Comparisons of family environment between homeless and non-homeless individuals with schizophrenia in Xiangtan, Hunan
Jinliang CHEN*, Jindong CHEN, Shuchun LI Jun LIU Guohua OUYANG Wenxuan LUOXiaofeng GUO, Ting LI Kaijie LI Zhenkuo LI Gan WANG
Comparisons of family environment between homeless and non-homeless individuals with schizophrenia in Xiangtan, Hunan
Jinliang CHEN1,*, Jindong CHEN2, Shuchun LI1, Jun LIU1, Guohua OUYANG1, Wenxuan LUO1,Xiaofeng GUO2, Ting LI1, Kaijie LI1, Zhenkuo LI1, Gan WANG1
homelessness; schizophrenia; family environment; China
1. Introduction
Homelessness among individuals with schizophrenia in China is much less common than in high-income countries but it is, nevertheless, is an increasingly important problem in the country, partly due to increased mobility of the population (so family members are dispersed) and partly due to the one-child per family policy (so there are fewer relatives available to care for a mentally ill family member). The limited number of studies about this issue in mainland China focus on the socio-demographic characteristics and physical health of the homeless mentally ill and on their difficulties in obtaining necessary psychiatric treatment.[1]To the best of our knowledge, there has been no research about the original family environment of homeless individuals with schizophrenia in China, a factor that potentially contributes to their homelessness. Noxious family environments and schizophrenic symptoms can exacerbate each other leading to the ejection or departure of the ill individual; in the absence of otherfamily members who can care for the individual or government-supported half-way houses, the ill individual then becomes homeless and, thus, is less likely to receive appropriate treatment.[2]Research about the characteristics of the original families of individuals with mental disorders who become homeless is needed to help characterize high-risk families who should become the focus of preventive interventions aimed at reducing homelessness among patients with serious mental illnesses.
In this study we define homelessness as a period of 7 days or greater in which a person with a confirmed diagnosis of schizophrenia has no place to stay, no source of income, and no social or family support.The study compares the sociodemographic and family characteristics of individuals with schizophrenia who did and did not meet this definition of homelessness.
2. Methods
2.1 Subjects
The recruitment of participants for this study is shown in the flowchart in Figure 1. All participants were from the Fifth Ren Min Hospital of Xiangtan, the hospital that is the designated center for the treatment of homeless mentally ill in Xiangtan City, a municipality in Hunan Province with a population of 2.8 million, 72% of whom are rural residents. Between April 2011 and April 2014,a sample of 2439 consecutively admitted homeless inpatients and a convenience sample of 2033 nonhomeless inpatients with a diagnosis of schizophrenia were screened for enrollment in the study. Among the homeless individuals, 212 (8.7%) refused to participate,182 (7.5%) were excluded, and 189 (7.7%) had incomplete data, leaving 1856 (76.1%) who completed the study questionnaire. In the non-homeless group,198 (9.7%) refused, 84 (4.1%) were excluded, and 23(1.1%) had incomplete data, leaving 1728 (85.0%) who completed the study questionnaire.
All participants met the following inclusion criteria: a) met the diagnostic criteria for schizophrenia according to the Chinese Classification of Mental Disorders (CCMD-3);[3]b) 18 to 60 years of age; c) had a score of 35 or lower on the Brief Psychiatric Rating Scale(BPRS)[4](indicating that they were clinically remitted)at the time of the assessment; d) were able to take care of themselves at the time of assessment; e) could comprehend and complete the study questionnaire; and f) signed the informed consent form for the study. Based on their medical records, participants who had organic brain disease, severe physical illness, psychoactive substance dependence, mental retardation, mood disorders, or personality disorders were excluded.‘Homeless’ was defined as living on the streets, public places, cars, deserted buildings, and so forth, for at least 7 days prior to the index admission.[4]All homeless participants were brought to the hospital by the police;the police were usually notified about the individualsby local community members and unable to rapidly locate the individual’s family, so they transported them to the hospital. The non-homeless group consisted of inpatients with schizophrenia who were not homeless at the time of admission.

Figure 1. Flowchart of the study
2.2 Assessment instrument
The Family Environment Scale (FES) was developed by Moss and colleagues in 1981. FES has been used widely in Western countries to assess the change in family environment before and after family interventions. This study used the third version of the Chinese version of the scale (FES-CV)[5]which had good reliability across patient ratings and family-member ratings when assessing family environment, and had good internal consistency and validity. There are 90 true or false questions in FES-CV, divided into ten 9-item subscales that assess different aspects of the family environment.
The internal consistency (Cronbach’s α) of the ten FES-CV subscales was as follows: cohesion 0.75,expressiveness 0.42, conflict 0.67, independence 0.24,achievement orientation 0.55, intellectual-cultural orientation 0.64, active-recreational orientation 0.57,moral-religious emphasis 0.33, organization 0.63,and control 0.53. The definition of each subscale is as follows. Cohesion: the degree of commitment, help and support the family members provide for each other. Expressiveness: how much family members are encouraged to openly express their emotions.Conflict: the extent to which family members openly express anger and disagreements. Independence: the amount of self-esteem, confidence, and autonomy that family members have. Achievement orientation:the degree to which common activities (for example,going to school or working) are considered measures of achievement and the degree of focus on competition-oriented activities. Intellectual-cultural orientation: the level of interest of family members in political, societal,intellectual, and cultural activities. Active-recreational orientation: the degree of family members’ participation in social and recreational activities. Moral-religious emphasis: the emphasis on ethics, religion, and value.Organization: the extent to which family activities and responsibilities are organized and structured. Control:the importance of following family rules and procedures to arrange family life.
The items all have dichotomous responses so the range in subscale scores is 0 to 9, with higher scores indicating a greater tendency to have the trait considered by the subscale.[6]
2.3 Assessment procedure
The FES-CV is a self-report scale that takes less than 30 minutes to complete. This was administered an average of 50 days after the index admission (while the patients were still inpatients). Before the administration of the instrument, trained psychiatrists provided participants with standardized instructions about how to complete the scale. For about 100 illiterate participants in each group, trained psychiatrists read the FES-CV and completed the scale based on respondents’ answers.On the same day that the patient completed the FESCV, a trained clinician administered the Brief Psychiatric Rating Scale (BPRS).
2.4 Statistical analysis
All data analyses were conducted using SPSS 17.0. FESCV subscale scores were continuous measures that approximated normal distributions, so the mean scores of the two groups (i.e., homeless and non-homeless patients) were compared using t-tests. Categorical variables were compared using chi-squared tests.
In order to explore variables that were independently associated with homelessness, two unconditional multivariate logistic regression models were performed. The first model used a backward stepwise procedure to identify socio-demographic variables independently associated with homelessness.The nine socio-demographic variables considered included age, gender (male v. female), occupation(stable job, temporary job, and unemployed), residence(urban vs. rural residence), place of origin (Xiangtan vs. other), marital status (unmarried, married, and divorced or widowed), level of educational (high school or above, middle school, and primary school or below),ethnicity (Han versus other), and severity of psychotic symptoms at the time of the assessment of family functioning (as assessed by the total BPRS score). The second logistic regression entered all 10 subscale scores of the FES-CV after forcing all significant variables from the first model into the expanded model; the goal was to determine which family environment variables were associated with homelessness after adjusting for socio-demographic variables. In the second analysis two variables (residence and place of origin) had to be dropped from the model due to collinearity. The statistical significance level was set atp<0.05 (twosided).
3. Results
3.1 Comparison of demographic variables and FES-CV subscale scores
The basic characteristics of participants are shown in Table 1. The gender distribution was similar in both groups and the severity of psychiatric symptoms at the time of the FES-CV evaluation was similar between the two groups, but all the other characteristics were significantly different between the groups. Compared to the non-homeless group, those in the homeless group were older and they were more likely to be rural residents, from outside of Xiangtan, to have a lower level of education, and to be married. The proportion of individuals who had temporary jobs was higher in the homeless group, but the proportion of unemployed individuals was higher in the non-homeless group.
As shown in Table 2, with the exception of the expressiveness subscale, all of the FES-CV subscale scores differed significantly between the two groups.
Compared to respondents in the non-homeless group,those in the homeless group reported that their original families had greater achievement orientation,intellectual-cultural orientation, organization, and control; they also reported that their original families had lower levels of cohesion, conflict, independence,active-recreational orientation, and moral-religious emphasis.

Table 1. Comparison of basic characteristics of two groups

Table 2. Comparison of subscale scores of the Chinese version of the Family Environment Scale (FES-CV)between homeless and non-homeless inpatients with schizophrenia
3.2 Logistic regression of demographic and family environment risk factors for homelessness in patients with schizophrenia
To identify variables independently associated with homelessness, the aforementioned demographic variables were entered into a logistic regression model,the results of which are shown in Table 3. Eight of the nine variables considered (in Table 1) were significant in the multivariate model. Among this sample of 3574 inpatients with schizophrenia, being homeless at the time of admission was associated with older age, female gender, more severe psychiatric symptoms (at the time of assessing family functioning), rural residence,low educational achievement, residence outside of Xiangtan, being marriage or divorced, and working on a temporary job. There were three differences between the univariate and multivariate results: gender (being female) and severity of psychiatric symptoms became significantly related to homelessness after adjustment for other demographic variables while ethnicity was no longer associated with homelessness after adjustment for the other variables.
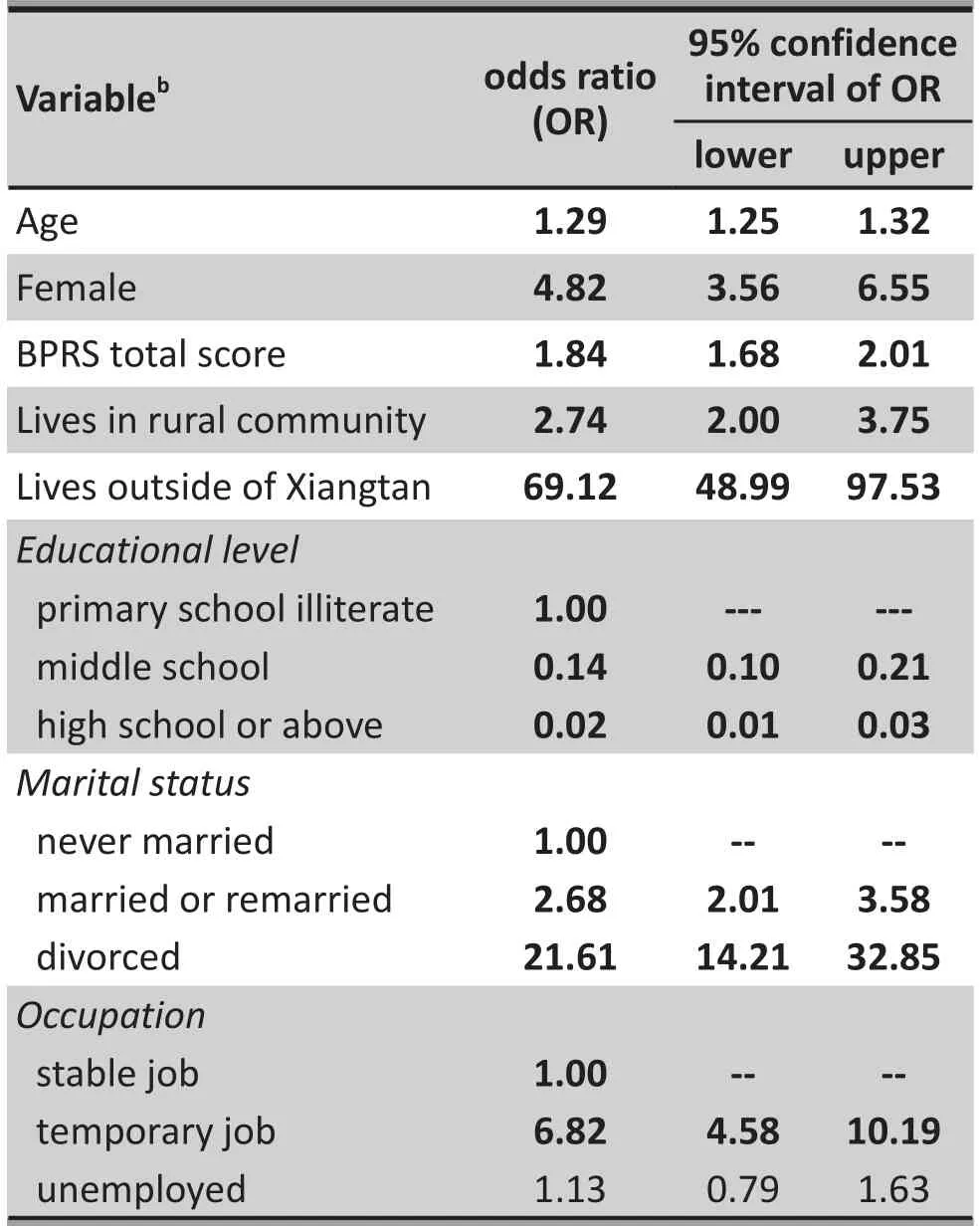
Table 3. Multivariate logistic regression of socio-demographic factors related to homelessness in 3574 patients with schizophreniaa
The key question for this paper is the extent to which prior family environmental factors are associated with homelessness after controlling for the demographic differences between homeless and nonhomeless individuals with schizophrenia. To assess this,the results of all ten FES-CV subscale were entered into a logistic regression model after adjusting for six of the eight socio-demographic variables that were significantly associated with homelessness (shown above). Two variables, urban versus rural residence and living outside of Xiangtan, could not be entered as covariates in the model because of collinearity. As shown in Table 4, with the exception of the conflict and expressiveness subscales, after adjustment of socio-demographic factors all of the other 8 subscale scores were significantly associated with homelessness.Specifically, homelessness was associated with greater organization, intellectual-cultural orientation,achievement orientation, and control; homelessness was also associated with lower levels of independence,cohesion, active-recreational orientation, and moralreligious emphasis. After adjustment the conflict subscale score was no longer significantly associated with homelessness, but the results for all the other subscales were similar to those seen in the univariate analysis (Table 2).
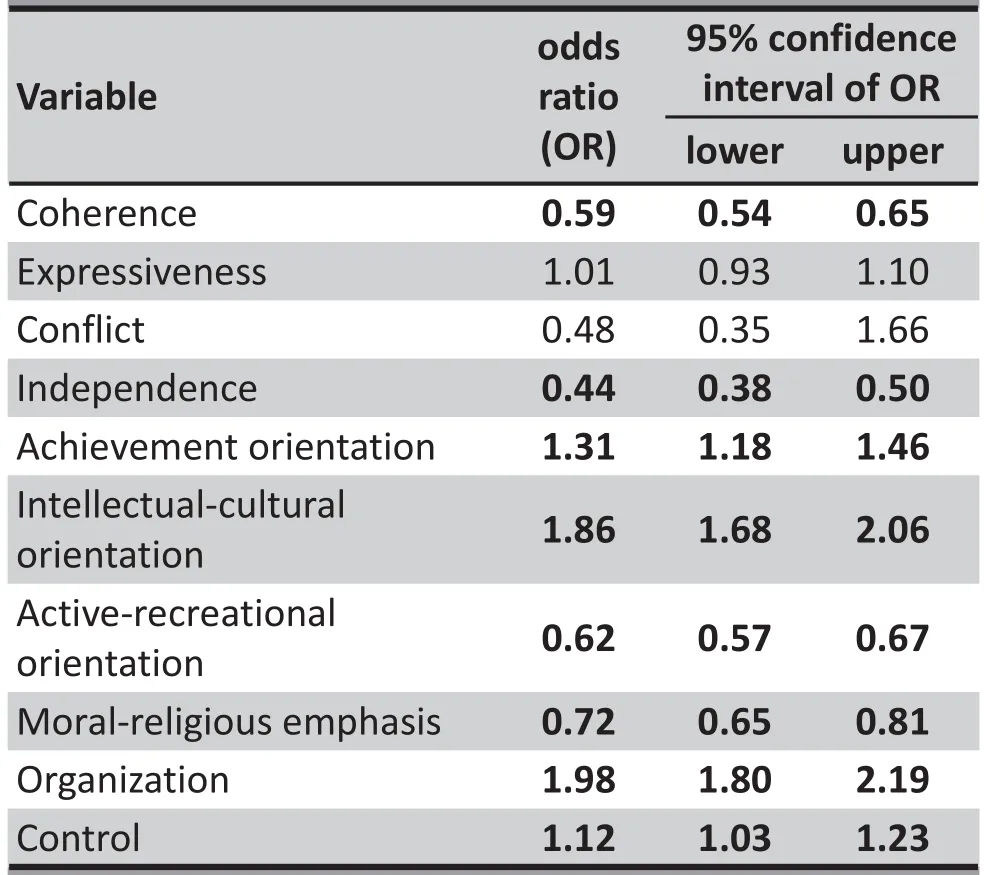
Table 4. Multivariate logistic regression of the relationship of family environment factors assessed by the subscales of the Chinese version of the Family Environment Scale(FES-CV) to homelessness in 3584 patients with schizophrenia after controlling for socio-demographic variablesa
4. Discussion
4.1 Main findings
This study identified a large sample of homeless individuals with schizophrenia and compared them to a sample of individuals with schizophrenia who were not homeless. There were substantial differences in the socio-economic characteristics of homeless and non-homeless patients and in the functioning of their original families – as reported by the patients after their acute psychotic symptoms had resolved.
Homelessness was equally common in men and women but after adjusting for other demographic variables women with schizophrenia were at greater risk of homelessness than men. As expected, homelessness was more common in individuals from rural communities (where social support services are limited),among those who wander away from their communities(i.e., those not from Xiangtan municipality), and among those with limited education (who are less able to mobilize social supports). Homelessness was also associated with greater age; its unclear why this is the case, but it may be that older patients have ‘burned their bridges’ with relatives and, thus, end up on the streets. Those who had never married (and, thus, were probably still living with parents) were less likely to be homeless while those who were currently married were more likely to be homeless. Finally, patients who reported having temporary employment (i.e., those with no stable income) were more likely to be homeless,while those who reported being unemployed were less likely to be homeless; this may be because formally unemployed individuals (typically only urban residents)may have access to social welfare benefits not available to those in temporary jobs.
Our study found that even after controlling for these socio-demographic variables, family environment– as assessed by the patients themselves using the FES-CV after their acute symptoms resolved – is significantly associated with homelessness among patients with schizophrenia. This finding is consistent with a substantial body of research which has found that family environment, particularly the cohesion and organization of the family,[7]is associated with the onset and course of serious mental illness. Some patients with schizophrenia grow up in noxious family environments which contribute to the emergence and development of their illness.[8,9]Harsh physical and verbal punishment from family members have been associated with the severity of symptoms in individuals with schizophrenia.[10]Addressing these family problems using comprehensive bio-psycho-social interventions can reduce the severity of patients’ symptoms, help the patient maintain a stable mood, and prevent relapse.[11,12]
One of the 10 subscales assessed by the FES-CV,the conflict subscale, generated different results in the univariate and multivariate analysis – family conflict was less important in the self-reports of homeless patients than in the self-reports of non-homeless patients, but this difference disappeared after adjustment for the sociodemographic factors. The remaining 9 subscales were consistent in the univariate and multivariate analyses, indicating that demographic factors did not strongly influence the results. As reported by the patients themselves, families in which patients with schizophrenia become homeless have a stronger a) intellectual-cultural orientation, b) achievement orientation, c) organization, and d) control; one possible interpretation for this is that patients with serious mental illnesses are less able to meet the high expectations of such families and, thus, are more likely to be extruded from the families or to leave on their own. Patients with schizophrenia who become homeless also report that their families have weaker a)cohesion, b) moral-religious emphasis, c) independence,and d) active-recreational orientation; one possible interpretation for this is that such families are generally less supportive of individual family members with problems. However, some of the constructs considered by the FES-CV subscales are not fully consistent with Chinese cultural norms (e.g., the importance of‘independence’ and a ‘moral-religious emphasis’) so one must be cautious in interpreting these subscale results.Efforts are needed to identify more culture-sensitive measures of family functioning in China.
4.2 Limitations
There are several limitations that need to be considered when interpreting these results. This was a large inpatient sample from one location in China; we are unable to determine how representative this sample is of all homeless individuals with schizophrenia in China. The 7-day duration of homelessness used as the operational definition of homelessness in this study was chosen arbitrarily; it may be too short to identify the chronically homeless subgroup of patients who are most in need of social services. The assessment of family function was based on a self-completion instrument completed by individuals who had been hospitalized for two to three months at the time they completed the instrument and, in the case of the homeless group, may have been separated from their family for some time prior to hospitalization; this could introduce substantial recall bias. Moreover, all respondents had schizophrenia so their interpretation of family functioning may have been affected by their illness. Other factors that may affect homelessness among mentally ill individuals such as the personality and coping skills of the patients, and the number, age, and socio-economic status of the patients’ close relatives were not considered. The very large sample resulted in many small but statistically significant differences between the groups; one needs to be cautious to avoid over-interpreting these small differences. Finally, the evaluation of family functioning was based on a scale for which some of the subscales have weak internal consistency: previous studies with the FES-CV[6]have shown that the Cronbach alpha values for the expressiveness, independence, achievement orientation, active-recreational orientation, moralreligious emphasis, and control subscales are all below 0.60, indicating that the items in these subscales are not assessing a distinct construct. Future research about this important topic will need to address these complex issues.
4.3 Implications
This study identifies both demographic characteristics of patients and characteristics of patients’ families that are independently associated with homelessness among individuals with schizophrenia. These results need to be confirmed by simultaneously obtaining information on family function from patients’ family members and by using other measures of family functioning. The next step will be to see if these retrospectively identified risk factors for homelessness can prospectively predict which patients will become homeless. If they can, then clinicians must develop and test interventions aimed at reducing this very negative outcome (i.e., homelessness)for persons with serious mental disorders.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The Fifth Ren Min Hospital of Xiangtan provided 50,000 Chinese Yuan to support this study.
Ethics review
The study was approved by the Ethics Committee of The Fifth Ren Min Hospital of Xiangtan.
Informed consent
All participants provided written informed consent for participation in this study.
Acknowledgement
The Xiangtan Medical Association provided policy support and human resources for this project.
1. Chen JL, Guo XF, Chen JD. [Introduction to research about homeless patients with schizophrenia].Guo Ji Jing Shen Bing Xue Za Zhi. 2014; 41(1): 56-58. Chinese
2. Schlosser DA, Pearson R, Perez VB, Loewy RL. Environmental risk and protective factors and their influence on the emergence of psychosis.Adolesc Psychiatry (Hilversum).2012; 2(2): 163-171
3. Psychiatry Branch of the Chinese Medical Association. [China Classification and Diagnostic Criteria for Mental Disorders,3rd Edition]. Shandong: Shandong Science and Technology Press; 2001. Chinese
4. Wang XD, Wang XL, Ma H. [Updated Version of Mental Health Rating Scale Manual ]. Beijing:Chinese Mental Health Magzine (suppl); 1999. pp: 263-267. Chinese
5. Hwang SW, Kirst MJ, Chiu S, Tolomiczenko G, Kiss A, Cowan L.Multidimensional social support and the health of homeless individuals.J Urban Health. 2009; 86(5): 791-803. Epub 2009 Jul 23. doi: http://dx.doi.org/10.1007/s11524-009-9388-x
6. Phillips MR. [Family Environment Scale – Chinese Version(FES-CV)]. In: Wang XD, Wang XL, Ma H, editors. [Handbook of Mental Health Rating Scales (updated version)]. Beijing:Chinese Mental Health magazine; 1999. p. 134-142. Chinese
7. Xu P, Yang JH. [Correlation between family environment and psychological health of teenager with schizophrenia disease].Zhongguo Jian Kang Xin Li Xue Za Zhi.2007;15(2): 157-159. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1005-1252.2007.02.025
8. Lv F, Gao H, Liang JG, Li P, Liu JT, Yu XJ. [A controlled study of family relations and parental rearing styles of patients with schizophrenia].Zhong Hua Jing Shen Ke Za Zhi.2001; 4: 42-44. Chinese. doi: http://dx.doi.org/10.3760/j:issn:1006-7884.2001.04.011
9. Amaresha AC, Venkatasubramanian G. Expressed emotion in schizophrenia: an overview.Indian J Psychol Med.2012; 34:12-20. doi: http://dx.doi.org/10.4103/0253-7176.96149
10. Masanet MJ, Lacruz M, Asencio A, Bellver F, Montero I. [Emotional family environment and clinical profile in schizophrenia].Actas Luso Esp Neurol Psiquiatr Cienc Afines.1997; 25(3): 159-66. Spanish
11. Jiang YH, He JY, Liang CS, Li RJ, Hou ZY, Zhang JX. [Effects of synthetical intervention on family environment in rural schizophrenia].Zhong Hua Jing Shen Ke Za Zhi. 2004;37(2): 99-102. Chinese. doi: http://dx.doi.org/10.3760/j:issn:1006-7884.2004.02.011
12. Zhou GZ, Sun ZM. [Relationship between family environment and relapse schizophrenia patients].Zhongguo Jian Kang Xin Li Xue Za Zhi.2005; 13(4): 256-258. Chinese. doi: http://dx.doi.org/10.3969/j.issn.1005-1252.2005.04.006
, 2014-10-27; accepted, 2015-06-20)

Jinliang Chen obtained a Bachelor’s degree in psychiatry from the Qiqiha’er Medical School in 2006. In 2013, he graduated from Zhong Nan University with a Master’s degree in psychiatry and mental health.Since 2007, he has been working as an attending physician and deputy director of the Second Psychiatric Ward at the Fifth Ren Min Hospital of Xiangtan. His research interests are psychopharmacology and the psychiatric epidemiology of homelessness among persons with serious mental disorders.
There are two errors in the print version of the article:
Xie MM, Jiang WH, Yang HB. Efficacy and safety of the Chinese herbal medicine shuganjieyu with and without adjunctive repetitive transcranial magnetic stimulation (rTMS) for geriatric depression: a randomized controlled trial.
Shanghai Archives of Psychiatry.2015; 27(2): 103-110. doi: http://dx.doi.org/10.11919/j/issn.1002-0829.214151
In the second sentence of the first paragraph of section ‘2.1 Sample’ (last line of left column on page 104), the listed sample size was incorrect: ’Study participants were 79 patients with geriatric depression…’ should read‘Study participants were 65 patients with geriatric depression…’.
In the second sentence of the first paragraph of section ‘4.1 Main findings’ (third line of the left column on page 108), the numbers in parentheses representing subjects who completed the trial were incorrect:‘Ninety-four percent (65/69) of the enrolled subjects completed the 6-week trial.’ Should read ‘Ninety-four percent (61/65) of the enrolled subjects completed the 6-week trial.’
The online version of the article is correct.
流浪与非流浪精神分裂症患者的家庭环境比较
陈进良,陈晋东,李淑春,刘军,欧阳国华,罗文轩,国效峰,李婷,李凯杰,李震阔, 王甘
流浪行为;精神分裂症;家庭环境;中国
Background: Homelessness is an increasingly important problem for individuals with serious mental illness in China.Aims: Identify the characteristics of families that are associated with homelessness among individuals with schizophrenia.Methods: Participants were 1856 homeless individuals with schizophrenia (defined as those who had no place of residence or involved caregivers for 7 consecutive days) and 1728 non-homeless individuals with schizophrenia from Xiangtan, Hunan. The self-completion Family Environment Scale-Chinese Version (FES-CV)was administered to these participants after their acute psychotic symptoms resolved.Results: Compared to individuals in the non-homeless group, those in the homeless group were older and more likely to be non-locals (i.e., from outside of Xiangtan), be residents of rural (versus urban)communities, have temporary (versus permanent) jobs, be married, and have a low level of education.After controlling for demographic differences using multivariate logistic regression models, homelessness was independently associated higher scores in the FES-CV intellectual-cultural orientation, organization,achievement orientation, and control subscales and with lower scores in the FES-CV cohesion, moralreligious emphasis, independence, and active-recreational orientation subscales.Conclusions:After controlling for sociodemographic factors, certain aspects of the family environment are associated with being homeless among patients with schizophrenia in China. Further work is needed to identify interventions that can reduce the risk of homelessness in high-risk individuals.
[Shanghai Arch Psychiatry. 2015; 27(3): 175-182.
http://dx.doi.org/10.11919/j.issn.1002-0829.214162]
1Fifth Ren Min Hospital of Xiangtan, Hunan, Xiangtan, Hunan Province, China
2Mental Health Research Center, Xiang Ya Second Hospital of Zhong Nan University, Changsha, Hunan Province, China
*correspondence: 125592215@qq.com
背景:流浪行为逐渐成为中国严重精神疾病患者的一个重要问题。目的:发现在精神分裂症患者中与流浪行为相关的家庭特征因素。方法:本研究被试人员都来自湖南省湘潭市,包括1856例具有流浪行为的精神分裂症患者(其定义为连续7天没有地方居住或无照顾者)和1728例无流浪行为的精神分裂症患者。所有被试人员在急性精神病性症状得到缓解后,自行填写中文版家庭环境量表(Family Environment Scale-Chinese Version ,FES-CV)。结果:与无流浪行为的患者相比,有流浪行为的患者更为年长,并且更可能不是本地人(即从湘潭以外的地方来的),更可能是农村居民(相对于城市),更可能是临时工(相对于固定职业),多为已婚,以及教育程度偏低。本研究采用逻辑回归模型并控制人口学差异,发现流浪行为分别与FES-CV知识性、组织性、成功性和控制性分量表的较高评分独立相关,并分别与FES-CV凝聚力、道德宗教观、独立性、和娱乐性分量表的较低评分独立相关。结论:即使控制了社会人口学因素后,家庭环境的某些方面还是与中国精神分裂症患者的流浪行为相关,并需要进一步研究以确定可以减少高风险人群的流浪行为风险的干预措施。
本文全文中文版从2015年08月06日起在http://dx.doi.org/10.11919/j.issn.1002-0829.214162可供免费阅览下载
- 上海精神医学的其它文章
- Meta-analysis for psychiatric research using free soft ware R
- Development of a checklist of short-term and long-term psychological symptoms associated with ketamine use
- Oligodendroglioma presenti ng as chronic mania
- Abnormal inter- and intra-hemispheric integrati on in male paranoid schizophrenia: a graph-theoreti cal analysis
- Metacognitive training for schizophrenia: a systematic review
- Addressing risk of bias in trials of cognitive behavioral therapy

