的残余血小板高反应性,残余血小板高反应性增加支架内血栓风险。
急性冠状动脉综合征; 2型糖尿病; 氯吡格雷; 替格瑞洛; 残余血小板高反应性
急性冠状动脉综合征(acute coronary syndrome,ACS)是心血管疾病的急危重症。血小板在ACS中发挥重要的作用,抗血小板治疗可有效降低急性冠状动脉事件发生率,减少心血管事件死亡率[1-4]。氯吡格雷是目前ACS抗血小板治疗的基石[5],但是氯吡格雷需要经肝代谢后转化为活性药物。血小板功能测试研究显示,氯吡格雷抗血小板聚集存在很大的个体变异性[6-7]。
替格瑞洛是一种新型抗血小板药物,不需要肝代谢激活,比氯吡格雷能更有效地抑制腺苷二磷酸(adenosine diphosphate,ADP)诱导的血小板聚集。糖尿病是冠心病患者发生残余血小板高反应性的独立影响因素[8-9]。合并糖尿病的患者心血管事件风险更高。替格瑞洛较氯吡格雷理应有更大的心血管获益。但PLATO研究[10]的亚组分析发现,糖尿病患者应用替格瑞洛能显著获益,但是跟非糖尿病患者相比,差异无统计学意义,其机制不明,是否与残余血小板高反应性相关,尚未明确。本研究比较ACS合并2型糖尿病患者应用氯吡格雷与替格瑞洛后残余血小板高反应性及对预后的影响。
1 对象与方法
1.1 研究对象
选取武汉亚洲心脏病医院2013年3月至2015年3月住院的ACS(包括不稳定型心绞痛、急性ST段抬高心肌梗死、急性非ST段抬高心肌梗死)合并2型糖尿病患者175例。2型糖尿病按照2010年美国糖尿病学会(American diabetes association,ADA)糖尿病诊断标准[11]:(1)糖化血红蛋白≥6.5%; (2)空腹血糖≥7.0 mmol/L,空腹定义为至少8 h内无热量摄入;(3)口服糖耐量试验时2 h血糖≥11.1 mmol/L;(4)在伴有典型的高血糖或高血糖危象症状的患者,随机血糖≥11.1 mmol/L;在无明确高血糖时,应通过重复检测来证实标准(1)~(3)。
纳入标准:(1)ACS;(2)2型糖尿病。排除标准:(1)对氯吡咯雷禁忌,入选前24 h行溶栓治疗,未行起搏器植入增加心动过缓风险,联合使用细胞色素P4503A的强效抑制剂或诱导剂;(2)1型糖尿病;(3)酮症酸中毒;(4)乳酸酸中毒;(5)慢性肾病4期以上[估算的肾小球滤过率 (estimated glomerular filtration rate,eGFR)<30 ml/(min· 1.73 m2)];(6)纽约心脏病协会(new york heart association,NYHA)心功能Ⅳ级,血流动力学不稳定,不能平卧24 h以上;(7)需口服抗凝药。
1.2 方法
患者入院时均先顿服阿司匹林300 mg和氯吡格雷300 mg或者替格瑞洛180 mg,之后用氯吡格雷75 mg、每日1次(氯吡格雷组,153例)或者替格瑞洛90 mg、每日2次(替格瑞洛组,22例)的维持剂量治疗12个月。于清晨服药前采集肘静脉血检测血小板聚集功能,使用2支3.8 mg/dl枸橼酸钠抗凝管采血3 ml。
血小板聚集功能检测(光比浊法):采用美国Helena Laboratories公司生产的血小板聚集仪(AggRAM)进行检测分析,诱导剂为ADP,ADP最终诱导浓度为5 μmol/L,定义血小板最大聚集率>46.0%为残余血小板高反应性。
其他检测项目:入院后第2天查糖化血红蛋白,空腹血糖;左心室射血分数(left ventricular ejection fraction,LVEF);肝功能(谷丙转氨酶);血液分析(红细胞计数、白细胞计数、血小板计数),电解质(K+、Na+、Cl-);血脂,甲状腺功能(游离 T3、游离T4、促甲状腺激素);血清肌钙蛋白I。以上生化检验均使用本院检验科设备。
其他基本情况如年龄、性别、体重、身高、血压等,既往病史如高血压病、卒中、高脂血症、心力衰竭、经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI)、冠状动脉旁路移植术(coronary artery bypass grafting,CABG)、外周血管疾病等,心血管危险因素如吸烟、高血压病、血脂异常等被记录,同时所有患者进行临床随访,记录3个月主要事件(包括全因死亡、心肌梗死、卒中、支架内血栓)和出血事件的发生情况。
1.3 统计学处理
采用SPSS 22.0统计学软件进行数据分析。计量资料以均数±标准差(¯x±s)表示,组间比较采用t检验,计数资料以例数(百分率)表示,组间比较采用卡方检验。以P<0.05为差异有统计学意义。
2 结果
2.1 两组患者的基线资料比较
氯吡格雷组患者的白细胞计数显著低于替格瑞洛组[(7.72±2.51)×109/L比(9.21±3.68)×109/L,P=0.016],血清 Na+浓度显著高于替格瑞洛组[(139.48±2.16)mmol/L比(138.25±2.49)mmol/ L,P=0.015],差异均有统计学意义。两组患者的性别、年龄、身高、体重、收缩压、舒张压、既往史、血液分析、血脂、甲状腺功能、肝功能、左心室舒张末期内径、左心室射血分数等其他指标比较,差异均无统计学意义(均P>0.05,表1)。
2.2 两组患者残余血小板高反应性比较
氯吡格雷组残余血小板高反应性患者99例,占64.7%。按本院常规,血小板最大聚集率>46.0%给予氯吡格雷剂量翻倍或替换为替格瑞洛。替格瑞洛组残余血小板高反应性患者8例,占36.4%,显著低于氯吡格雷组,差异有统计学意义(P=0.011)。
2.3 残余血小板高反应性和3个月随访事件的关系
根据血小板最大聚集率>46.0%为残余血小板高反应性,将患者分为残余血小板高反应组(107例)和残余血小板正常反应组(68例)。随访3个月,残余血小板高反应组发生支架内血栓事件3例(2.8%),残余血小板正常反应组无一例发生,两组比较,差异有统计学意义(P=0.016);3例支架内血栓均发生于氯吡格雷组。两组患者3个月的主要事件复合终点、全因死亡、心肌梗死、卒中、出血事件等发生率分别比较,差异均无统计学意义(均 P>0.05,表2)。
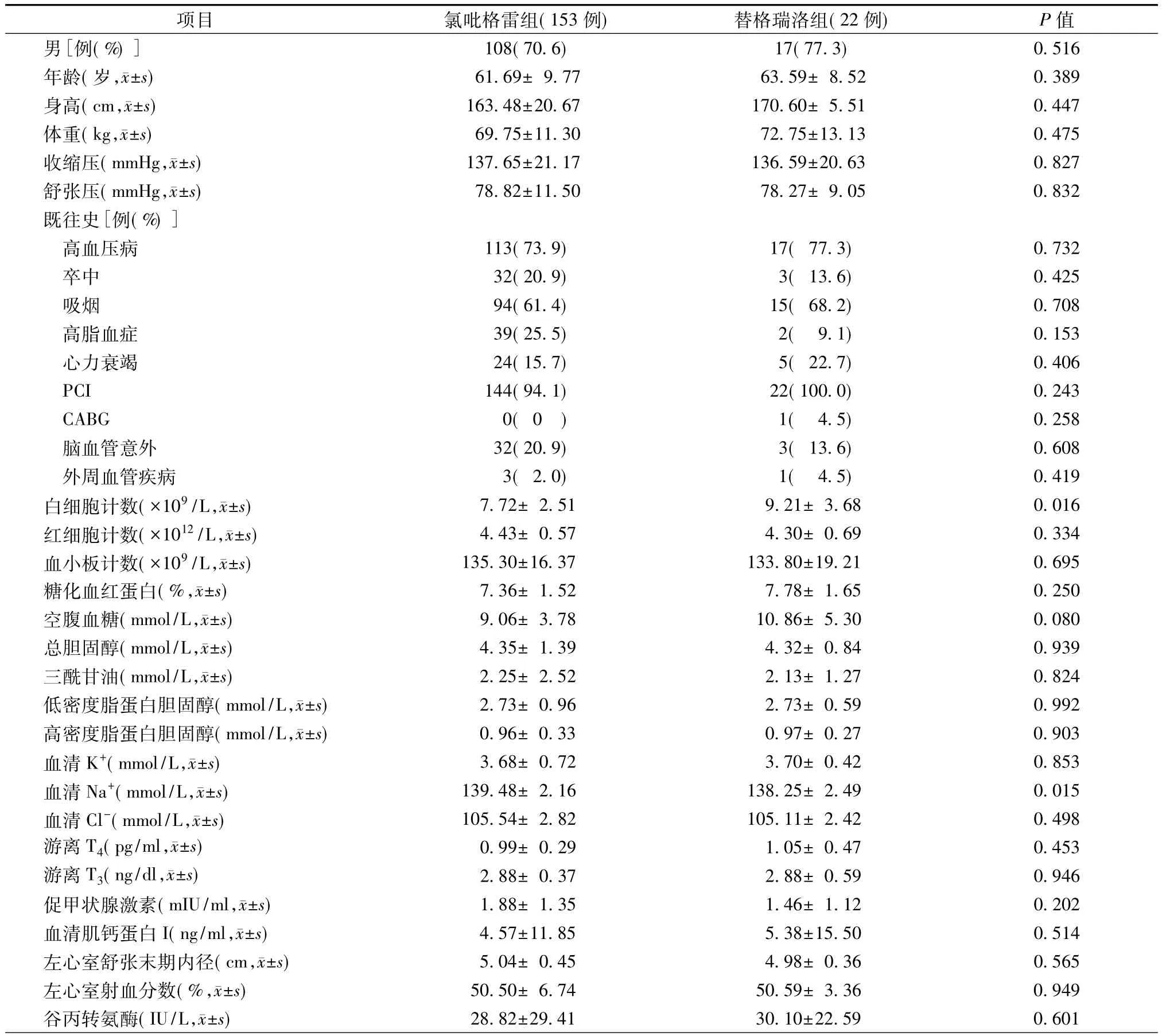
表1 两组患者的基线资料比较
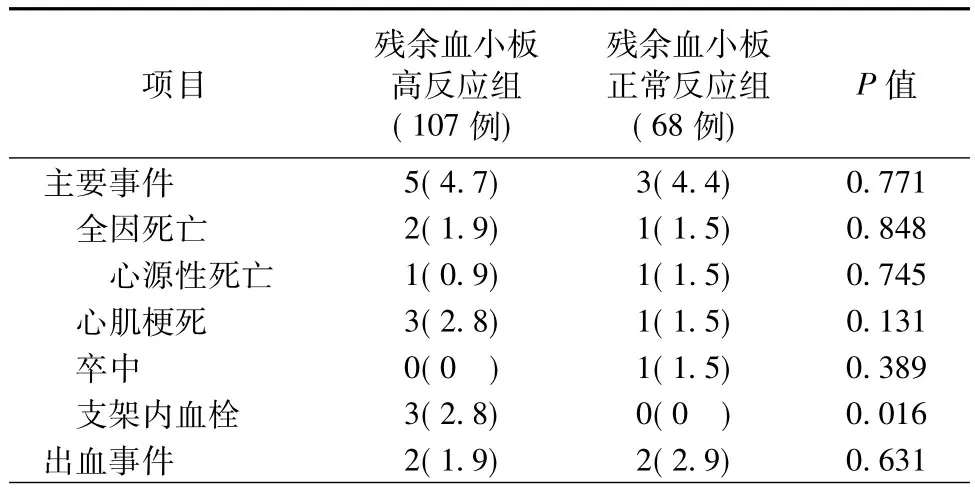
表2 残余血小板高反应性和3个月随访事件的关系[例(%)]
2.4 主要事件及临床特点
残余血小板高反应组共5例患者发生主要事件,其中3例心肌梗死合并支架内血栓,1例猝死,1例心力衰竭合并肾衰竭死亡。残余血小板正常反应组共3例患者发生主要事件,其中1例心肌梗死,1例卒中,1例室性心动过速、心室颤动死亡。8例主要事件及其临床特点见表3。
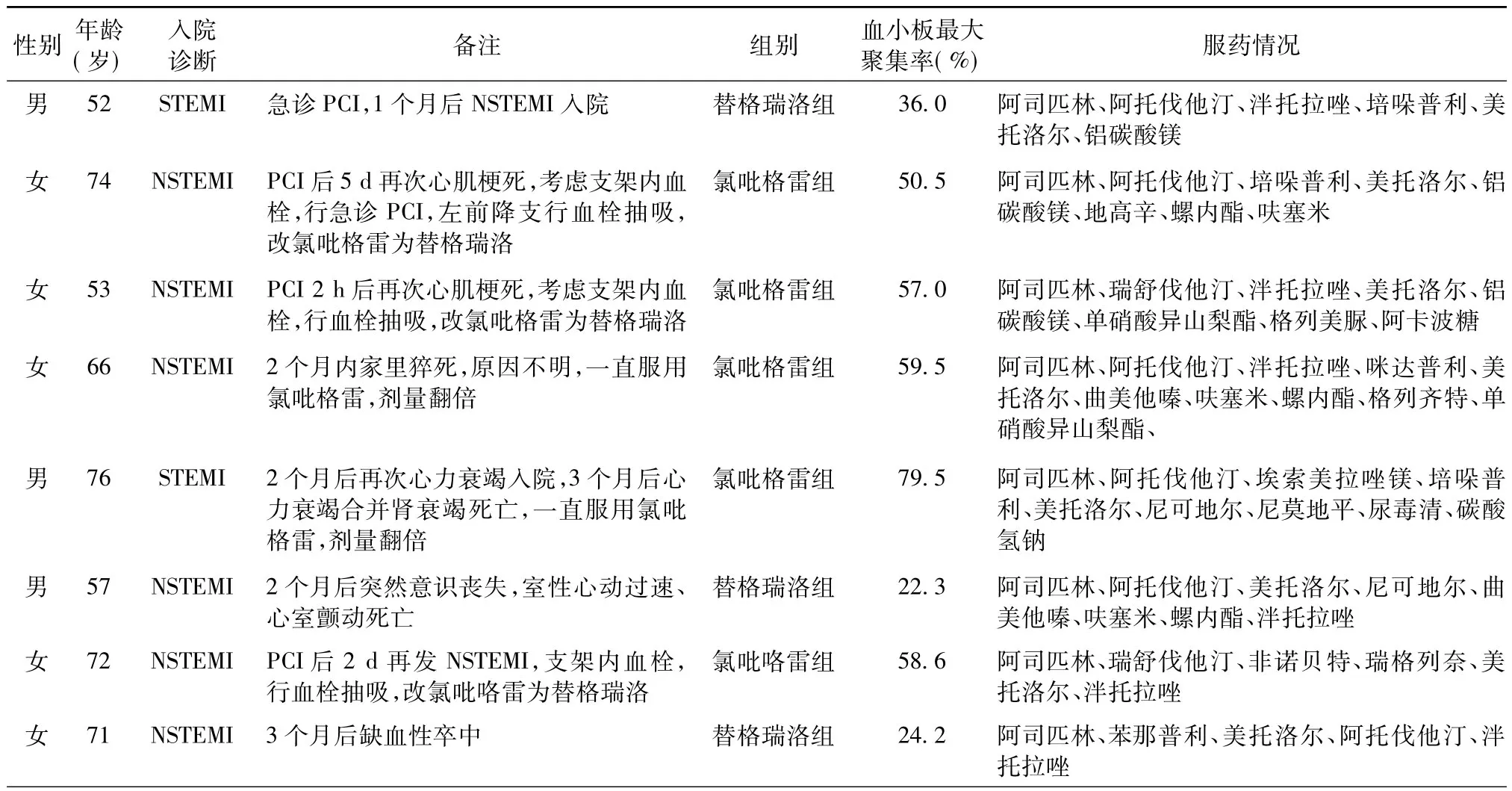
表3 8例主要事件及其临床特点
2.5 出血事件及临床特点
残余血小板高反应组和残余血小板正常反应组各2例患者发生出血事件,均分别为消化道出血或血尿。4例出血事件及其临床特点见表4。

表4 4例出血事件及其临床特点
3 讨论
ACS是心血管疾病的急危重症。血小板在ACS中发挥重要的作用,抗血小板治疗可有效地降低急性冠状动脉事件,减少心血管事件死亡率。氯吡格雷是ACS抗血小板治疗的基石,可是氯吡咯雷需要经肝代谢后转化为活性药物才能发挥抗血小板效果,而大约85%的氯吡格雷被水解为无活性的产物,只有小部分转为活性产物,CYP2C19基因在这个过程中起着关键作用[12]。但是,氯吡格雷反应的变异性是多因素的,CYP2C19基因仅仅只解释5%~12%的总变异性[8-9,13]。血小板功能测试显示,氯吡格雷抗血小板聚集表现了很大的个体变异性。糖尿病是增加残余血小板高反应性的另一个主要危险因素[8-9]。评估残余血小板高反应性的检测方法比较多,光比浊法是血小板聚集功能检测的“金标准”,虽然可重复性差,非ADP受体特异性,但其价格低廉、易于普及,是目前国内使用最为普遍的检查方法之一,有很好的实用性。本研究选择该方法评估残余血小板高反应性。
多项研究显示,即使给予负荷剂量氯吡格雷,仍有5%~44%的患者不能获得充足的抗血小板效应[14-18]。不同检测方法、不同诱导剂浓度决定了残余血小板高反应性的阈值。Cuisset等[19]使用10 μmol/L ADP作为诱导剂,将研究人群四等分,其中25%的研究对象表现为低反应,确定ADP诱导的血小板最大聚集率>70%作为临界值。最近的一项共识[20]在残余血小板高反应性的定义中指出,采用光比浊法测定5 mmol/L ADP诱导的血小板最大聚集率>46%的患者常合并严重不良心脏事件。
影响氯吡格雷残余血小板高反应性的因素包括细胞因素(降低的CYP3A代谢活性,增加ADP暴露,P2Y12路径的上调等)、基因因素(如CYP450基因多态性)、临床因素(如依从性差,ACS、糖尿病、心力衰竭、肾衰竭,体重指数增加,高龄)以及药物代谢性因素[如吸收差、代谢下降、剂量不足、药物相互作用(钙离子拮抗药、质子泵抑制药)]。Saad等[21]研究显示,采用5 mmol/L ADP诱导,糖尿病患者的平均血小板最大聚集率为22%,非糖尿病患者为11%,差异有统计学意义。Mylotte等[22]研究显示,采用5 mmol/L ADP诱导,糖尿病患者的平均血小板最大聚集率为(56.0±11.1)%。由此可见,糖尿病是残余血小板高反应性的危险因素。Mobley等[23]研究显示,糖尿病组抗血小板无反应的发生率高达40%,非糖尿病组为23%;并且,氯吡格雷治疗0~3 d后残余血小板高反应性患者所占比例仍高达40%。本研究的研究对象为ACS合并糖尿病患者,同时存在氯吡格雷用药时间过短、给予负荷剂量不足、合并使用质子泵抑制药及他汀类药物等多种因素的影响,导致氯吡格雷组的残余血小板高反应性发生率增加。残余血小板高反应性比血小板低反应性增加了缺血并发症的风险。RECLOSE 2-ACS研究[24]显示,氯吡格雷的残余血小板高反应性发生率为14%,即使增加氯吡格雷剂量或更改为噻氯匹定,血小板高反应性的发生率仍保持将近40%;残余血小板高反应组中,心脏病死亡的一级终点发生率是血小板低反应组的2倍以上,支架内血栓的发生率绝对风险增加3.2%。
研究显示,亚急性支架内血栓患者血小板反应性显著升高[25]。Müller等[14]的队列研究共纳入105例行PCI的患者,结果显示,氯吡格雷无反应者的支架内血栓发生风险更高。Cuisset等[26]的研究结果证实了该现象。CREST研究[27]结果证实,残余血小板高反应性以及不完全的P2Y12受体抑制是亚急性支架内血栓的危险因素。2007年的一项观察性研究显示,对行药物洗脱支架置入的PCI患者,给予600 mg负荷剂量的氯吡格雷后,随访6个月发现,残余血小板高反应性增加支架内血栓风险[28]。
替格瑞洛是一种新型抗血小板药物,不需要经肝代谢激活,比氯吡格雷能更有效地抑制ADP诱导的血小板聚集。本研究证实了对于ACS合并糖尿病患者,替格瑞洛显著降低血小板高反应性的发生率,并且证实了对于ACS合并糖尿病患者,残余血小板高反应性同样增加支架内血栓风险。但本研究样本量偏小,同时为观察性研究,需要更多样本的随机对照研究证实。
[1] Leon MB,Baim DS,Popma JJ,et al.A clinical trial comparing three antithrombotic-drug regimens after coronary-artery stenting.Stent Anticoagulation Restenosis Study Investigators.N Engl J Med,1998,339(23):1665-1671.
[2] Yusuf S,Zhao F,Mehta SR,et al.Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation.N Engl J Med,2001,345(7): 494-502.
[3] Wiviott SD,Braunwald E,McCabe CH,et al.Prasugrel versus clopidogrel in patients with acute coronary syndromes.N Engl J Med,2007,357(20):2001-2015.
[4] Wallentin L,Becker RC,Budaj A,et al.Ticagrelor versus clopidogrel in patients with acute coronary syndromes.N Engl J Med,2009,361(11):1045-1057.
[5] Jneid H,Anderson JL,Wright RS,et al.2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.J Am Coll Cardiol,2012,60(7):645-681.
[6] Price MJ,Coleman JL,Steinhubl SR,et al.Onset and offset of platelet inhibition after high-dose clopidogrel loading and standard daily therapy measured by a point-of-care assay in healthy volunteers.Am J Cardiol,2006,98(5):681-684.
[7] Price MJ,Baker BA,Jakubowski JA,et al.Detecting a thienopyridine effect by platelet reactivity assessment and its implications for risk stratification.J Thromb Haemost,2014,12 (4):560-563.
[8] Price MJ,Murray SS,Angiolillo DJ,et al.Influence of genetic polymorphisms on the effect of high-and standard dose clopidogrel after percutaneous coronary intervention:the GIFT (Genotype Information and Functional Testing)study.J Am Coll Cardiol,2012,59(22):1928-1937.
[9] Hochholzer W,Trenk D,Fromm MF,et al.Impact of cytochrome P450 2C19 loss-of-function polymorphism and of major demographic characteristics on residual platelet function after loading and maintenance treatment with clopidogrel in patients undergoing elective coronary stent placement.J Am Coll Cardiol,2010,55(22):2427-2234.
[10] James S,Angiolillo DJ,Cornel JH,et al.Ticagrelor vs.clopidogrel in patients with acute coronary syndromes and diabetes:a substudy from the PLATelet inhibition and patient Outcomes(PLATO)trial.Eur Heart J,2010,31(24):3006-3016.
[11] Kirkman S,Dunbar SA.American diabetes association clinical practice recommendations 2010 introduction.Diabetes Care,2010,33:S1-S2.
[12] Zhang K,Zhang J,Gao ZG,et al.Structure of the human P2Y12 receptor in complex with an antithrombotic drug.Nature,2014,509(7498):115-118.
[13] Shuldiner AR,O'Connell JR,Bliden KP,et al.Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy.JAMA,2009,302(8): 849-857.
[14] Müller I,Besta F,Schulz C,et al.Prevalence of clopidogrel nonresponders among patients with stable angina pectoris scheduled for elective coronary stent placement.Thromb Haemost,2003,89 (5):783-787.
[15] Geisler T,Langer H,Wydymus M,et al.Low response to clopidogrel is associated with cardiovascular outcome after coronary stent implantation.Eur Heart J,2006,27(20):2420-2425.
[16] Lev EI,Patel RT,Maresh KJ,et al.Aspirin and clopidogrel drug response in patients undergoing percutaneous coronary intervention:the role of dual drug resistance.J Am Coll Cardiol,2006,47(1):27-33.
[17] Gurbel PA,Bliden KP,Hayes KM,et al.The relation of dosing to clopidogrel responsiveness and the incidence of high posttreatment platelet aggregation in patients undergoing coronary stenting.J Am Coll Cardiol,2005,45(9):1392-1396.
[18] Angiolillo DJ,Fernandez-Ortiz A, Bernardo E, et al.Identification of low responders to a 300-mg clopidogrel loading dose in patients undergoing coronary stenting.Thromb Res,2005,115(1-2):101-108.
[19] Cuisset T,Frere C,Quilici J,et al.High post-treatment platelet reactivity identified low-responders to dual antiplatelet therapy at increased risk of recurrent cardiovascular events after stenting for acute coronary syndrome.J Thromb Haemost,2006,4(4):542-549.
[20] Bonello L,Tantry US,Marcucci R,et al.Consensus and Future Directions on the Definition of High On-Treatment Platelet Reactivity to Adenosine Diphosphate.J Am Coll Cardiol,2010,56(12):919-933.
[21] Saad A A,Ismail EA,Darwish YW,et al.Platelet function profile post-clopidogrel therapy in patients with type 2 diabetes undergoing coronary stentimplantation.Clin ApplThromb Hemost,2012,18(3):249-257.
[22] Mylotte D,Kavanagh GF,Peace AJ,et al.Platelet reactivity in type 2 diabetes mellitus:A comparative analysis with survivors of myocardial infarction and the role of glycaemic control.Platelets,2012,23(6):439-446.
[23] Mobley JE,Bresee SJ,Wortham DC,et al.Frequency of nonresponse antiplatelet activity of clopidogrel, during pretreatment for cardiac catheterization.Am J Cardiol,2004,93 (4):456-458.
[24] Valenti R,Marcucci R,Capodanno D,et al.Residual platelet reactivity to predict long-term clinical outcomes after clopidogrel loading in patients with acute coronary syndromes:comparison of different cutoff values by light transmission aggregometry from the responsiveness to clopidogrel and stent thrombosis2-acute coronary syndrome(RECLOSE 2-ACS) study.J Thromb Thrombolysis,2015,40(1):76-82.
[25] Barragan P,Bouvier JL,Roquebert PO,et al.Resistance to thienopyridines:clinical detection of coronary stent thrombosis by monitoring of vasodilator-stimulated phosphoprotein phosphorylation.Catheter Cardiovasc Interv,2003,59(3):295-302.
[26] Cuisset T,Frere C,Quilici J,et al.Predictive values of posttreatment adenosine diphosphate-induced aggregation and vasodilator-stimulated phosphoprotein index for stent thrombosis after acute coronary syndrome in clopidogrel-treated patients.Am J Cardiol,2009,104(8):1078-1082.
[27] Gurbel PA,Bliden KP,Samara W,et al.Clopidogrel effect on platelet reactivity in patients with stent thrombosis:results of the CREST Study.J Am Coll Cardiol,2005,46(10):1827-1832.
[28] Buonamici P,Marcucci R,Migliorini A,et al.Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis.J Am Coll Cardiol,2007,49(24):2312-2317.
High residual platelet reactivity in patients with acute coronary syndrome and diabetes mellitus receiving dual antiplatelet therapy with clopidogrel or ticagrelor and its influence on prognosis
WANG Min,SHUANG Dong-si,SU Xi.
Department of Cardiology,Wuhan Asia Heart Hospital,Wuhan 430022,China
SHUANG Dong-si,Email:sds97@163.com
ObjectiveTo observe high residual platelet reactivity in patients with acute coronary syndrome and diabetes mellitus receiving dual antiplatelet therapy with clopidogrel or ticagrelor and its influence on prognosis.MethodsA total of 175 patients with acute coronary syndrome and diabetes mellitus in Wuhan Asia Heart Hospital were included in this retrospective study,and all patients were divided into two groups:ticagrelor group(n=22)and clopidogrel group(n=153).The platelet aggregation function was tested by light transmission platelet aggregation(LTA).The high residual platelet reactivity was defined as maximum platelet aggregation rate>46.0%.The differences of high residual platelet reactivity and the effect of high residual platelet reactivity on cardiovascular events were compared between the two groups.ResultsThe number of patients with high residual platelet reactivity in the clopidogrel group were 99 patients(64.7%),and 8 patients(36.4%)in the ticagrelor group(P=0.011).For stent thrombosis developed in three months,3 patients were from the high residual platelet reaction group(n= 107),none from the normal residual platelet reaction group(n=68)(P=0.016).For bleeding events at 3 months,there were 2 patients(1.9%,2/107)from the high residual platelet reaction group and 2 patients (2.9%, 2/68) were from the normal residual platelet reaction group (P=0.631).ConclusionsTicagrelor significantly decreases high residual platelet reactivity than clopidogrel.High residual platelet reactivity increases stent thrombosis risk for ACS and type 2 diabetes mellitus.
Acute coronary syndrome; Diabetes mellitus; Clopidogrel; Ticagrelor; High residual platelet reactivity
R541.4
2016-05-18)
10.3969/j.issn.1004-8812.2016.12.004
武汉市卫计委课题(WX14C78)
430022 湖北武汉,武汉亚洲心脏病医院心内科
双东思,Email:sds97@163.com