Metacognitive training for schizophrenia: a systematic review
Jiangling JIANG, Li ZHANG, Zhipei ZHU, Wei LI, Chunbo LI*
•Systematic review and meta-analysis•
Metacognitive training for schizophrenia: a systematic review
Jiangling JIANG, Li ZHANG, Zhipei ZHU, Wei LI, Chunbo LI*
metacognitive training; schizophrenia; randomized controlled trials; meta-analysis
1. Introducti on
Schizophrenia is a disorder characterized by distinctive distortions of thinking and perception and inappropriate or blunted affect; cognitive deficits also occur but intelligence and consciousness are usually maintained.[1]The lifetime prevalence of schizophrenia is estimated to be 0.3 to 0.7%, though there are reported differences in the prevalence by race, nationality, and geographic origin.[2]The course of schizophrenia is quite variable,but the first episode of schizophrenia usually occurs in the early twenti es.[3]This disorder is oft en accompanied by marked occupational or social dysfunction,[4]that results in serious disability and premature mortality.[5]The human and financial cost of the illness are substantial,[6]but differences in data collection methods across studies makes it difficult to precisely estimate the overall social burden attributable to schizophrenia.
Currently, medication remains the mainstay treatment for schizophrenia. A small proporti on of patients recover,[7]most patients respond to treatment but have ongoing chronic disability, and about 30 to 40%of patients only respond partially to antipsychoticmedication.[8]More recently, several studies have shown that adjunctive treatment using cognitive behavioral therapy for psychosis (CBTp) can improve the effectiveness of pharmacotherapy.[9]These studies have identified specific cognitive processes and biases among persons with schizophrenia,[10,11]some of which are associated with the formation and maintenance of delusional symptoms.[10,12]Individuals with schizophrenia a) jump to strong conclusions based on a small quantity of information;[13]b) lack insight about their rashness and, thus, consider themselves indecisive;[14]c) are unsure about their correct interpretations of information but over-confident about their incorrect interpretations of information;[15]d) frequently have attributional biases;[16]and e) are oft en convinced of the accuracy of false recollecti ons.[17]
Based on research about the cognitive processes and biases reported in persons with schizophrenia,Moritz and Woodward[18]developed a novel psychotherapeutic approach called ‘metacognitive training’ (MCT) that involves eight group sessions with 4 to 10 patients based on three fundamental components. The aim of MCT is to make patients aware of delusion-relevant cognitive biases and then to amend these biases. The first component is knowledge translation, which means describing cognitive biases in a way that explains how they contribute to the formation of delusions. The second component uses specific exercises to raise awareness about the negative consequences of cognitive biases. In the third component, participants are taught alternative thinking strategies to help them avoid the cognitive biases that can lead to delusional beliefs.[19]The modules for this treatment are freely available in over 30 languages(http://clinical-neuropsychology.de/metacognitive_training-psychosis.html).
Moritz has conducted several pilot studies on the feasibility, safety, and efficacy of MCT,[18,20-22]but given the relatively small sample sizes and short follow-up periods of these studies, the effectiveness of this new treatment modality remains in doubt. The primary objective of this review is to use meta-analytic methods to combine the results of available studies to help decide whether or not MCT for schizophrenia is effective.
2. Methods
2.1 Search methods
The article selection process is shown in Figure 1.Electronic searches up to January 2015 were conductedin Embase, MEDLINE, Web of Science, Current Contents,PsycINFO, and the Cochrane Collaboration Controlled Trials Register. (We also considered Chinese-language databases [CNKI, CQVIP, Wanfang] but no relevant articles were identified.) The following search strategy was used in Embase: [‘randomized controlled trial’/exp OR ‘randomized controlled trial’ AND (metacogniti *:ab,tiOR (‘meta’ NEAR/2 (‘cognitive’ OR ‘cognition’)):ab,ti)AND schizophreni*:ab,ti]. Similarly structured search strategies were used for the other databases. The references lists of articles identified in the electronic search were hand-searched for other relevant articles.
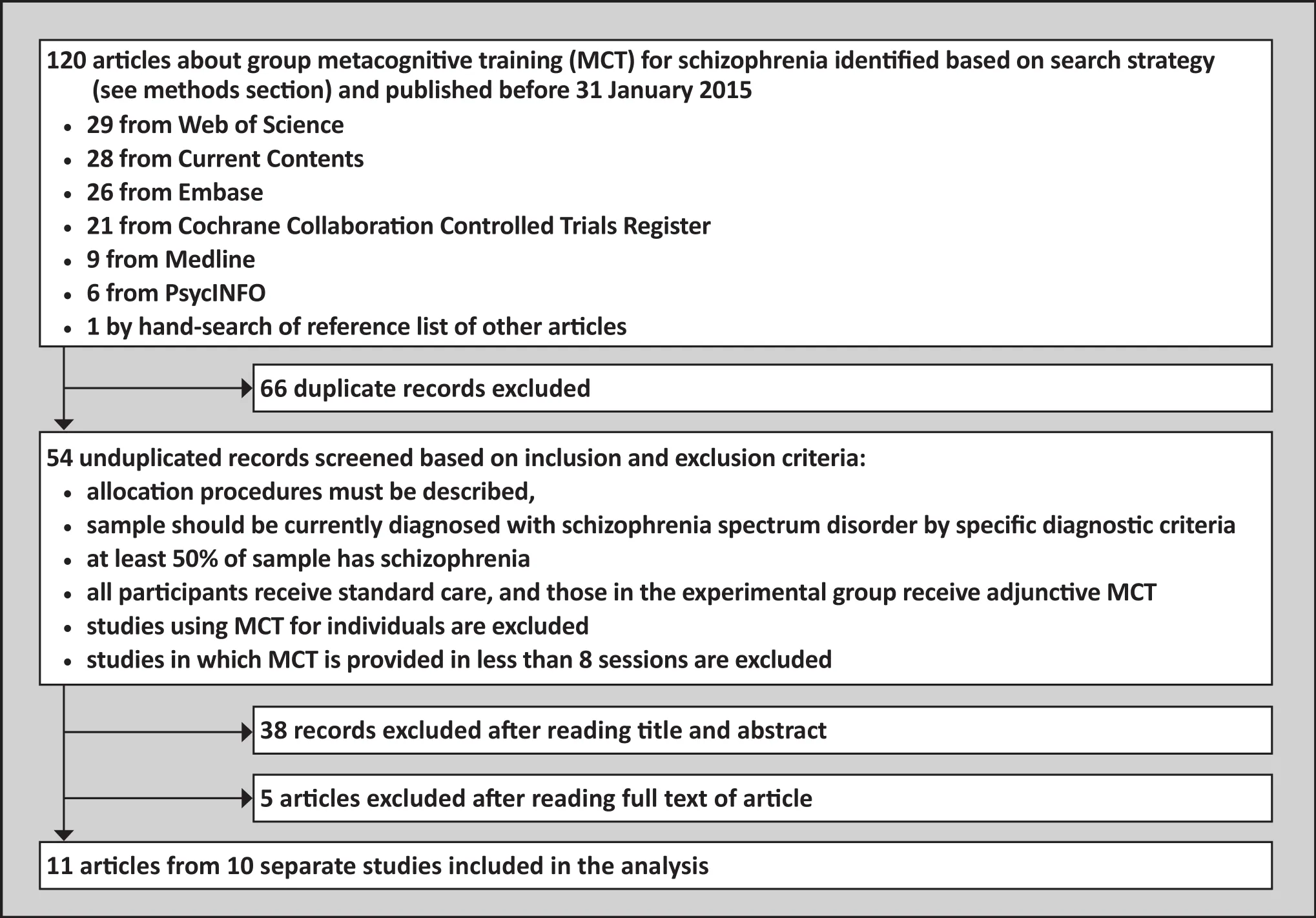
Figure 1. Identification of included studies
2.2 Studies selection procedure and inclusion criteria
Two authors (JLJ, ZPZ) first independently screened titles and abstracts of all articles identified by the electronic database searches for relevance; the full text of articles not excluded in the first step were then independently assessed against the screening criteria (below) by the two coders. In the first stage of screening they disagreed about two articles and in the second stage they disagreed about one article; they were able to resolve these differences between themselves without referring to the assigned arbitrator (WL). If two or more papers were published on a study, the primary paper, the paper with the largest number of patients, or the paper with the most informative data, was selected for inclusion in the analysis.
We considered all relevant randomized controlled trials (RCTs) as potentially eligible. Included studies had to a) describe the allocation procedure, b) include subjects with a current diagnosis of a schizophrenia spectrum disorder based on standardized criteria (e.g.,all conditions listed in the ‘Schizophrenia Spectrum and Other psychotic Disorders’ section of the Diagnostic and Statistical Manual of Mental Disorders,[23]or all disorders coded F20-F29 in the International Classification of Diseases[24]), c) have a sample in which at least 50% of the participants had a diagnosis of schizophrenia, d) all participants should receive standard pharmacological treatment, and e) participants in the experimental group receive adjunctive group MCT psychotherapy which met the description of MCT provided at http://clinicalneuropsychology.de/metacognitive_training-psychosis.html.Studies in which MCT was provided to individuals or that did not include a minimum of 8 standardized MTC sessions were excluded.
2.3 Outcome measures
The primary outcome was the severity of psychotic symptoms as assessed by the Positive and Negative Syndrome Scale (PANSS).[25]Secondary outcomes considered including ‘global state’ (i.e., meaningful changes in symptomatology and general clinical condition, recovery, and well-being), ‘mental state’ (i.e.,presence or absence of symptoms other than psychosis plus characteristics or behaviors of such symptoms),‘engagement with service’ (i.e., number of inpatient days, number of hospital admissions, changes in level of care), ‘quality of life’, ‘ general functioning’ (i.e.,changes in employment, occupational and educational status, level of received benefits or social welfare),‘adverse effects’, ‘dropout rate’, ‘satisfaction with treatment’ (i.e., satisfaction questionnaires devised by each study), and ‘economic costs’ (i.e., direct and indirect costs).
2.4 Data extraction, management, and analysis
Two authors independently extracted data from all included articles. Any disagreement was discussed and documented. Again, a third author settled disagreements that could not be solved by discussion.Authors of studies were contacted for clarification where necessary.
We originally planned to exclude any non-normal data from the meta-analysis, but we found that all but one of our intended outcome variables did not meet a simple criteria for use in a parametric analysis (that is, if minimum=0, mean>2*sd; if minimum >0, [meanminimum]>2*sd),[26]so we decided to pool the results regardless of their normality and interpret the outcome with cauti on. We synthesized data across studies using the Cochrane Collaboration Review Manager version 5.3 and R version 3.1.1 with random-effect models.Statistical significance was set atp<0.05.
2.5 Assessment of quality and heterogeneity of the included studies
Two author independently assessed risk of bias utilizing criteria described in theCochrane Handbook for Systematic Reviews of Interventions.[27]Disputes were resolved through discussion and, if necessary,involvement of a third author.
We planned to assess reporting bias by drawing funnel plots of the key outcomes, but ten studies with data on any specific outcome variable are needed to draw funnel plots and most outcomes only had 2 to 4 studies eligible for inclusion in a meta-analysis. An alternative strategy was to compare the outcomes specified in the original protocol of the included studies (provided on the study registry systems) with the outcomes actually employed in the fi nal published report, but the original protocol was only available for 4 of the 10 included studies.
Heterogeneity of results across the included studies was assessed using theI2statistic (ifI2>50% the results are considered heterogeneous) and the Chi-square statistic (if the p-value of Chi-square is <0.05, the results are considered heterogeneous).[27]If heterogeneity was present, subgroup analyses were conducted to identify the causes of the heterogeneity.
3. Results
3.1 Eligible studies
Eleven of the 54 unduplicated reports identified in the search were included in the qualitative analysis.[18,21,22,28-35]Two papers by Moritz and colleagues[21,22]reported the 6-month follow-up and 3-year follow-up data for the same study, respectively, so both papers were included.Thus data from a total of ten studies were used in the analysis.
The characteristics of the included studies are shown in Table 1. Most of the trials provided 8 MCT sessions over 4 weeks, but a few provided 8 sessions over 8 weeks and one provided 16 sessions over 8 weeks. Eight of the studies enrolled participants with schizophrenia spectrum disorders, seven had blinded assessment of the outcome, six employed treatment as usual (TAU) as the control condition, and four involved follow-up after completion of the MCT intervention.All trials enrolled more men than women, the sample size varied from 16 to 154 participants (mean of 65 participants), and the mean age of participants in the ten studies varied from 28.9 to 45.1 years.
3.2 Study quality
The results of the quality assessment are shown in Table 2. Only four of the eleven reports provided information about how the random sequences for group assignment were generated and only one study provided information about how group assignment was concealed from the individuals who assessed the outcome. None of the studies were double-blind (which is extremely difficult to do in psychotherapy trials), but most of the studies reported blinded outcome assessment. Three of the studies were rated as ‘high risk’ of attribution bias because they had greater than 20% attrition and did not compensate for this by using an intenti on-to-treat (ITT)analysis. All trials were labelled as ‘high risk’ of other biases because they all used parametric tests to assess non-parametric data.
3.3 Primary outcome
Seven of the ten studies used PANSS to assess outcomes[21,22,29,30,32,33,34,35]but the method of using PANSS varied so it was only possible to pool results in a meta-analysis for four studies that assessed thepositive symptom subscale of PANSS at the end of the treatment (shown in Figure 2). These studies had a pooled sample of 129 individuals in the intervention group and 120 in the control group. There was no significant heterogeneity in the results between the four studies. The results of the pooled analysis show a small but statistically significant advantage of adjunctive MCT treatment in reducing the severity of the positive symptoms of schizophrenia.

Table 1. Characteristics of randomized controlled trials comparing metacognitive training (MCT) with analternative treatment for patients with schizophrenia (SZ) or schizophrenia spectrum disorders (SSDs)

Table 2. Risk of bias assessment
Other PANSS results could not be combined across studies because the timing of the assessment or the component of PANSS reported varied. Moritz and colleagues’ 2011 trial with treatment as usual (TAU) as the control condition[34]reported no differences in the pre-post change scores of the PANSS subscale scores between the two groups. Three trials considered PANSS total scores at the end of treatment,[21,30,33]but none of them reported statistically significant differences. Two studies assessed PANSS positive symptom subscale scores after completion of MCT: the 2014 study by Favrod and colleagues[29]reported a statistically significant greater improvement at the six-month followup in the MCT group, and the 2013 and 2014 reports by Moritz and colleagues reported a non-significant advantage in the MCT group at both the 6-month and 3-year follow-up. The 2014 study by Kuokkanen and colleagues[33]reported significantly lower PANSS total scores in the MCT group 3 months after the end of the intervention and significantlyhigherPANSS total scores in the MCT group 6 months aft er the end of the interventi on. Overall, these results are inconclusive.
3.4 Secondary outcomes
Six of the studies[21,22,28,29,32,33,34]employed the 17-item psychotic Symptom Rating Scales (PSYRATS)[36]to assess outcomes. Four of these studies with pooled samples of 196 in the MCT group and 191 in the control group reported post-treatment scores of the 6-item delusion subscale of PSYRATS; a meta-analysis of these four studies (shown in Figure 3) found that the results were heterogeneous (I2=60%) and that the pooled result did not show a significant difference between the two groups. One study that reported the PSYRATS total score at the end of treatment[33]found a non-significant difference in favor of MCT. Another study that compared results for each of the 17 items on the PSYRATS[34]found significantly less self-reported distress due to delusions in the MCT group.
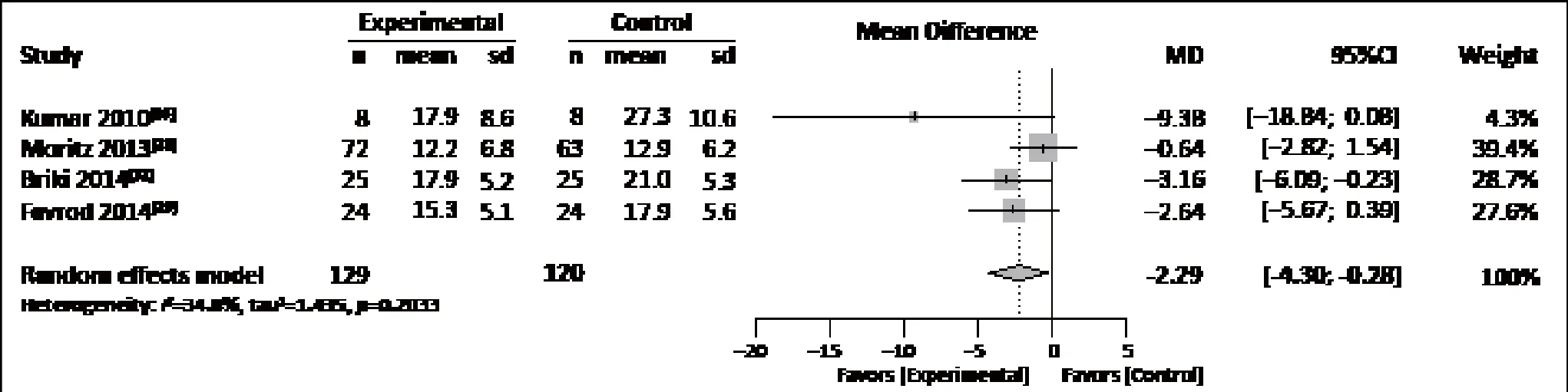
Figure 2. Forest plot of positive symptom subscale score of the positive and Negative Syndrome Scale (PANSS)assessed at the end of the intervention

Figure 3. Forest plot of delusion subscale score of the psychotic Symptoms Rating Scales (PSYRATS) assessed at the end of the interventi on
All ten studies reported dropout rates from the trial.As shown in Figure 4, four of the studies reported no dropouts so it was only possible to compute risk rati os for the six remaining studies. The pooled result across all studies showed no significant difference in dropout rates between the two groups.
None of the three trials that considered medication dosage as an outcome measure[28,29,32]found significant differences in the mean chlorpromazine-equivalent dosage employed by the two groups after the intervention. Three other studies assessed adverse effects[18,28,30]and found no significant differences between the groups. The 2014 study by van Oosterhout and colleagues[28]was the only study to consider treatment costs and societal economic burden of schizophrenia; they found no significant differences between the groups.
A wide range of other psychometric measures of delusions, cognitive biases, insight, depression, selfesteem, and so forth were employed in the ten included studies, but none of these measures were used in more than two of the studies so we did not attempt to synthesize the results.
3.5 Heterogeneity
Subgroup analysis was performed to investigate the reason for substantial heterogeneity in the results for the four studies that reported results for the delusion subscale of PSYRATS (Figure 3). When subdividing the studies by the type of control condition, we found that the two studies that employed TAU as the control condition[28,29]remained heterogeneous (I2=84% and p-value for Chi-square=0.01), while the two studies that used an alternative psychotherapy as the control condition[21,32]were homogeneous (I2=0% and p-value for Chi-square=0.90) – but the MCT results were not significantly better than results for the control group when pooling these two homogeneous studies. When subdividing the high-quality studies (i.e., those in which all types of biases other than ‘other bias’ are rated as low-risk) from other studies, there was only one study rated as high-quality[28]; the results of the other three studies[21,29,32]were homogeneous (I2=0% and p-value for Chi-square=0.83), and the pooled results for these three studies showed a signi fi cantly greater drop in the delusion subscale score in the MCT group compared to the control group (-1.80 [-3.34, -0.26], p=0.02).
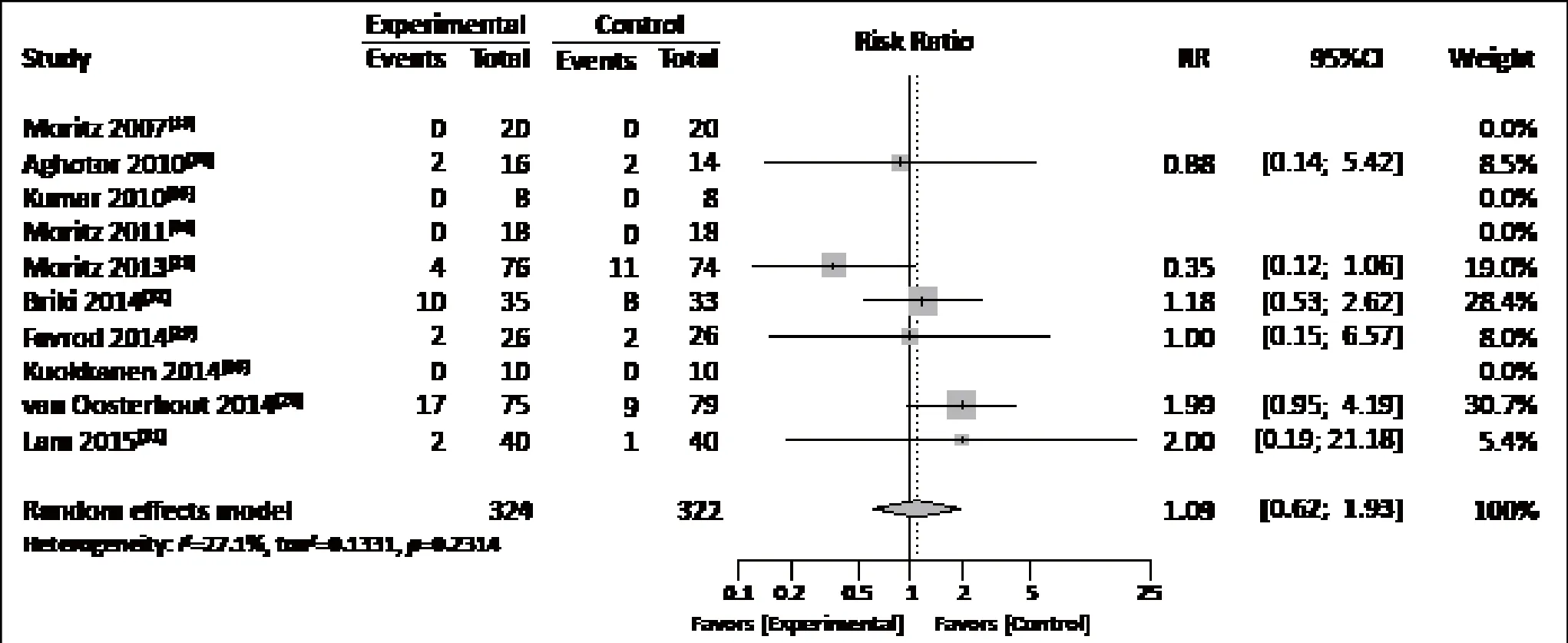
Figure 4. Forest plot of the proportion of enrolled participants who dropped out of the study
4. Discussion
4.1 Main findings
The primary goal of this meta-analytic review was to assess the effectiveness of adjunctive treatment with meta-cognitive training for patients with schizophrenia who are receiving standard psychopharmacological treatment. Unfortunately, the small number of RCTs for MCT in schizophrenia identified and the wide diversity in the measures used to assess the outcomes of these studies made it impossible to synthesize most of the results. Only three measures were reported in enough studies to merit pooling the results. a) Based on four studies, there was a small but statistically significant greater reduction in the positive symptoms subscale score of the PANSS at the end of treatment in the MCT group compared to the control group. Results across these four groups were homogeneous, supporting the conclusion that this is a ‘real’ result, not a statistical artifact. b) Based on four studies, the delusions subscale score of the PSYRATS at the end of the treatment was not significantly different between the groups. Results across the four studies were heterogeneous; subgroup analysis found that results for the two studies that used other types of psychotherapy as a control condition and the three studies that were rated as ‘non-high-quality’studies were homogeneous and there was a statistically significant advantage of MCT over the control condition in the three ‘non-high-quality’ studies. c) Based on all ten included studies, the dropout rate in the two groups was not statistically significant.
Qualitative assessment of the results from the studies that could not be pooled did not provide a clear picture about the potential efficacy of MCT for schizophrenia. Some findings indicated a trend in favor of MCT but other findings showed no difference in the outcomes between the two groups. Results for the four studies that assessed outcomes at different follow-up periods after the intervention were contradictory.
There were several possible reasons for the lack of definitive results. The sample sizes for some of the analyses were too small to produce statistically significant differences. The measures used may not have been sensitive to the specific cognitive biases addressed by MCT. The intensity and duration of the intervention– 8 to 16 group sessions over 4 to 8 weeks – may not be sufficient to produce the intended effect (standard CBTp for schizophrenia involves at least 16 one-to-one sessions[37]). Finally, MCT may not be effective.
4.2 Limitati ons
MCT for schizophrenia has only emerged over the last decade so it is not surprising that we were only able to identify a few randomized controlled trials.Consideration of studies in other languages may have increased the number of available studies for the review, but we found no studies in the Chineselanguage literature so it is doubtful that many highquality studies would be available in other non-English databases.[38]Another problem is that the methods and timing of assessing outcomes for MCT have not yet been standardized, so the studies used a variety of measures in a variety of ways making it impossible to include many of the available RCTs in a pooled meta-analysis.Finally, the available studies had several methodological and analytic limitations that limited the robustness of findings based on these results.
4.3 Implications
Overall, the small number of studies that could be synthesized in a meta-analysis, the limited number of measures for which comparable data were available across studies (i.e., the positive subscale of PANSS, the delusion subscale of PSYRATS, and the drop-out rate),and the small number of studies for which follow-up assessments (after the end of the intervention) were conducted make it impossible to come to a conclusion about the effectiveness of this adjunctive treatment for schizophrenia. More randomized trials that use standardized global outcome and cognition-specific outcome measures, that use ITT analyses, and that follow-up participants at regular intervals after the intervention are needed to determine whether or not MCT should become a recommended adjunctive treatment for schizophrenia. If MCT proves effective,further work will be needed to determine the best intensity and duration of the intervention (i.e., how many MCT sessions over what period of ti me) and the appropriate interval between MCT booster sessions.
Conflict of interest
The authors report no conflict of interest related to this manuscript.
Acknowledgment
We thank the reviewers of this analysis for their useful comments.
Funding
This study was funded by the Science and Technology Commission of Shanghai Municipality (13z2260500); the Shanghai Municipal Commission of Health and Family Planning (2013ZYJB0020); the Shanghai Shen Kang Hospital Development Center (SHDC12014111); and the Shanghai Health System Leadership in Health Research Program (XBR2011005).
1. World Health Organization[Internet]. World Health Organization; 2015 [cited 2015 June]. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). version 2015. Available from: http://apps.who.int/classi fi cations/icd10/browse/2015/en#/F20-F29
2. American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders (DSM V-5th edition).Virginia:American Psychiatric Publishing; 2013. p. 97-327
3. World Health Organization.Report of the international pilot study of schizophrenia. Geneva: World Health Organizati on;1973
4. McGrath J, Saha S, Chant D, Welham J. Schizophrenia:a concise overview of incidence, prevalence, and mortality.Epidemiologic reviews.2008; 30(1): 67-76. doi:http://dx.doi.org/10.1093/epirev/mxn001
5. Drake RE, Bebout RR, Roach JP. (1993). A research evaluati on of social network case management for homeless persons with dual disorders. Edited by Maxine Harris and Helen Bergman. Case management for mentally ill patients: theory and practice.Switzerland: Harwood Academic Publishers;1993. p.83-98
6. Mueser KT, McGurk SR. Schizophrenia.The Lancet.2004;363(9426): 2063-2072. doi: http://dx.doi.org/10.1016/S0140-6736(04)16458-1
7. van Os J, Kapur S. Schizophrenia.The Lancet.2009;374(9690): 635-645. doi: http://dx.doi.org/10.1016/S0140-6736(09)60995-8
8. Zink M, Englisch S, Meyer-Lindenberg A. [Polypharmacy in schizophrenia].Nervenarzt.2011; 82(7): 853-858. German
9. Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor.Schizophr Bull. 2008; 34(3): 523-537.doi: http://dx.doi.org/10.1093/schbul/sbm114
10. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE.A cognitive model of the positive symptoms of psychosis.Psychol Med.2001; 31(02): 189-195
11. Morrison AP. The interpretation of intrusions in psychosis:an integrative cognitive approach to hallucinations and delusions.Behav Cogn Psychother.2001; 29(03): 257-276
12. Freeman D. Suspicious minds: the psychology of persecutory delusions.Clin Psychol Rev.2007; 27(4): 425-457. doi: http://dx.doi.org/10.1016/j.cpr.2006.10.004
13. Fine C, Gardner M, Craigie J, Gold I. Hopping, skipping or jumping to conclusions? Clarifying the role of the JTC bias in delusions.Cogn Neuropsychiatry.2007; 12(1): 46-77. doi:http://dx.doi.org/10.1080/13546800600750597
14. Freeman D, Garety P, Kuipers E, Colbert S, Jolley S, Fowler D,et al. Delusions and decision-making style: use of the Need for Closure Scale.Behav Res Ther.2006; 44(8): 1147-1158.doi: http://dx.doi.org/10.1016/j.brat.2005.09.002
15. Riccaboni R, Fresi F, Bosia M, Buonocore M, Leiba N, Smeraldi E, et al. Patterns of evidence integration in schizophrenia and delusion.Psychiatry Res.2012; 200(2): 108-114. doi:http://dx.doi.org/10.1016/j.psychres.2012.04.005
16. Garety PA, Freeman D. Cognitive approaches to delusions:a criti cal review of theories and evidence.Br J Clin Psychol.1999; 38(2): 113-154
17. Bhatt R, Laws KR, McKenna PJ. False memory in schizophrenia patients with and without delusions.Psychiatry Res.2010; 178(2): 260-265. doi: http://dx.doi.org/ 10.1016/j.psychres.2009.02.006
18. Moritz S, Woodward TS. Metacognitive training for schizophrenia patients (MCT): a pilot study on feasibility,treatment adherence, and subjective efficacy.German J Psychiatry.2007; 10(3): 69-78
19. Moritz S, Woodward TS. Metacognitive training in schizophrenia: from basic research to knowledge translati on and interventi on.Curr Opin Psychiatry.2007; 20(6): 619-625.doi: http://dx.doi.org/10.1097/YCO.0b013e3282f0b8ed
20. Moritz S, Veckenstedt R, Randjbar S, Vitzthum F, Woodward TS. Antipsychotic treatment beyond antipsychotics:metacognitive intervention for schizophrenia patients improves delusional symptoms.Psychol Med.2011; 41(09): 1823-1832. doi: http://dx.doi.org/10.1017/S0033291710002618
21. Moritz S, Veckenstedt R, Bohn F, Hottenrott B, Scheu F,Randjbar S, et al. Complementary group Metacognitive Training (MCT) reduces delusional ideation in schizophrenia.Schizophre Res.2013; 151(1): 61-69. doi:http://dx.doi.org/10.1016/j.schres.2013.10.007
22. Moritz S, Veckenstedt R, Andreou C, Bohn F, Hott enrott , B,Leighton L, et al. Sustained and “sleeper” effects of group metacognitive training for schizophrenia: a randomized clinical trial.JAMA Psychiatry.2014; 71(10): 1103-1111. doi:http://dx.doi.org/10.1001/jamapsychiatry
23. American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. DSM IV-4th edition. Virginia:American Psychiatric Publishing; 1995
24. World Health Organization.International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). World Health Organizati on; 2015
25. Kay SR, Flszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia.Schizophre Bull.1987; 13(2): 261
26. Altman DG, Bland JM. Stati stics Notes: Detecting skewness from summary information.BMJ.1996; 313(7066): 1200
27. Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.2 [Internet].The Cochrane Collaboration; 2009 [updated September 2009]. Available from: http://handbook.cochrane.org
28. van Oosterhout B, Krabbendam L, de Boer K, Ferwerda J, van der Helm M, Stant AD, et al. Metacognitive group training for schizophrenia spectrum patients with delusions: a randomized controlled trial.Psychol Med.2014; 44(14): 3025-3035. doi: http://dx.doi.org/10.1017/S0033291714000555
29. Favrod J, Rexhaj S, Bardy S, Ferrari P, Hayoz C, Moritz S, et al. Sustained anti psychotic effect of metacognitive training in psychosis: A randomized-controlled study.Eur Psychiatry.2014; 29(5): 275-281. doi: http://dx.doi.org/10.1016/j.eurpsy.2013.08.003
30. Aghotor J, Pfueller U, Moritz S, Weisbrod M, Roesch-Ely D.Metacognitive training for patients with schizophrenia (MCT):feasibility and preliminary evidence for its efficacy.J Behav Ther Exp Psychiatry.2010; 41(3): 207-211. doi: http://dx.doi.org/10.1016/j.jbtep.2010.01.004
31. Lam KC, Ho CP, Wa JC, Chan SM, Yam KK, Yeung OS, et al.Metacognitive training (MCT) for schizophrenia improves cognitive insight: A randomized controlled trial in a Chinese sample with schizophrenia spectrum disorders.Behav Res Ther.2015; 64:38-42. doi: http://dx.doi.org/10.1016/j.brat.2014.11.008
32. Briki M, Monnin J, Haffen E, Sechter D, Favrod J, Netillard C, et al. Metacognitive training for schizophrenia: A multicentrerandomised controlled trial.Schizophre Res.2014; 157(1): 99-106. doi: http://dx.doi.org/10.1016/j.schres.2014.06.005
33. Kuokkanen R, Lappalainen R, Repo-Tiihonen E, Tiihonen J.Metacognitive group training for forensic and dangerous non-forensic patients with schizophrenia: A randomised controlled feasibility trial.Crim Behav Ment Health. 2014;24(5): 345-357. doi: http://dx.doi.org/10.1002/cbm.1905
34. Moritz S, Kerstan A, Veckenstedt R, Randjbar S, Vitzthum F, Schmidt C, et al. Further evidence for the efficacy of a metacognitive group training in schizophrenia.Behav Res Ther.2011; 49(3): 151-157. doi: http://dx.doi.org/10.1016/j.brat.2010.11.010
35. Kumar D, Zia Ul, Haq M, Dubey I, Doti vala KN, Veqar Siddiqui S, et al. effect of meta-cognitive training in the reduction of positive symptoms in schizophrenia.Eur J Psychotherapy Counsel.2010; 12(2): 149-158
36. Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS).Psychol Med.1999; 29(04): 879-889
37. National Institute for Health and Care Excellence.Schizophrenia (NICE clinical guidelines 178)[Internet].National Institute for Health and Care Excellence 2014;c2014 [Update February 2014; cited 2015 June]. Available from: http://www.nice.org.uk/cg178
38. Morrison A, Polisena J, Husereau D, Moulton K, Clark M,Fiander M, Rabb D. The effect of English-language restricti on on systematic review-based meta-analyses: a systematic review of empirical studies.Int J Technol Assess Health Care.2012; 28(02): 138-144. doi: http://dx.doi.org/10.1017/S0266462312000086
, 2015-06-09; accepted, 2015-06-20)

Dr. Jiangling Jiang graduated with a Bachelor’s degree in Medicine from Tongji Medical College,Huazhong University of Science and Technology, Wuhan, China in 2014. He is currently a postgraduate fellow at Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine. His main research interests include basic and clinical aspects of schizophrenia and evidence-based psychiatry.
精神分裂症进行元认知训练:一项系统综述
蒋江灵,张丽,朱智佩,李伟,李春波
元认知训练;精神分裂症;随机对照试验;Meta分析
Background: Metacognitive training (MCT) is a novel group psychotherapy method for schizophrenia, but there is, as yet, no conclusive evidence of its efficacy.Aims: Conduct a meta-analysis to assess the effectiveness of MCT in schizophrenia.Methods: Electronic and hand searches were conducted to identify randomized controlled trials about the effects of MCT in schizophrenia that met pre-de fined inclusion criteria. The Cochrane Risk of Bias tool was employed to assess of risk of biases, and Cochrane Review Manager version 5.3 and R version 3.1.1 were used to conduct the data synthesis.Results: Ten trials from 54 unduplicated reports were included in the review, but differences in the methods of assessing outcomes limited the number of studies that could be included in the meta-analysis. Pooling four studies that assessed the positive symptom subscale of the positive and Negative Syndrome Scale (PANSS)at the end of the trial identified a small but statistically significant greater reducti on in the MCT group than in the control group. But pooling four studies that assessed the delusion subscale of the psychotic Symptom Rating Scales (PSYRATS) at the end of the trial found no significant difference between the groups. Results from the qualitative assessment of the other results that could not be pooled across studies were mixed,some showed a trend in favor of MCT but many found no difference between the groups.Conclusions: The limited number of RCT trials, the variability of the method and time of the outcome evaluati on, and methodological problems in the trials make it impossible to come to a conclusion about the effectiveness of MCT for schizophrenia. More randomized trials that use standardized outcome measures,that use intention-to-treat (ITT) analyses, and that follow-up participants at regular intervals after the intervention are needed to determine whether or not MCT should become a recommended adjunctive treatment for schizophrenia.Registrati on number: PROSPERO CRD42015016609
[Shanghai Arch Psychiatry. 2015, 27(3): 149-157.
http://dx.doi.org/10.11919/j.issn.1002-0829.215065]
Shanghai Key Laboratory of psychotic Disorders, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
*correspondence: chunbo_li@163.com
背景:元认知训练(metacognitive training, MCT)是一组全新的针对精神分裂症的心理治疗方法,但是到目前为止还没有确凿的证据证实其疗效。目的:采用meta分析评估MCT治疗精神分裂症的有效性。方法:使用电子检索和手工检索的方法筛查文献,从而识别出有关MCT治疗精神分裂症疗效的随机对照试验(randomized controlled trials, RCT),这些RCT都满足预先规定的纳入标准。本研究采用Cochrane风险评估偏倚工具评估各种偏倚的风险性,并使用Cochrane Review Manager 5.3版和R 3.1.1版进行数据合成。结果:54项不重复报告中的10项试验被纳入,但评估结果方法上的差异限制了可能被纳入meta分析的研究数量。综合分析了四项在试验结束时使用阳性和阴性症状量表(Positive and Negative Syndrome Scale,PANSS)的研究,发现MCT组比对照组有一个较小的降低,但具有统计学意义。但综合四项在试验结束时使用精神病症状评定量表(Psychotic Symptom Rating Scales, PSYRATS)的错觉分量表的研究,发现两组间无显著差异。将那些无法汇集的各研究的其它结果进行定性的综合分析,显示出一些有利于MCT的趋势,但多数发现两组之间是没有差异的。结论:纳入的RCT试验数量有限、各试验结果评价的方法和时间的多样性、以及方法学上的问题使我们无法得出一个关于使用MCT治疗精神分裂症的有效性的结论。我们需要更多的使用标准化的结果评估方法、使用意向性治疗(intention-to-treat ITT)分析、以及在干预后对参与者进行有规律的定期随访的随机试验,从而确定MCT是否应该成为一个值得推荐的精神分裂症辅助治疗。
本文全文中文版从2015年08月06日起在http://dx.doi.org/10.11919/j.issn.1002-0829.215065可供免费阅览下载
- 上海精神医学的其它文章
- Meta-analysis for psychiatric research using free soft ware R
- Development of a checklist of short-term and long-term psychological symptoms associated with ketamine use
- Oligodendroglioma presenti ng as chronic mania
- Comparisons of family environment between homeless and non-homeless individuals with schizophrenia in Xiangtan, Hunan
- Abnormal inter- and intra-hemispheric integrati on in male paranoid schizophrenia: a graph-theoreti cal analysis
- Addressing risk of bias in trials of cognitive behavioral therapy

