Brugada phenocopy: emergence of a new clinical entity
, ,
Brugada phenocopy: emergence of a new clinical entity
ByronHGottschalk,DanielDAnselm,AdrianBaranchuk
[Abstract]Brugada phenocopies (BrP) are clinical entities that present with ECG patterns identical to true Brugada syndrome (BrS) but are induced by various clinical conditions. They are characterized by type 1 or type 2 Brugada ECG patterns in precordial leads (V1-V3) that present during an associated underlying condition. Upon resolution of the underlying condition, these ECG patterns normalize. In this study, we reviewed the classification of BrP, methods for differentiating BrP from BrS, and recently discussed etiologies of BrP. In addition, we provided an update on the international online registry for BrP and discussed future directions in BrP research.
[Key words]Brugada ECG pattern; Brugada phenocopy; Brugada syndrome
1Introduction
Brugada syndrome (BrS) is an inherited sudden cardiac death syndrome with autosomal dominant inheri-tance and variable penetrance. Over 70 mutations have been linked to the condition, most of which are found in cardiac sodium channels[1]. About 20-30 percent of patients affected by true BrS will have an identifiable SCN5A mutation[2].The condition is characterized on ECG by ST-segment changes in the right precordial leads (V1-V3) resulting in two defining patterns. The Type 1 (“coved”) Brugada ECG pattern is defined by a high take-off ST-segment elevation(≥2 mm), followed by a slow down-sloping concave or rectilinear ST-segment and a negative symmetric T wave (Fig.1)[1]. The Type 2 (“saddleback”) Brugada ECG pattern presents with a high take-off r′≥2 mm from the isoelectric baseline, followed by a convex ST-segment elevation of ≥0.05 mV with a variable T wave in lead V1and a positive or flat T-wave in lead V2(Fig.2)[1].While these patterns serve as the hallmark of BrS, it is important to note that the changes seen on ECG may be dynamic and are often concealed. In some patients, the typical ECG findings are “unmasked” by certain drugs or febrile states[3-4]. A personal or family history of syncope or aborted sudden cardiac death(SCD) provide additional clues to the BrS diagnosis. In cases where the diagnosis is not clear based on history and ECG changes alone, a positive provocative challenge with a potent sodium channel blocking agent such as ajmaline, procainamide, or flecainide suggests sodium channel dysfunction. BrS is important to identify as it is associated with a high risk for sudden cardiac death in young, otherwise healthy adults[5]. Upon diagnosis, patients should undergo risk stratification to determine their likelihood of malignant ventricular arrhythmias and high-risk patients are often referred for implantable cardiac defibrillator (ICD) therapy to reduce the morbidity and mortality associated with BrS.
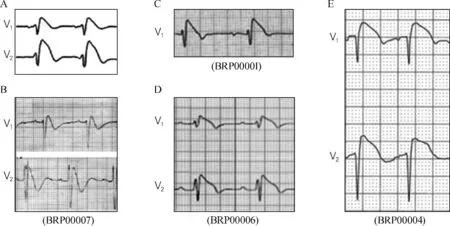
(A) True congenital type 1 Brugada syndrome electrocardiogram shown in comparison to (B) congenital hypokalemic periodic paralysis
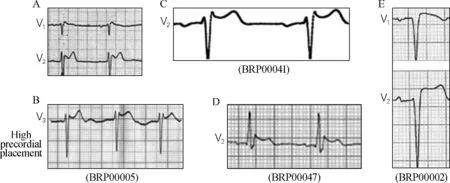
(A) True congenital type 2 Brugada syndrome shown in comparison to (B) congenital pectus excavatum causing mechanical mediastinal
Brugada phenocopies (BrP) are clinical entities with ECG findings identical to either the type 1 or type 2 Brugada ECG patterns yet differ etiologically from true congenital BrS[6-8]. These patient’s ECG findings are associated with an identifiable condition and upon resolution of that condition, the ECG pattern normalizes. Importantly, these patients have a negative sodium channel blocker provocative challenge suggesting a pathophysiological basis other than sodium channel dysfunction[7]. Alternatively, the sodium channel dysfunction may be transient occurring only during the inciting clinical event such as metabolic abnormality or ischemia, although this remains speculative. While the arrhythmogenic properties of BrS are well known along with the risk of sudden cardiac death, not much is known about the natural history of BrP. In an effort to facilitate research into the various etiologies, pathophysiology, and prognosis of the condition, we have developed an online educational portal and international registry for BrP (see www.brugadaphenocopy.com)[8]. This paper reviews previous cases of BrP, the various etiologies that have been identified in BrP, and future directions in research on this relatively new clinical entity.
2Classification of BrP
BrP may be induced under a multitude of clinical circumstances that have been characterized in six distinct etiological groups: (i) metabolic conditions, (ii) mechanical compression, (iii) ischemia, (iv) myocardial and pericardial disease, (v) ECG modulation, and (vi) miscellaneous(Tab.1)[7, 9]. In addition, they are further classified according to the presenting ECG morphology: type 1 BrP if the patient presents with a type 1 Brugada ECG pattern; or type 2 BrP if the patient presents with a type 2 Brugada ECG pattern. Cases of BrP are further sub-classified as A, B, and C(Tab.1). Class A includes true BrP in which all mandatory diagnostic criteria have been including negative provocative challenge with a sodium channel blocking agent. Class B includes cases highly suspected to be BrP; however, the mandatory diagnostic criteria are incomplete. These are cases where a provocative challenge is not possible due to factors such as the patient being deceased or lost to follow-up. Class C includes highly suspected cases of BrP; however, provocative testing was not justified such as in cases with recent surgical right ventricular outflow tract(RVOT) manipulation[10].
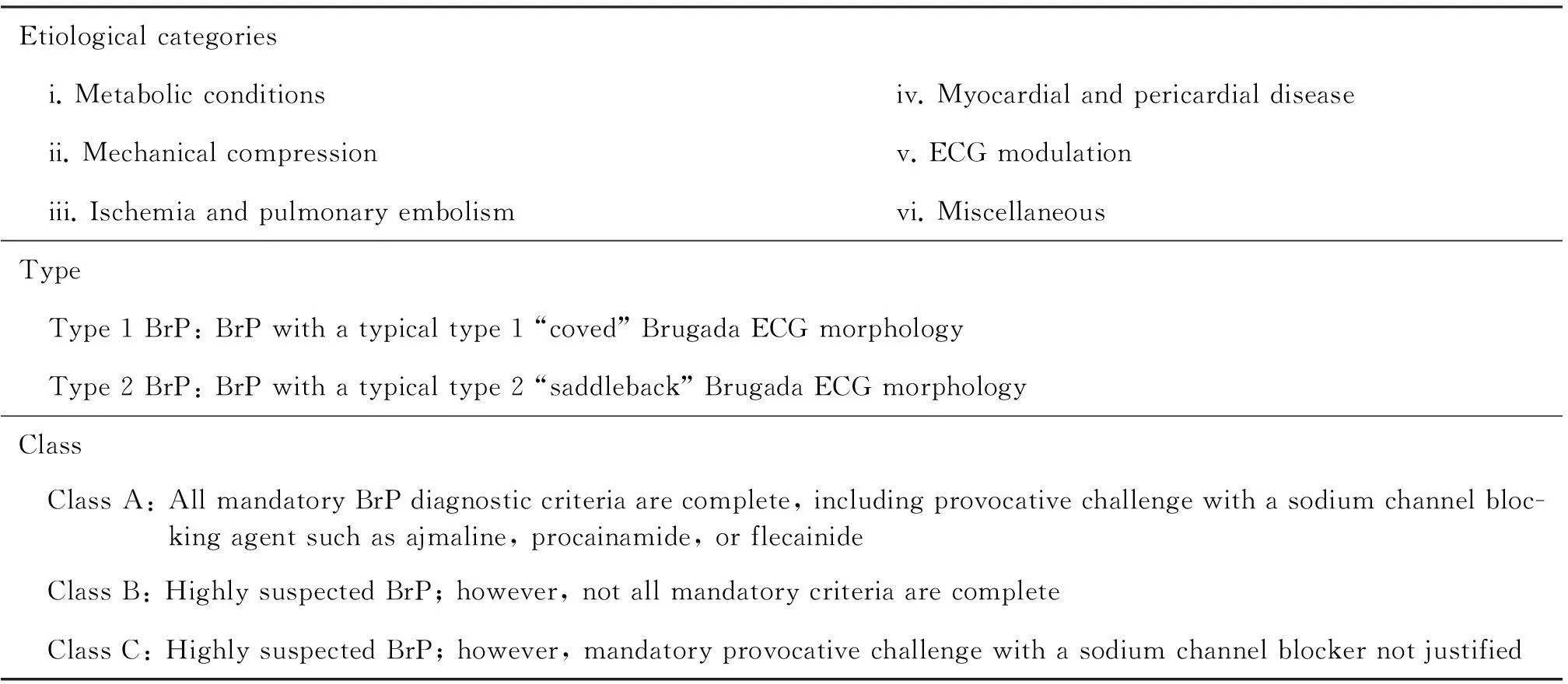
Tab.1 Brugada phenocopy etiological categories and morphological classification system
Adapted from Gottschalk et al[10]
3Differentiating BrP from BrS
Establishing a clear diagnostic distinction between BrP and BrS is of the utmost importance[11-12]. The fact that BrS may occur spontaneously, with no personal or family history of suggestive of the condition and in the absence of known genetic abnormalities makes differentiating between the two conditions challenging[1-2]. Current recommendations for diagnosis and risk stratification of BrS rely on a combination of clinical factors, presenting ECG morphologies, and positive provocative testing with a sodium channel blocking agent. It is this combination of factors that guides the clinical decision of whether to implant an ICD or not[1]. Similarly, the clinical diagnosis of BrP requires clinical factors(an identifiable underlying condition that triggers the ECG pattern in the absence of personal or family history suggestive of BrS), presenting ECG morphologies identical to BrS that normalizes upon resolution of the underlying condition, and a negative provocative test with sodium channel blocking agents[7]. Tab.2 depicts the current recommended systematic diagnostic criteria for BrP.
The importance of this distinction is highlighted by the natural history of the two conditions; while for patients with high risk of BrS who are candidates for treatment with an ICD, the clinical implications of BrP remain unknown. Therefore, current recommendations for treatment of BrP focus on resolving the underlying condition.
3.1Methods
Using Ovid MEDLINE(R) and Ovid OLDMEDLINE(R) from 1947 to May Week 1 2015, EMBASE from 1980 to May Week 1 2015, and PubMed we performed a search using “Brugada Syndrome”MeSH heading combined with keyword searches for “Brugada Phenocopy”“mimicking Brugada”“induced Brugada syndrome”“acquired Brugada”“Brugada-like”“Brugada type”, and “Brugada pattern”. The results were reviewed and case reports were selected according to the following inclusion criteria: (i) the case report was published; (ii) the case report includes a legible ECG showing a Brugada ECG pattern; (iii) the patient in the case does not have true BrS determined by a low clinical probability, absence of a positive provocative test, and/or absence of a positive genetic test for BrS. Case reports were excluded if they reported an example of confirmed (or suspected) underlying BrS being unmasked by drug, fever, or other clinical circumstances.
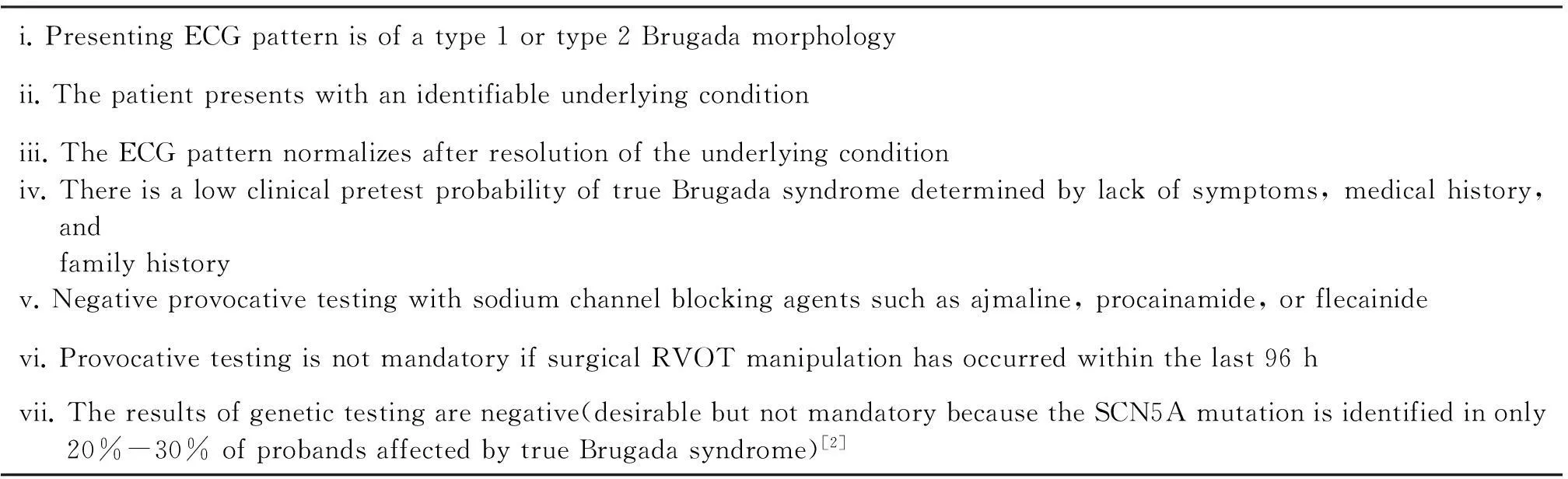
Tab.2 Brugada phenocopy diagnostic criteria
Adapted from Anselm et al[13]. Abbreviation: ECG, electrocardiogram; RVOT, right ventricular outflow tract; SCN5A, sodium channel voltage-gated type V alpha subunit
3.2Results
Fifty-eight case reports, reporting 71 individual cases of BrP met our inclusion criteria. These cases were classified according to the updated classification of BrP[9]. Tab.3 depicts an updated summary of BrP as of May, 2015. Since the first literature review on BrP published by our group in 2012, 37 cases have been added to the database[7]. These include BrP in the context of myocardial infarction, pulmonary embolism, and intracranial hemorrhage.

Tab.3 Summary of Brugada Phenocopy Registry

Continued
Quoted from Gottschalk et al[8]
3.2.1BrP:myocardial infarctionAt this time,there are 5 cases of BrP in the context of myocardial ische-mia[14-18]. Of the reports demonstrating BrP in the context of myocardial infarction, 3 were the result of a right coronary artery occlusion and 2 were the result of a left coronary artery occlusion. All 5 of the cases presented without a family history or personal history suggestive of BrS, thus making BrP very likely. Two of the 5 cases was a confirmed type 1A BrP in that all the diagnostic criteria were met[14, 18].
Is ischemia eliciting BrP or unmasking BrS?
Interestingly, ischemia may either induce BrP as previously discussed, or it may result in unmasking of true BrS through modulation of myocardial sodium channels[19-20]. Two interesting case reports demonstrate this phenomenon and illustrate the importance of proper diagnostic investigations in this patient population[18, 21]. Jiang et al[18]described a patient who presented with a type 1 Brugada ECG pattern and elevated troponin Ⅰ levels shortly after radiofrequency catheter ablation as treatment of atrial fibrillation. The patient underwent coronary angiography that revealed a sub-total occlusion in the first diagonal. In this case, we hypothesized that the ST-segment elevations produced after this procedure were likely the result of ischemia[20]. This patient underwent a diagnostic provocative test using a sodium channel blocker for BrS. The result was negative,which coupled with the patient’s lack of personal or family history suggestive of BrS, which was diagnostic for a type 1A BrP due to myocardial ischemia. This case is the second confirmed BrP reported in the context of myocardial ischemia in the international registry.
In contrast to the previously discussed case, Garg et al[21]discussed a particularly interesting case of a patient presenting with a Brugada ECG pattern during an acute coronary event. This patient subsequently underwent a provocative test with ajmaline, which proved to be positive, thereby diagnosing BrS in this patient that was unmasked by ischemia.
These cases highlight the need to investigate the cause of a Brugada ECG pattern. Indeed, the patient described by Garg et al would require risk stratification in order to determine his risk for SCD.
3.2.2BrP:pulmonary embolismTo date, there have been 4 reported cases of BrP in the context of acute pulmonary embolism[22-24]. Three of these cases presented with a type 1 Brugada ECG pattern while the final case presented with a type 2 Brugada ECG pattern. The phenomenon of right precordial ST-elevations caused by moderate to severe pulmonary emboli has been previously reported in the literature[25-28]. In all 4 reported cases of BrP in the context of acute pulmonary embolism, the responsible embolism was either large or massive. A speculated mechanism behind these ECG manifestations is the idea that large emboli results in significant right ventricular strain leading to transient sodium channel dysfunction[13].Zhan et al[24]further postulated that the right ventricular strain results in transmural ischemia of the right ventricle leading to the ST-elevations through a similar mechanism that is found during BrP in the context of right ventricular myocardial infarctions.
3.2.3BrP:neurological diseaseOur group published the first documented case of a confirmed BrP caused by a neurological condition in 2014[29].Briefly, an 85-year-old man was admitted to ICU after syncope complicated by traumatic head injury. A CT scan demonstrated temporo-parietal subarachnoid hemorrhage and 12 hours after the patient was admitted, he developed a type 2 Brugada ECG pattern that resolved within 9 hours. This patient underwent a subsequent CT scan demonstrating an insular hematoma with intraventricular hemorrhage.The patient underwent sodium channel provocation with flecainide that failed to induce a Brugada ECG pattern.He was therefore diagnosed with a type 2A BrP.There are various reports in the literature of cardiac manifestations of neurologic disease[30-32].These complications include ST-segment elevation on ECG in cases of subarachnoid hemorrhage. Indeed, there are multiple reports[30, 33-35]of the relationship between the insular region and ECG abnormalities(including ST-segment elevation).We postulated that our patient’s Brugada ECG manifestations were a result of neurological dysfunction caused by hematoma formation in the insular region of the brain[29].It is likely that resolution of the pressure effect of the hematoma resulted in normalization of the ECG pattern in this patient.To our knowledge,this is the only published case of BrP due to a neurologic disease to date and the only case of its kind registered in our international database.
3.3Future directions
Most reported cases of BrP discussed a single inciting event such as metabolic derangement or myocardial ischemia during which the Brugada ECG pattern was observed. Recently, we advanced the concept of clinical reproduction in BrP where resolution of an underlying condition resulted in normalization of the ECG[36]. The pattern subsequently reappeared when the same underlying condition reoccurred. In short, a young patient with diarrhea was admitted to the hospital following the development of severe hypokalemia(K+1.5 mEq/L). An ECG was performed and demonstrated a type 1 Brugada ECG pattern. After correction of the patient’s metabolic abnormalities, an ECG showed resolution of the Brugada ECG pattern. During the same admission, the patient again became hypokalemic(K+2.6 mEq/L) due to ongoing gastrointestinal losses. The corresponding ECG demonstrated recurrence of the type 1 Brugada ECG pattern that subsequently normalized after correction of the metabolic derangement. This patient had no personal or family history suggestive of BrS and underwent a negative provocative challenge. This is the first case that demonstrated clinical reproducibility of BrP.
Future investigations of BrP must focus on the development of experimental models designed to fully understand the mechanisms behind BrP. Through experimentation, we will begin to understand whether BrP are the result of transient sodium channel dysfunction that is not reproduced by sodium channel blocking agents, or whether the key to the ECG manifestations lies in malfunction of other ion channels. We may find that BrP and BrS are indeed entities along a continuous spectrum of ion channel dysfunction.
3.4Conclusions
The BrP international registry is aimed at furthering knowledge on the etiology, pathophysiology, and natural history of these phenomena. At this point, it is unknown whether BrP is a risk factor for malignant arrhythmias since there have been no studies examining the long-term prognosis of these patients. The question of clinical reproducibility of BrP has been demonstrated through one report thus far; however, we will be looking for more such examples in the future. Questions that remain unanswered include whether development of BrP predisposes patients to malignant arrhythmias under certain clinical conditions, or whether a patient that develops BrP in the context of one etiology is at risk of developing BrP in another etiology. The international database will aid in answering these questions through collating patients, identification of patterns, and assessing the long-term morbidity and mortality of these patients with longitudinal follow-up. Within the first year of the website being operational, it has generated over 2 000 unique visitors resulting in the submission of a number of potential BrP cases. With further awareness of the concept and more widespread use of the term “Brugada phenocopy” in the literature, we expect this number to grow more rapidly. In order to facilitate research on this phenomenon, we encourage other investigators to use the term “Brugada phenocopy” when reporting such cases. In addition, we invite the submission of cases to our online international registry at www.brugadaphenocopy.com.
References
[1] Bayés de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern:a consensus report[J]. J Electrocardiol, 2012, 45(4):433-442.
[2] Probst V, Wilde AA, Barc J, et al. SCN5A mutations and the role of genetic background in the pathophysiology of Brugada syndrome[J]. Circ Cardiovasc Genet, 2009, 2(6):552-557.
[3] Postema PG, Wolpert C, Amin AS, et al. Drugs and Brugada syndrome patients:review of the literature, recommendations, and an up-to-date website(www.brugadadrugs.org)[J]. Heart Rhythm, 2009, 6(9):1335-1341.
[4] Wilde AA, Antzelevitch C, Borggrefe M, et al. Proposed diagnostic criteria for the Brugada syndrome:consensus report[J]. Circulation, 2002, 106(19):2514-2519.
[5] Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome:report of the second consensus conference:endorsed by the Heart Rhythm Society and the European Heart Rhythm Association[J].Circulation. 2005, 111(5):659-670.
[6] Anselm DD, Gottschalk BH, Baranchuk A. Brugada phenocopies:consideration of morphologic criteria and early findings from an international registry[J]. Can J Cardiol, 2014, 30(12):1511-1515.
[7] Baranchuk A, Nguyen T, Ryu MH, et al. Brugada phenocopy:new terminology and proposed classification[J]. Ann Noninvasive Electrocardiol, 2012, 17(4):299-314.
[8] Gottschalk BH,Anselm DD,Baranchuk A.Brugada Phenocopy international registry and online educational portal[EB/OL].(2013-08-01)[2015-06-10].www.brugadaphenocopy.com.
[9] Anselm DD, Baranchuk A. Brugada phenocopy:redefinition and updated classification[J]. Am J Cardiol, 2013, 111(3):453.
[10] Gottschalk B, Anselm DD, Baranchuk A. Brugada phenocopy:morphological classification and importance of provocative testing[J]. Ann Noninvasive Electrocardiol, 2014, 19(6):604-605.
[11] Gottschalk BH, Anselm DD, Baranchuk A. Brugada phenocopies are the leading differential diagnosis of Brugada syndrome[J]. Clin Med, 2015, 15(3):308-309.
[12] Gottschalk BH, Anselm DD, Baranchuk A. Brugada syndrome unmasked by ischemia needs full risk evaluation[J]. Intern Emerg Med, 2015, 10(1):111-112.
[13] Anselm DD, Baranchuk A. Brugada Phenocopy in the context of pulmonary embolism[J]. Int J Cardiol, 2013, 168(1):560.
[14] Anselm D, Barbosa-Barros R, de Sousa Belém L, et al. Brugada Phenocopy induced by acute inferior ST-segment elevation myocardial infarction with right ventricular involvement[J].Inn Card Rhythm Manag,2013,4:1092-1094.
[15] Eggebrecht H, Wieneke H, Erbel R. Brugada-like ECG pattern in a patient with isolated right ventricular infarction[J]. Herz, 2009, 34:327.
[16] Nakazato Y,Kurata T,Yamaguchi H.ST segment elevation in the precordial leads mimicking Brugada syndrome[J].Heart,2000,83(2):216.
[18] Jiang C, Wang R, Lu W, et al. A Brugada-like electrocardiogram pattern induced after radiofrequency catheter ablation of atrial fibrillation[J]. Int J Cardiol, 2015, 178:e1-e4.
[19] Di Diego JM, Antzelevitch C. Acute myocardial ischemia:cellular mechanisms underlying ST segment elevation[J]. J Electrocardiol, 2014, 47(4):486-490.
[20] Gottschalk BH,Anselm DD,Baranchuk A.Brugada phenocopy induced by ischemia or Brugada syndrome unmasked by ischemia?[J].Int J Cardiol,2014,177(2):619-620.
[21] Garg P,Nelson T,Sahu J,Sheridan P.Is this ST-elevation because of myocardial ischemia or a Brugada pattern?An interesting case review[J].Intern Emerg Med,2015,10(2):249-250.
[22] Wynne J, Littmann L. Brugada electrocardiogram associated with pulmonary embolism[J]. Int J Cardiol, 2013, 162(2):e32-e33.
[23] Yetkin Ö, Turhan H. Massive pulmonary embolism simulating electrocardiographic pattern of Brugada syndrome[J]. TAPE, 2007, 5:260-264.
[24] Zhan ZQ, Wang CQ, Nikus KC, et al. Brugada phenocopy in acute pulmonary embolism[J]. Int J Cardiol, 2014, 177(3):e153-e155.
[25] Grand A, Taine B, Huret JF, et al. An overlooked electrocardiographic sign of acute embolic cor pulmonale:elevation of the ST segment in right precordial leads[J]. Ann Cardiol Angeiol(Paris), 1985, 34(5):361-362.
[26] Cassin M, Charmet P, Collazzo R, et al. Electrocardiographic aspects simulating acute myocardial infarct in massive pulmonary embolism. Description of 2 cases[J]. G Ital Cardiol, 1986, 16(10):882-885.
[27] Panneerselvam A, Dattatreya PV, Sridhar L, et al. ST-segment elevation in right precordial leads in acute pulmonary embolism[J]. JICC, 2011, 1:112-114.
[28] Zhan ZQ, Wang CQ, Wang ZX, et al. Significance of ST-segment deviation in patients with acute pulmonary embolism and negative T waves[J]. Cardiol J, 2015 May 25. doi:10.5603/CJ.a2015.0023. [Epub ahead of print]
[29] Labadet C, Gottschalk BH, Rivero M, et al. Brugada phenocopy in the context of intracranial hemorrhage[J]. Int J Cardiol, 2014, 177(3):e156-e157.
[30] Baranchuk A, Nault MA, Morillo CA. The central nervous system and sudden cardiac death:what should we know?[J]. Cardiol J, 2009, 16(2):105-112.
[31] Goldberger ZD, Creutzfeldt CJ, Goldberger AL. Catastrophic neurologic syndrome with dramatic ECG changes[J]. J Electrocardiol, 2014, 47(1):80-83.
[32] Saritemur M,Akoz A,Kalkan K,et al.Intracranial hemorrhage with electrocardiographic abnormalities and troponin elevation[J]. Am J Emerg Med, 2013, 31(1):271.e5-271.e7.
[33] Christensen H,Boysen G,Christensen AF,et al.Insular lesions,ECG abnormalities,and outcome in acute stroke[J].J Neurol Neurosurg Psychiatry, 2005, 76(2):269-271.
[34] Koppikar S, Baranchuk A, Guzmn JC, et al. Stroke and ventricular arrhythmias[J].Int J Cardiol,2013,168(2):653-659.
[35] Svigelj V, Grad A, Tekavcic I,et al. Cardiac arrhythmia associated with reversible damage to insula in a patient with subarachnoid hemorrhage[J].Stroke,1994,25(5):1053-1055.
[36] Genaro NR, Anselm DD, Cervino N, et al. Brugada phenocopy clinical reproducibility demonstrated by recurrent hypokalemia[J]. Ann Noninvasive Electrocardiol, 2014, 19(4):387-390.
Brugada拟表型:一个新的临床实体
ByronHGottschalk,DanielDAnselm,AdrianBaranchuk蒋祖勋 译并审校
[摘要]Brugada拟表型(Brugada phenocopy, BrP)是临床实体,它与真正的Brugada综合征(Brugada syndrome, BrS)具有相同的心电图波形,但前者是由各种临床状况诱发的。在某种相关的潜隐状况下,BrP的特征表现为心前区导联V1~V3呈1型或2型Brugada心电图波形。随着潜隐状况的纠正,这些心电图波形恢复正常。本研究中,我们回顾了BrP的分类、与BrS鉴别的方法及有关BrP病因的最新研究结果。此外,我们提供了BrP国际在线注册的更新数据,并讨论了BrP未来的研究方向。 表3Brugada拟表型注册的类别个体数量(病例报道的数量)平均年龄(范围)男性:女性BrP类型代谢状况33(26)49±16(19~89)23:82例未知Type1A:8Type2A:1Type1B:17Type2B:7Type1C:0Type2C:0机械压迫11(10)42±23(1~71)6:5Type1A:8Type2A:1Type1B:5Type2B:1Type1C:2Type2C:0缺血和肺动脉栓塞8(7)54±9(43~70)3:5Type1A:1Type2A:0Type1B:5Type2B:2Type1C:0Type2C:0心肌和心包疾病10(7)48±12(28~72)7:3Type1A:2Type2A:1Type1B:5Type2B:2Type1C:0Type2C:0心电图调制3(3)34±19(20~55)2:1Type1A:0Type2A:1Type1B:0Type2B:0Type1C:0Type2C:2其他6(5)33±30(7~85)3:3Type1A:0Type2A:2Type1B:1Type2B:1Type1C:2Type2C:0
[关键词]Brugada心电图波形; Brugada拟表型; Brugada综合征
1引言
Brugada综合征(Brugada syndrome, BrS)是一种遗传心源性猝死综合征,具有常染色体显性遗传和可变的外显率。超过70种基因突变与这种状况有关,大多数突变发现在心脏钠通道中[1]。在真正的BrS患者中,约20%~30%可检测出SCN5A基因突变[2]。这种状况的特征性心电图表现为在右心前区导联V1~V3上出现ST段改变,产生两个典型的波形。1型(穹窿型)Brugada心电图波形定义为迅速上升的ST段抬高(≥2 mm),紧接着一个较慢的下斜凹面或直线ST段,以及负性对称T波[图1:各种1型Brugada拟表型(Brugada phenocopy, BrP)的比较;(A) 真正的先天性1型BrS心电图;(B) 先天性低钾周期性瘫痪(1B型BrP);(C) 急性下壁ST段抬高型心肌梗死伴右室受累(1A型BrP);(D) 并行高钾、低钠及酸中毒(1A型BrP);(E) 急性肺动脉栓塞(1B型BrP)。图下数字是BrP国际注册的身份编号。][1]。2型(马鞍型)Brugada心电图波形表现为从等电位基线出现一个迅速上升的r′≥2 mm,紧接着一个凸面ST抬高(≥0.05 mV),伴V1导联变化的T波和V2导联正向或扁平的T波[图2:各种2型BrP的比较;(A) 真正的先天性2型BrS;(B) 先天性漏斗胸引起机械纵隔压迫(2A型BrP);(C) 急性心包炎(2A型BrP);(D) 意外触电损害后(2A型BrP);(E) 采用不恰当的高通心电图滤波的结果(2C型BrP)。图下数字是BrP国际注册的身份编号。][1]。当把这些波形作为BrS的标志时,需要特别注意的是,心电图上看到的改变可以是动态的并且常常是不易被发现的。对一些患者而言,某种药物或发热状态可使典型的心电图表现暴露出来[3-4]。晕厥或心源性猝死(SCD)中止的个人或家族病史提供了BrS诊断的另一线索。对于单纯基于病史和心电图改变难以确诊的患者,采用强力钠通道阻滞剂(如阿马林、普鲁卡因胺或氟卡尼)进行的阳性激发试验可提示钠通道功能失常。由于与年轻人及健康成人的心源性猝死高危分层相关,因此BrS的识别是很重要的[5]。依据诊断,应对患者进行危险分层以决定其发生恶性心律失常的可能性,并且高危患者常被要求考虑植入心脏除颤器(ICD),以降低BrS相关的发病率和死亡率。
BrP是临床实体,其心电图表现与1型或2型BrS心电图波形相同,然而在病因学上又不同于真正的先天性BrS[6-8]。这些患者的心电图表现与某种可辨识的状况相关联,且随着这种状况的纠正,心电图波形恢复正常。重要的是,这些患者的钠通道阻滞剂激发试验结果呈阴性,提示除钠通道功能失常以外还存在病理生理基础[7]。或者,钠通道功能失常可能仅仅一过性地出现在刺激性临床事件中,如代谢异常或缺血,尽管这仍然是推测性的。人们能够清楚地认识BrS的致心律失常特性与心源性猝死风险,然而关于BrP的自然病史却所知不多。为了推进病因学、病理生理学和疾病预后等各层面的研究,我们开发了一个在线教育入口和BrP国际注册系统(见www.brugadaphenocopy.com)[8]。本文回顾了之前的BrP病例、已识别的BrP病因以及这种相对较新的临床实体的未来研究方向。
2BrP的分类
BrP可在许多临床环境下被诱发,依特征分为6个病因组:① 代谢状况;② 机械压迫;③ 缺血;④ 心肌和心包疾病;⑤ 心电图调制;⑥ 其他(表1)[7, 9]。此外,依据表现出来的心电图形态,BrP可被进一步分类:1型BrP,如果患者表现为1型Brugada心电图波形;或2型BrP,如果患者表现为2型Brugada心电图波形。BrP的病例还能进一步亚分为A、B和C类(表1)。A类包括真正的BrP,所有的强制诊断标准是完整的,包括钠通道阻滞剂的激发试验结果呈阴性。B类包括高度怀疑BrP的病例,然而强制诊断标准是不完备的。由于患者死亡或无法进行随访等因素,对上述病例不可能进行激发试验。C类包括高度怀疑BrP的病例,然而激发试验不适用,例如近期行右心室流出道外科手术的病例[10]。

表1 Brugada拟表型病因类别和形态分类系统病因类别
改编自Gottschalk等[10]
3BrP与BrS的鉴别
建立BrS和BrP之间清晰的鉴别诊断标准至关重要[11-12]。BrS可在无相关个人或家族病史,且缺乏已知的基因异常的情形下自发出现,这就使二者的鉴别具有挑战性[1-2]。对于BrS的诊断和危险分层,目前推荐综合临床因素、表现出的ECG形态和钠通道阻滞剂的阳性激发试验加以考量。正是这些因素的结合指导临床决定是否植入ICD[1]。类似地,BrP的诊断要求临床因素(即某种可识别的潜隐状况,在无BrS相关个人或家族病史的情况下引发相应的ECG波形),表现出与BrS相同的、随潜隐状况纠正而正常化的ECG形态,以及钠通道阻滞剂激发试验阴性[7]。表2为目前推荐的BrP的诊断标准。
这两种状况的自然病史使BrP与BrS鉴别的重要性更为突出;而对BrS高危且预备进行ICD治疗的患者而言,临床上是否预示着发生BrP尚不明确。因此目前对BrP的治疗,我们推荐先集中精力改善潜隐状况。

表2 Brugada拟表型诊断标准
改编自Anselm等[13]。缩写:RVOT,右心室流出道;SCN5A,钠通道电压门控V型a亚单位
3.1方法
我们以“Brugada综合征”为MeSH主题词,以“Brugada拟表型”“拟Brugada”“诱发的Brugada综合征”“获得性Brugada”“Brugada样”“Brugada型”和“Brugada波形”为关键词,应用Ovid MEDLINE(R)和Ovid OLDMEDLINE(R)搜索从1947年至2015年5月第一周、EMBASE搜索从1980年至2015年5月第一周及PubMed搜索相关文献。我们对结果进行了回顾分析,且依据下列纳入标准选取病例报告:① 该病例报告已发表;② 该病例报告中至少有一张显示Brugada心电图波形的清晰的心电图;③ 由于较低的临床可能性、未做阳性激发试验和/或未做BrS的阳性基因测试,判断病例中的患者未患有真正的BrS。排除标准:由于药物、发热或其他临床环境,而被揭示出来的确认(或疑似)的潜在BrS。
3.2结果
我们共选出58份病例报告,报道了71例BrP个案病例,其均满足事先设定的纳入标准。依据更新的BrP分类标准[10]对这些病例进行分类。表3为2015年5月更新的BrP国际注册的统计数据。自从2012年我们团队发表了第一篇关于BrP的文献综述,已有37个病例加入到了这一数据库中[7]。这些病例包括心肌梗死、肺动脉栓塞和颅内出血合并的BrP。

续表
引自Gottschalk等[8]
3.2.1BrP: 心肌梗死此时,在心肌梗死的情况下有5例BrP[14-18]。在心肌梗死背景下显示BrP的报道中,3例是由右冠状动脉阻塞导致的,2例是由左冠状动脉阻塞导致的。上述所有5例患者并没有BrS相关的个人或家族病史,由此患有BrP的可能性很大。5例中的2例被确认为1A型BrP,满足所有的诊断标准[14, 18]。
缺血将会激发BrP,还是会暴露BrS?
有趣的是, 缺血既可以诱发BrP(正如先前讨论的),也可以通过心肌钠通道的调制使真正的BrS暴露出来[19-20]。两例有趣的病例报道证实了这一现象并且阐明了对该类患者群进行适当的诊断性调查的重要性[18, 21]。Jiang等[18]报道了一例患者,行心房颤动射频消融术后短时间内表现为1型Brugada心电图和肌钙蛋白Ⅰ水平升高。冠脉造影显示该患者第一对角支几乎完全阻塞。在这一病例中,我们假定消融术后产生的ST段抬高可能是缺血造成的[20]。该患者因BrS接受了钠通道阻滞剂的诊断性激发试验。激发试验呈阴性,加之缺乏BrS相关的个人或家族病史,患者诊断为心肌缺血引起的1A型BrP。在BrP国际注册中,上述病例是心肌缺血背景下第二例确诊的BrP。
对比先前讨论过的病例,Garg等[21]讨论了一例在急性冠脉事件中表现出Brugada心电图波形的特别有趣的病例。该患者随后做了一次阿马林激发试验,结果呈阳性,由此诊断为缺血所暴露的BrS。
这些病例说明探讨Brugada心电图波形的成因很有必要。实际上,应对Garg描述的这些患者进行危险分层,以判断其心源性猝死的风险。
3.2.2BrP: 肺动脉栓塞迄今为止,在急性肺动脉栓塞的背景下,我们已有4例BrP的报道[22-24],其中3例表现为1型Brugada心电图波形,1例表现为2型Brugada心电图波形。由中度至严重肺动脉栓塞引起的右心前区导联ST段抬高的现象,之前已经相关文献[25-28]报道。在所有报道的4例急性肺动脉栓塞背景下的BrP病例中,起重要影响的栓塞要么是大块,要么是巨大块。据猜测,出现这些心电图表现的机制是大栓塞产生明显的右室牵张,从而导致一过性钠通道功能失常[13]。Zhan等[24]进一步推测:右室牵张产生右室透壁性缺血,继而导致ST段抬高,其发生机制就类似于右室心肌梗死背景下发生BrP的机制。
3.2.3BrP:神经系统疾病我们研究团队在2014年公开发表了第一例确诊的BrP病例[29],其是由神经系统状况引起的。简述如下:患者男,85岁,因晕厥合并头部外伤收入ICU。CT扫描示颅顶部蛛网膜下腔出血;入院12 h后,该患者出现2型Brugada心电图波形,9 h内消失。随后再行CT扫描,显示存在一个孤立的血肿伴脑室内出血。对该患者用氟卡尼进行钠通道激发试验,未能诱发Brugada心电图波形。由此该患者被诊断为2A型BrP。在反映神经系统疾病心脏表现的相关文献中,已有多篇报道[30-32]。在蛛网膜下腔出血的病例中,这些并发症包括心电图ST段抬高。实际上,已有多篇报道[30, 33-35]涉及孤立区域和心电图异常(包括ST段抬高)之间的关系。 现在我们假定患者的Brugada心电图表现是脑部孤立区域血肿形成、引起神经功能失常所致[29]。血肿压力效应的消退有可能使该患者的心电图波形恢复正常。据我们所知,这是迄今为止报道的唯一一例神经系统疾病所致的BrP病例,并且这类病例在我们的BrP国际数据库中也仅注册了一例。
3.3未来研究方向
大多数BrP病例报道讨论的是在一个单独的激发事件(如代谢失常或心肌缺血)过程中所观察到Brugada心电图波形。近年来,我们发展了BrP临床再现的概念,某种潜隐状况的纠正将导致心电图正常化[36]。当同样的潜隐状况再次发生时,这种心电图波形随后再次出现。下面简要介绍一例。一位年轻患者因腹泻入院,继而发展为严重的低钾(K+1.5 mEq/L)。心电图显示为1型Brugada波形。患者的代谢异常纠正后,心电图示Brugada波形消失。住院期间,患者因持续的胃肠道损失而再次出现低钾状况(K+2.6 mEq/L)。相应的心电图显示再次出现1型Brugada心电图波形,代谢失常纠正后波形恢复正常。该患者无BrS相关的个人或
家族病史,且激发试验呈阴性。这是证实BrP临床再现性的第一例。
未来的BrP研究应当聚焦于设计和发展实验模型,以便完全理解BrP的发生机制。借助实验,我们将逐步了解BrP是否是一过性的钠通道功能失常(利用钠通道阻滞剂无法重现)造成的,或者心电图表现的发生机制是否在于其他离子通道功能失常。我们可能发现:BrP和BrS实际上是沿着离子通道功能失常连续谱系存在着的临床实体。
3.4结论
BrP国际注册旨在增进人们对上述现象在病因学、病理生理学及自然病史方面的了解。就这一点而言,BrP是否是恶性心律失常的危险因素尚不明确,原因是目前还没有关于这些患者长期预后的研究。迄今为止,BrP临床再现性的问题已被一份病例报告所证实,然而将来我们会寻找更多这样的例子。仍有待回答的问题包括:BrP的进展是否易使患者在某种临床状况下发生恶性心律失常;或由于某一病因发生BrP的患者在另一病因下是否有发生BrP的风险。通过整理患者资料、鉴别心电图波形,以及在纵向随访中评价这些患者的长期发病率和死亡率,我们所开发的国际数据库将有助于回答上述问题。在网站开放的第一年内,它吸引了超过2 000位独立访问者,并提交了大量潜在的BrP病例。随着对这一概念认识的加深以及在文献中越来越普遍地使用“Brugada拟表型”这一术语,我们期待着它的使用频次增长得更为迅速。为了方便对该现象的研究,我们鼓励其他研究者在报道这样的病例时运用术语“Brugada拟表型”。此外,我们诚邀研究者们将相关病例提交到我们的BrP在线国际注册系统,见www.brugadaphenocopy.com。
参考文献(图和请查阅前面的英文原文)
【致谢】衷心感谢广东省人民医院心功能科的蒋祖勋主任在百忙中承担了本文的翻译和审校工作。
(本文编辑:顾艳)

作者单位: 050031 河北 石家庄,河北医科大学第一医院急诊科(苏冠丽,李斌),心血管内科(刘刚,郑明奇)

作者单位: 050051 河北 石家庄,河北医科大学附属石家庄市第三医院心血管内科(刘红彬,张晓华,刘志红);050041 河北 石家庄,石家庄市建北社区卫生服务中心心血管内科(张志刚)
专题主持/刘刚
Author Unit: K7L 2V7 Kingston, Ontario, Canada, Department of Cardiology, Kingston General Hospital, Queen’s University(Byron H Gottschalk, Adrian Baranchuk); T2N 2T9 Calgary, Alberta, Canada, Libin Cardiovascular Institute of Alberta, Foothills Medical Centre, University of Calgary(Daniel D Anselm
Author Brief Introduction:Byron H Gottschalk,BMSc,medical student at Queen’s University;research interests:Brugada phenocopy,Brugada ECG pattern.
Correspondence Author:Adrian Baranchuk, E-mail: barancha@kgh.kari.net
通信作者:刘刚,E-mail:cardio2004@163.com
作者简介:苏冠丽,主治医师,主要从事心血管内科研究。 刘红彬,主任医师、教授,主要从事冠心病及其介入治疗研究,E-mail:lhbyxr@126.com
基金项目:河北省科技计划项目(13277720D);河北省重大医学科研课题资助项目(zd2013081,ZL201320,ZL20140141) 河北省科技计划项目(13277720D)
收稿日期:(2015-06-19)
[中图分类号]R541; R540.4
[文献标志码]A
[文章编号]2095-9354(2015)04-0245-11
DOI:10.13308/j.issn.2095-9354.2015.04.002 10.13308/j.issn.2095-9354.2015.04.002