人工破膜术对分娩结局及母婴的影响
人工破膜术对分娩结局及母婴的影响
刘振荣1,谢娟2
(1.徐州市铜山区中医院 妇产科,江苏 徐州 221116;2.南华大学附属第三医院妇产科,湖南 衡阳 421001)
摘要:目的探讨人工破膜和胎膜自然破裂对分娩结局以及母婴的影响。方法对正常分娩的初产妇100例临床资料进行回顾分析,将实施人工破膜的产妇50例设为治疗组;另50例胎膜自然破裂产妇设为对照组,比较2组产妇的分娩结局、羊水性状、经阴道分娩各产程时间、产后2 h出血量及分娩后并发症发生情况,并比较2组新生儿窒息、产瘤的发生率及并发症情况。结果治疗组产妇的剖宫产率明显低于对照组(P<0.05);治疗组产妇阴道分娩率明显高于对照组(P<0.05);治疗组新生儿窒息的发生率明显低于对照组(P<0.05);治疗组产妇羊水污染的发生率明显低于对照组(P<0.05),而新生儿产瘤率高于对照组(P<0.05);治疗组产妇分娩后并发症及新生儿并发症发生率明显低于对照组(P<0.05)。结论人工破膜分娩可加速产妇产程进展,提高自然分娩率,并可有效改善分娩结局。
关键词:胎膜自然破裂;人工破膜;分娩结局;新生儿窒息
DOI:10.13463/j.cnki.cczyy.2015.06.069
中图分类号:R271.9文献标志码:A
文章编号:2095-6258(2015)06-1285-03
基金项目:湖南省教育厅科技计划项目(13B098)。
作者简介:刘振荣(1971-),女,大学本科,副主任医师,主要从事妇产科疾病研究。
收稿日期:(2015-08-31)

Artificial rupture of membrane on birth outcomes and the maternal and child health
LIU Zhenrong1, XIE Juan2
(1.Department of Obstetrics and Gynecology, Tongshan District Hospital of Traditional Chinese Medicine,
Xuzhou 221116, Jiangsu Province, China;
2.Department of Obstetrics and Gynecology, The Third Hospital Affiliated to University of South China,
Hengyang 421001, Hunan Province, China)

Abstract:ObjectiveTo explore the effect of artificial rupture of membrane and natural rupture of membrane on the birth outcomes and the maternal and child health. MethodsThe clinical materials of 100 primipara were retrospectively analyzed, among which 50 cases performed with artificial rupture of membrane were served as the observation group, while 50 cases with natural rupture of membrane were served as the control group. The birth outcomes, amniotic fluid character, each birth process time through vaginal delivery, amount of bleeding 2h after delivery, and complications in the two groups were compared. The occurrence rate of neonatal asphyxia and caput succedaneum, and the complications in the two groups were compared. ResultsThe cesarean section rate in the observation group was significantly lower than that in the control group (P<0.05). The vaginal deliver rate in the observation group was significantly higher than that in the control group (P<0.05). The amniotic fluid pollution rate in the observation group was significantly lower than that in the control group (P<0.05), while the neonatal caput succedaneum rate was significantly higher than that in the control group (P<0.05). The occurrence rates of postpartum complications and neonatal complications in the observation group were significantly higher than those in the control group (P<0.05). ConclusionThe artificial rupture of membrane can accelerate the birth process progress, enhance the natural delivery rate, and effectively improve the birth outcomes.
Keywords:natural rupture of membrane; artificial rupture of membrane; birth outcomes; neonatal asphyxia
胎膜自然破裂是正常分娩胎儿娩出前胎膜发生的自然破裂,是一种生理状态分娩下的胎膜破裂[1]。人工破膜是利用人工的方法刺破胎膜的手术操作,在产科常用,对产程进展起到明显的促进作用[2]。实施人工破膜还可在早期对产妇的羊水情况进行观察,了解产妇羊水胎粪污染的程度、胎儿宫内窘迫程度,使新生儿窒息率明显降低[3]。有研究[4]证实,人工破膜分娩对缩短产程及降低妊娠不良结局均十分有利。另有学者[5]认为,在分娩活跃早期行人工破膜不仅可使产程加速,还有利于降低新生儿窒息的发生率。本研究对比了人工破膜和胎膜自然破裂对分娩结局及母婴预后的影响。现将结果报告如下。
1资料与方法
1.1一般资料对2013年1月—2014年12月于我院正常分娩的初产妇100例临床资料进行回顾分析,其中实施人工破膜的产妇50例设为治疗组,年龄23~35岁,平均(28.6±2.2)岁,孕38~42周,平均(40.2±1.0)周,胎儿体质量2.7~4.5 kg,平均(3.5±0.5) kg;另50例胎膜自然破裂产妇设为对照组,年龄22~36岁,平均(28.1±2.4)岁,孕37~41周,平均(39.5±0.8)周,胎儿体质量2.8~4.3 kg,平均(3.4±0.6) kg。2组产妇经B超检查显示均为单胎、头位,纳入本研究的产妇均无脐带先露、头盆不称、产道异常等妊娠并发症。本研究经医院伦理委员会认可,产妇以及家属均事先知情并同意接受研究。1.2治疗方法对照组待产产妇等待胎膜自然破裂分娩,待产过程中不给予其他干预措施。治疗组产妇在宫口开大3~4 cm时实施人工破膜,人工破膜具体操作如下:产前嘱产妇排空膀胱,取截石位,常规消毒,当宫缩规律、宫颈口明显扩张至3 cm时,可对产妇实行人工破膜处理,人工破膜选择在宫缩间歇期及下次宫缩开始前进行,将9号针头在宫缩间歇期即2次宫缩之间送入阴道内,利用9号针头刺破羊膜囊,刺破过程中注意保持适度的破口大小,将有齿钳伸入阴道内钳夹住胎膜并将其撕破,胎膜撕破后将手伸入阴道内,不仅利于羊水的缓慢流出,还可使胎膜紧贴胎头表面,羊水流出过程中医生需倾听胎心音、胎动情况,若2次宫缩后,胎儿出现胎头下降并进入盆腔内,且无脐带脱垂的发生,此时医生可缓慢退出手;破膜完成后嘱咐产妇放平臀部,并采用胎心监护仪持续监测产妇的宫缩情况及胎心音变化情况。若破膜后产妇出现羊水污染,可结合产妇产程进展情况制定分娩计划。1.3观察指标采用Apgar评分法对2组新生儿窒息情况进行评分,比较2组产妇的分娩结局、各产程时间、产后2 h出血量及分娩后并发症情况[6]。对2组产妇的羊水污染情况进行判断[7]。对2组新生儿窒息发生率、产瘤发生率进行比较[8]。1.4统计学方法研究数据采用SPSS 13.0统计学软件分析,计量资料用均数±标准差(±s)表示,计数资料以百分比表示,2组间计量资料比较进行t检验,计数资料比较采用χ2检验,P<0.05 表示差异有统计学意义。
2结果
2.12组新生儿1 min Apgar评分情况及新生儿窒息发生率比较见表1。

表1 2组新生儿1min Apgar评分情况及新生儿窒息发生率比较( n=50)例(%)
注:与对照组比较,#P<0.05
2.22组产妇的分娩结局比较见表2。
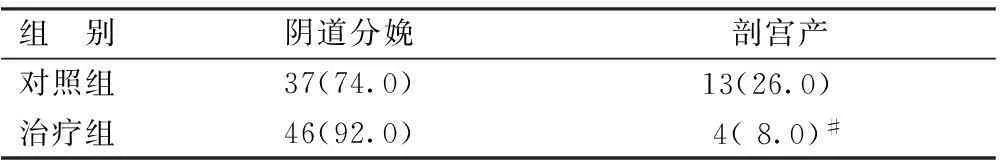
表2 2组产妇的分娩结局比较( n=50) 例(%)
注:与对照组比较,#P<0.05
2.32组产妇分娩后羊水污染情况及新生儿产瘤情况比较见表3。
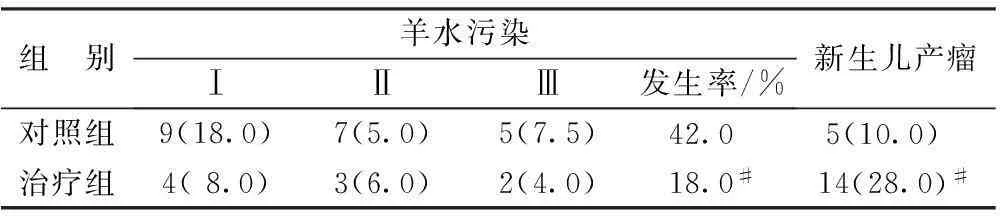
表3 2组产妇分娩后羊水污染情况及新生儿产瘤情况比较( n=50)例(%)
注:与对照组比较,#P<0.05
2.42组母婴并发症情况比较治疗组产妇分娩后并发症及新生儿并发症发生率显著低于对照组(P<0.05)。
3结语
人工破膜在活跃早期应用的主要作用机制是增加前列腺素、缩短宫颈全开时间、增强宫缩、缩短产程等,对于胎膜自然破裂前出现羊水污染的产妇,及时行人工破膜可减少胎儿宫内窘迫、窒息等并发症的发生[9-15]。本研究结果提示,人工破膜术在活跃早期的应用具有缩短产程,提高自然分娩率,降低新生儿窒息率及母婴并发症发生率等优势,但可增加新生儿产瘤发生概率,临床应根据产妇具体情况选择合适的分娩破膜方式。
参考文献:
[1]苗娜.两种破膜方式结合自由体位待产对分娩结局及母儿的影响[D].山东大学,2014.
[2]何丽平,李静,陈春玲,等.不同时机人工破膜对分娩结局的影响[J].中国医药指南,2012,10(18):213-215.
[3]郝丽萍.产妇胎膜破裂时间对产程的影响300例临床观察[J].山西职工医学院学报,2013,23(2):39-40.
[4]乔莉,张永红.活跃期人工破膜对分娩结局的影响[J].中国实用护理杂志,2011,27(8):58-59.
[5]陈巧玲.88例活跃期人工破膜的临床观察及护理[J].医学理论与实践,2011,24(23):2880-2881.
[6]DUNJA T, TIHOMIR V. Preterm and premature rupture of membranes in pregnancies after in vitro fertilization[J]. Medicinski Pregled, 2010, 67(58): 7-8.
[7]SAHHAF F, ABBAS`ALIZADEH F, H. Effect of Uterine Contraction and Amniotomy on Fetal Cardiotocograph[J]. Pakistan Journal of Biological Sciences, 2010, 13(1): 783-790.
[8]MELAMED N, HADAR E, BEN-HAROUSH A, et al. Factors affecting the duration of the latency period in preterm premature rupture of membranes[J]. The Journal of Maternal-fetal & Neonatal Medicine : the Official Journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians, 2009, 22(11): 1051-1056.
[9]GABBAY-BENZIV R, MAMAN M, WIZNITZER A, et al. Umbilical cord prolapse during delivery - risk factors and pregnancy outcome: a single center experience[J]. The Journal of Maternal-fetal & Neonatal Medicine : the Official Journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians, 2014, 27(1): 14-17.
[10]SIMPSON K R, JAMES D C. Efficacy of intrauterine resuscitation techniques in improving fetal Oxygen status during labor[J]. Obstetrics and Gynecology, 2005, 105(6): 1362-1368.
[11]袁雪莲,陈杰.人工破膜对产程进展及分娩结局的影响[J].中国保健营养(中旬刊),2012(4):134.
[12]彭红,王彩霞.活跃早期人工破膜对产程的影响[J].中国医学创新,2012,9(15):26-27.
[13]张慧珠,韩田骏,刘妍,等.360例初产妇应用人工破膜的临床效果观察[J].中国妇幼保健,2009,24(22):3080-3081.
[14]李建敏.活跃早期人工破膜对产程进展及分娩结局的影响[J].现代中西医结合杂志,2014,23(2):162-164.
[15]谭光英,张宏玉,郑翠玲,等.低危初产妇足月分娩中人工破膜与自然破膜的临床研究[J].现代预防医学,2011,38(14):2734-2735.