孟鲁司特联合噻托溴铵对慢性阻塞性肺疾病患者肺功能、免疫功能及炎性因子的影响研究
吴 娟
·论著·
孟鲁司特联合噻托溴铵对慢性阻塞性肺疾病患者肺功能、免疫功能及炎性因子的影响研究
吴 娟

肺疾病,慢性阻塞性;免疫调节;炎症趋化因子类;孟鲁斯特;噻托溴铵
吴娟.孟鲁司特联合噻托溴铵对慢性阻塞性肺疾病患者肺功能、免疫功能及炎性因子的影响研究[J].实用心脑肺血管病杂志,2016,24(12):49-54.[www.syxnf.net]
WU J.Influence of montelukast combined with tiotropium bromide on pulmonary function,immune function and inflammatory cytokines of patients with chronic obstructive pulmonary disease[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2016,24(12):49-54.
慢性阻塞性肺疾病(chronic obstructive pulmonary disease,COPD)是一种慢性呼吸系统疾病,多发于老年人;COPD发病率、病死率均较高,严重影响患者生活质量和生命安全[1-2]。COPD本质上是气道、肺实质和肺血管慢性炎性反应,临床以抗炎治疗为主。吸入性糖皮质激素是治疗COPD的常用抗炎药物,但易导致口腔真菌感染及肺炎等[3]。阮军等[4]研究表明,支气管扩张剂可选择性激动支气管平滑肌上的β2受体而松弛平滑肌,继而缓解支气管痉挛及咳嗽、哮喘症状,但其整体治疗效果并不十分理想。有研究表明,孟鲁司特对半胱氨酰白三烯受体1(CysLT1)有高度的亲和性和选择性,可抑制白三烯C4(LTC4)、白三烯D4(LTD4)、白三烯E4(LTE4)与CysLT1受体的结合,且无任何受体激动活性,有利于维持COPD患者相关炎性因子平衡[5]。噻托溴铵作为长效支气管扩张剂,可有效减轻COPD患者呼吸困难等临床症状,改善患者肺功能并提高患者生活质量[6]。本研究旨在探讨孟鲁斯特联合噻托溴铵对COPD患者肺功能、免疫功能及炎性因子的影响,现报道如下。
1 资料与方法
1.1 纳入及排除标准 纳入标准:(1)符合中华医学会呼吸病学分会慢性阻塞性肺疾病学组制定的“慢性阻塞性肺疾病诊治指南(2013年修订版)”中的COPD诊断标准[7];(2)年龄30~75岁。排除标准:(1)伴有精神疾病或存在认知障碍患者;(2)存在肝肾功能严重损伤患者;(3)对本研究所用药物过敏患者;(4)近3个月内曾接受过糖皮质激素类药物治疗患者;(5)既往有肺切除术史患者;(6)无法配合完成本研究患者。
1.2 一般资料 选取广西壮族自治区南溪山医院2012年5月—2015年5月收治的COPD患者160例,采用随机数字表法分为对照组、A组、B组和C组,每组40例。对照组中男29例,女11例;年龄30~74岁,平均年龄(59.5±10.6)岁。A组中男29例,女11例;年龄32~74岁,平均年龄(60.2±10.1)岁。B组中男28例,女12例;年龄31~73岁,平均年龄(58.7±10.9)岁。C组中男27例,女13例;年龄33~75岁,平均年龄(59.3±11.2)岁。4组患者性别(χ2=0.331)、年龄(F=1.92)比较,差异无统计学意义(P>0.05),具有可比性。本研究经医院伦理委员会审核批准,患者及其家属均知情同意并签署知情同意书。
1.3 方法 对照组患者给予常规治疗,即予以抗生素治疗,哮喘严重患者在低流量持续吸氧同时给予止咳药〔按需给予硫酸沙丁胺醇(Glaxo Wellcome S.A生产,国药准字J20110040)雾化吸入治疗,0.1~0.2 mg/次,1次/6 h,治疗15 d后若患者肺部哮鸣音仍未减轻、肺功能未见明显改善则酌情重复吸入硫酸沙丁胺醇0.1 mg/次,1次/4 h,但重复吸入次数要≤8次/d〕。在常规治疗基础上,A组患者给予孟鲁司特片(Merck Sharp Dohme Ltd生产,国药准字J20070058)口服,10 mg/次,1次/d;B组患者给予噻托溴铵雾化吸入(浙江仙琚制药股份有限公司生产;国药准字H200902279),18 μg/次,1次/d;C组患者给予孟鲁司特片口服联合噻托溴铵雾化吸入,用法、用量与A、B组相同。4组患者均连续治疗3个月。

2 结果
2.1 肺功能指标 治疗前4组患者FEV1%和FEV1/FVC比较,差异无统计学意义(P>0.05)。治疗后4组患者FEV1%和FEV1/FVC比较,差异有统计学意义(P<0.05);其中A、B、C组患者FEV1%和FEV1/FVC高于对照组,C组患者FEV1%和FEV1/FVC高于A、B组,差异有统计学意义(P<0.05)。A、B、C组患者治疗后FEV1%和FEV1/FVC高于治疗前,差异有统计学意义(P<0.05),而对照组患者治疗前后FEV1%和FEV1/FVC比较,差异无统计学意义(P>0.05,见表1)。
2.2 6分钟步行距离和Borg评分 治疗前4组患者6分钟步行距离和Borg评分比较,差异无统计学意义(P>0.05)。治疗后4组患者6分钟步行距离和Borg评分比较,差异有统计学意义(P<0.05);其中A、B、C组患者6分钟步行距离长于对照组,Borg评分低于对照组,C组患者6分钟步行距离长于A、B组,Borg评分低于A、B组,差异有统计学意义(P<0.05)。A、B、C组患者治疗后6分钟步行距离长于治疗前,Borg评分低于治疗前,差异有统计学意义(P<0.05),而对照组患者治疗前后6分钟步行距离和Borg评分比较,差异无统计学意义(P>0.05,见表2)。
2.4 血清炎性因子水平 治疗前4组患者血清IL-6、CRP和APN水平比较,差异无统计学意义(P>0.05)。治疗后4组患者血清IL-6、CRP和APN水平比较,差异有统计学意义(P<0.05);其中A、B、C组患者血清IL-6、CRP、APN水平低于对照组,C组患者血清IL-6、CRP、APN水平低于A、B组,差异有统计学意义(P<0.05)。4组患者治疗后血清IL-6、CRP、APN水平低于治疗前,差异有统计学意义(P<0.05,见表4)。
表1 4组患者治疗前后肺功能指标比较
注:FEV1%=第1秒用力呼气容积占预计值百分比,FEV1/FVC=第1秒用力呼气容积与用力肺活量比值;与对照组比较,aP<0.05;与A组比较,bP<0.05;与B组比较,cP<0.05
表2 4组患者治疗前后6分钟步行距离和Borg评分比较
注:Borg=伯格呼吸困难评分量表;与对照组比较,aP<0.05;与A组比较,bP<0.05;与B组比较,cP<0.05
表3 4组患者治疗前后免疫功能指标比较
注:与对照组比较,aP<0.05;与A组比较,bP<0.05;与B组比较,cP<0.05
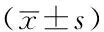
Table 4 Comparison of serum inflammatory cytokines levels among the four groups before and after treatment
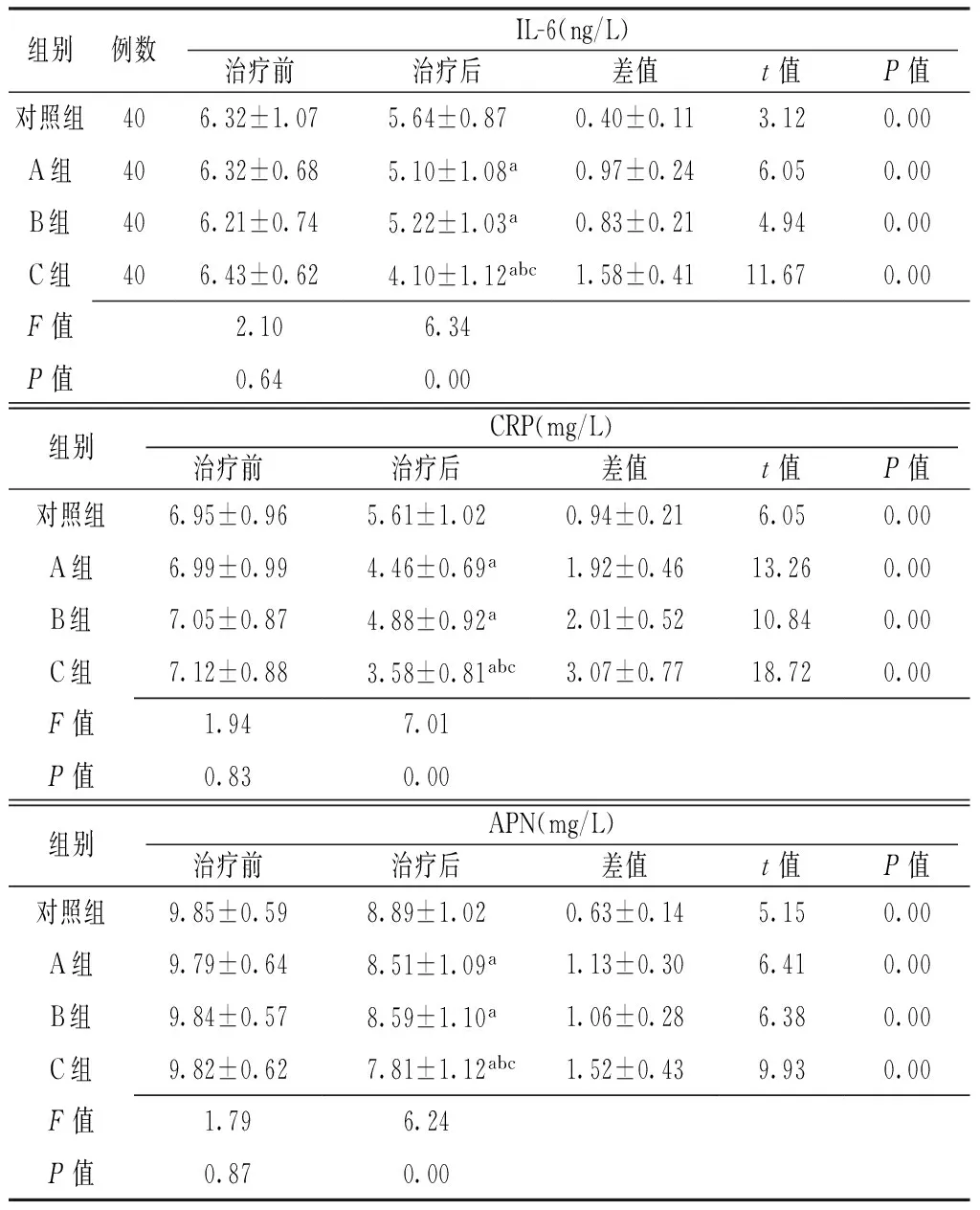
组别例数IL-6(ng/L)治疗前治疗后差值t值P值对照组406.32±1.075.64±0.870.40±0.113.120.00A组406.32±0.685.10±1.08a0.97±0.246.050.00B组406.21±0.745.22±1.03a0.83±0.214.940.00C组406.43±0.624.10±1.12abc1.58±0.4111.670.00F值2.106.34P值0.640.00组别CRP(mg/L)治疗前治疗后差值t值P值对照组6.95±0.965.61±1.020.94±0.216.050.00A组6.99±0.994.46±0.69a1.92±0.4613.260.00B组7.05±0.874.88±0.92a2.01±0.5210.840.00C组7.12±0.883.58±0.81abc3.07±0.7718.720.00F值1.947.01P值0.830.00组别APN(mg/L)治疗前治疗后差值t值P值对照组9.85±0.598.89±1.020.63±0.145.150.00A组9.79±0.648.51±1.09a1.13±0.306.410.00B组9.84±0.578.59±1.10a1.06±0.286.380.00C组9.82±0.627.81±1.12abc1.52±0.439.930.00F值1.796.24P值0.870.00
注:IL-6=白介素6,CRP=C反应蛋白,APN=脂联素。与对照组比较,aP<0.05;与A组比较,bP<0.05;与B 组比较,cP<0.05
2.5 不良反应发生情况 治疗期间,B组患者出现口干2例,C组患者出现口干4例,均能耐受;4组患者均未出现严重不良反应。
3 讨论
COPD为呼吸系统常见病之一,好发于中老年人群,其主要发病机制为多种炎性因子引起气道变态反应,进而导致慢性气道炎症[9],主要表现为进行性发展的气道呼吸气流受限。目前,临床多采用β2-受体激动剂或特异性抗胆碱药物治疗COPD,其可有效扩张支气管并缓解哮喘等临床症状。本研究旨在探讨孟鲁司特联合噻托溴铵对COPD患者肺功能、免疫功能及炎性因子的影响,为临床有效治疗COPD提供参考。
孟鲁司特属白三烯受体拮抗剂,可有效阻断白三烯的生物学效应,抑制气道炎性细胞增殖及聚集,促进白细胞凋亡,可有效改善COPD患者肺功能并降低COPD急性发作频率[10]。噻托溴铵是一种支气管扩张剂,可选择性阻断COPD患者气道平滑肌M受体,且作用时间可长达24 h,具有扩张支气管作用。此外,噻托溴铵不良反应的发生风险较低,安全性较高,多数患者可坚持规律使用[11]。
白三烯B4(LTB4)为强效炎性递质,是由淋巴细胞、中性粒细胞等多种炎性细胞分泌的趋化因子之一。王晓晟等[12]研究表明,LTB4参与了气道炎性细胞聚集、活化,与COPD的发生发展密切相关,其可通过促进相关腺体分泌和支气管平滑肌收缩、增加血管通透性而加重炎性反应。孟鲁司特具有类似毒蕈碱受体亚型M1~M5的亲和力,可通过抑制支气管平滑肌M3受体而发挥扩张支气管作用,且其对CysLT1受体具有高度亲和性和选择性,可对白三烯受体产生拮抗作用,有利于抑制气道炎性细胞增殖并促进白细胞凋亡。TSOUMAKIDOU等[13]研究表明,Th1/Th2细胞失衡与COPD的发生和发展密切相关。IL-6主要由Th2细胞分泌产生,参与体液免疫细胞的增殖、分化,与COPD患者气流受限密切相关[14],因此临床常将IL-6作为衡量COPD患者Th1/Th2细胞是否失衡的主要指标[15]。CRP是一种炎性反应急性时相蛋白,是反映COPD患者炎性反应的主要指标。APN为脂肪细胞分泌的蛋白,主要参与机体糖代谢与脂代谢。ORABY等[16]研究表明,COPD患者常出现气流受限、体质指数降低和骨骼肌耗损现象,可导致患者出现活动受限等,严重影响患者的生活质量。
FEV1%是综合评估患者肺通气功能、气道阻塞程度、气道反应及肺功能的主要指标[17]。本研究结果显示,治疗后A、B、C组患者FEV1%和FEV1/FVC高于对照组、治疗前,6分钟步行距离长于对照组、治疗前,Borg评分低于对照组、治疗前;C组患者FEV1%和FEV1/FVC高于A、B组,6分钟步行距离长于A、B组,Borg评分低于A、B组,表明孟鲁司特联合噻托溴铵可有效改善COPD患者肺功能,缓解患者临床症状,促进患者康复,与糜晓光[18]研究结果一致。孟鲁司特与噻托溴铵的药理作用机制不同,两种药物联用具有协同作用,可有效改善COPD患者肺功能、免疫功能并降低血清炎性因子水平。本研究结果还显示,4组患者治疗期间均未出现严重不良反应,表明孟鲁司特联合噻托溴铵治疗COPD的安全性较高。
综上所述,孟鲁司特联合噻托溴铵可有效改善COPD患者肺功能和免疫功能,减轻患者炎性反应,且安全性较高,有利于促进患者康复,值得临床推广应用。但本研究样本量较小,仍需在今后的研究中进一步扩大样本量进行深入探讨。
本文无利益冲突。
[1]李强,邹小新,饶常红,等.孟鲁司特联合噻托溴铵治疗慢性阻塞性肺疾病疗效的研究[J].重庆医学,2013,42(19):2278-2280.
[2]席与斌,郭小芙,吴允孚,等.噻托溴铵联合孟鲁司特治疗慢性阻塞性肺疾病急性加重期并发呼吸衰竭的疗效观察[J].中国血液流变学杂志,2014,24(3):398-399,424.
[3]简锦妮,李芳.噻托溴铵联合孟鲁司特对COPD急性发作期夜间呼吸困难的疗效观察[J].吉林医学,2013,34(14):2695-2696.
[4]阮军,吴友茹,缪李丽,等.NIPPV治疗AECOPD伴Ⅱ型呼吸衰竭的Meta分析[J].四川医学,2015,36(7):981-986.
[5]袁北芳,任立红.维生素D及其受体的免疫调节作用研究进展[J].国际免疫学杂志,2014,37(1):52-56.
[6]杜舒婷, 邢彬,丁连明,等.肺康复运动联合舒利迭与噻托溴铵对中重度慢性阻塞性肺疾病患者症状、运动耐力和肺功能的影响[J].中国运动医学杂志,2014,33(2):104-108.
[7]中华医学会呼吸病学分会慢性阻塞性肺疾病学组.慢性阻塞性肺疾病诊治指南(2013年修订版)[J].中华结核和呼吸杂志,2013,36(4):255-264.
[8]RINALDI M,LEHOUCK A,HEULENS N,et al.Antielastin B-cell and T-cell immunity in patients with chronic obstructive pulmonary disease[J].Thorax,2012,67(8):694-700.
[9]STRICKLAND S L,RUBIN B K,DRESCHER G S,et al.AARC clinical practice guideline:effectiveness of nonpharmacologic airway clearance therapies in hospitalized patients[J].Respir Care,2013,58(12):2187-2193.
[10]ZUHLKE IE, KANNIESS F, RICHTER K, et al.Montelukast attenuates the airway response to hypertonic saline in moderate-to-severe COPD.[J].Eur Respir J, 2003, 22(6):926-930.
[11]INCORVAIA C, RIARIOSFORZA G G, PRAVETTONI C,et al.Impairment of small airways in COPD patients with frequent exacerbations and effects of treatment with tiotropium.[J].Int J Chron Obstruct Pulmon Dis, 2007, 3(1):123-126.
[12]王晓晟,李敏,康筱玲,等.慢性阻塞性肺疾病患者肺功能分组的临床特征和治疗反应比较[J].中华结核和呼吸杂志,2015,38(12):901-906.
[13]TSOUMAKIDOU M,BOULOUKAKI I,THIMAKI K,et al.Innate immunity proteins in chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis[J].Exp Lung Res,2010,36(6):373-380.
[14]AL-MARAMHY H,ABDELRAHMAN A I,SAWALHI S.Resistin is not an appropriate biochemical marker to predict severity of acute pancreatitis:a case-controlled study[J].World J Gastroenterol,2014,20(41):15351-15357.
[15]KELLY E,OWEN C A,PINTO-PLATA V,et al.The role of systemic inflammatory biomarkers to predict mortality in chronic obstructive pulmonary disease[J].Expert Rev Respir Med,2013,7(1):57-64.
[16]ORABY S S,AHMED E S,FARAG T S,et al.Adiponectin as inflammatory biomarker of chronic obstructive pulmonary disease[J].Egy J Chest Dis Tuber,2014,63(3):583-587.
[17]张淼,陶洪臣,李月球,等.慢性阻塞性肺疾病患者体内游离免疫球蛋白轻链的表达及其意义[J].中华结核和呼吸杂志,2013,36(12):945-949.
[18]糜晓光.孟鲁司特联合噻托溴铵对稳定期COPD患者肺功能与呼吸困难症状的影响[J].中国实用医刊,2015,10(20):20-22.
(本文编辑:李越娜)
Influence of Montelukast Combined with Tiotropium Bromide on Pulmonary Function,Immune Function and Inflammatory Cytokines of Patients with Chronic Obstructive Pulmonary Disease
WUJuan.
NanxiMountainHospitalofGuangxiZhuangAutonomousRegion,Guilin541002,China
Objective To explore the influence of montelukast combined with tiotropium bromide on pulmonary function,immune function and inflammatory cytokines of patients with chronic obstructive pulmonary disease(COPD).Methods A total of 160 patients with COPD were selected in Nanxi Mountain Hospital of Guangxi Zhuang Autonomous Region from May 2012 to May 2015,and they were divided into control group,A group,B group and C group,each of 40 cases.Patients of control group received conventional treatment,patients of A group received oral montelukast tablets,patients of B group received aerosol inhalation of tiotropium bromide,while patients of C group received oral montelukast tablets combined with aerosol inhalation of tiotropium bromide;all of the four groups continuously treated for 3 months.Index of pulmonary function(including FEV1% and FEV1/FVC),6-minute walking distance,Borg score,T-lymphocyte subsets(CD+3cell percentage,CD+4cell percentage,CD+8cell percentage and CD+4/CD+8cell ratio)and serum inflammatory cytokines(including IL-6,CRP and APN)levels before and after treatment were compared among the four groups,incidence of adverse reactions during the treatment was observed.Results No statistically significant differences of FEV1% or FEV1/FVC was found among the four groups before treatment(P>0.05);after treatment,FEV1% and FEV1/FVC of A group,B group and C group were statistically significantly higher than those of control group and those before treatment,FEV1% and FEV1/FVC of C group were statistically significantly higher than those of A group and B group(P<0.05),while no statistically significant differences of FEV1% or FEV1/FVC of control group was found compared with those before treatment(P>0.05).No statistically significant differences of 6-minute walking distance or Borg score was found among the four groups before treatment(P>0.05);after treatment,6-minute walking distance of A group,B group and C group was statistically significantly longer than that of control group and that before treatment,Borg score of A group,B group and C group was statistically significantly lower than that of control group and that before treatment,6-minute walking distance of C group was statistically significantly longer than that of A group and B group,respectively,Borg score of C group was statistically significantly lower than that of A group and B group,respectively(P<0.05),while no statistically significant differences of 6-minute walking distance or Borg score of control group was found compared with those before treatment(P>0.05).No statistically significant differences of CD+3cell percentage,CD+4cell percentage,CD+8cell percentage or CD+4/CD+8cell ratio was found among the four groups before treatment(P>0.05);after treatment,CD+3cell percentage,CD+4cell percentage,CD+8cell percentage and CD+4/CD+8cell ratio of A group,B group and C group were statistically significantly higher than those of control group and those before treatment,CD+3cell percentage,CD+4cell percentage,CD+8cell percentage and CD+4/CD+8cell ratio of C group were statistically significantly higher than those of A group and B group(P<0.05),while no statistically significant differences of CD+3cell percentage,CD+4cell percentage,CD+8cell percentage or CD+4/CD+8cell ratio of control group was found compared with those before treatment(P>0.05).No statistically significant differences of serum level of IL-6,CRP or APN was found among the four groups before treatment(P>0.05);after treatment,serum levels of IL-6,CRP and APN of A group,B group and C group were statistically significantly lower than those of control group and those before treatment,serum levels of IL-6,CRP and APN of C group were statistically significantly lower than those of A group and B group,serum levels of IL-6,CRP and APN of control group were statistically significantly higher than those before treatment(P<0.05).No one of the four groups occurred any serious adverse reactions during the treatment.Conclusion Montelukast combined with tiotropium bromide can effectively improve the pulmonary function and immune function,relive the inflammatory reaction of patients with COPD,is safe and helpful to promote the recovery.
Pulmonary disease,chronic obstructive;Immunomodulation;Chemokines;Montelukast;Tiotropium bromide
541002广西壮族自治区桂林市,广西壮族自治区南溪山医院
R 563.9
A
10.3969/j.issn.1008-5971.2016.12.013
2016-08-23;
2016-11-13)

