完全腹腔镜远端胃癌D2根治术在进展期胃癌中的临床应用价值
沈乃营++何盟国+刘昌++++++王智翔
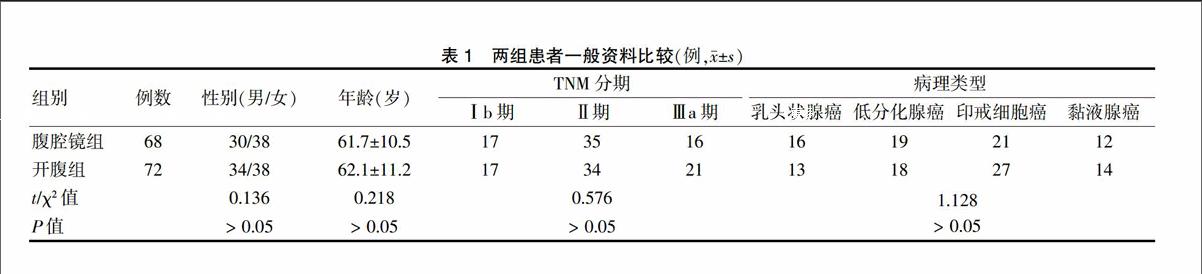
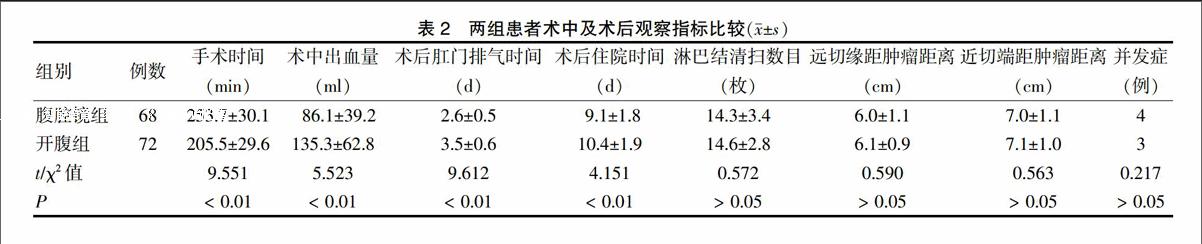
[摘要] 目的 对比分析完全腹腔镜与开腹远端胃癌D2根治术在进展期胃癌中的应用价值。 方法 回顾性分析2009年1月~2012年2月陕西核工业二一五医院收治的接受完全腹腔镜胃癌D2根治手术的进展期胃癌患者68例(腹腔镜组)及接受开腹胃癌D2根治手术的进展期胃癌患者72例(开腹组)的临床资料,对比分析两组所用手术时间、术中出血量、术后肛门排气时间、术后住院时间、术后并发症、淋巴结清除数、肿瘤距远近切缘距离、1年及3年生存率。 结果 腹腔镜组手术时间明显较开腹组长,但术中出血量明显较开腹组少,差异均有高度统计学意义(P < 0.01);腹腔镜组的术后肛门排气时间、术后住院时间均少于开腹组,差异均有高度统计学意义(P < 0.01);两组淋巴结清扫数目比较,差异无统计学意义(P > 0.05);两组距远、近切端距肿瘤距离比较,差异无统计学意义(P > 0.05)。两组术后并发症发生率比较,差异无统计学意义(P > 0.05)。腹腔镜组的1、3年生存率分别为100.0%、89.7%,开腹组分别为100.0%、90.3%,差异均无统计学意义(P > 0.05)。 结论 完全腹腔镜远端胃癌D2根治术治疗进展期胃癌是安全、可行的,可以达到与开腹手术同样的根治效果。
[关键词] 腹腔镜手术;D2根治术;进展期胃癌
[中图分类号] R735.2 [文献标识码] A [文章编号] 1673-7210(2015)10(b)-0013-04
Clinical application value of totally laparoscopic D2 gastrectomy for advanced gastric cancer
SHEN Naiying1.2 HE Mengguo1 LIU Chang2 WANG Zhixiang1
1.Department of Hepatobiliary Surgery, Shaanxi Nuclear Geology 215 Hospital, Shaanxi Province, Xianyang 712000, China; 2.Department of Hepatobiliary Surgery, the First Affiliated Hospital of Xi'an Jiaotong University, Shaanxi Province, Xi'an 711061, China
[Abstract] Objective To investigate the clinical value of totally laparoscopy D2 surgery for advanced gastric cancer by thecomparative analysis of totally laparoscopy and open the distal gastric D2 radical surgery. Methods From January 2009 to February 2012, the clinical data of 68 patients with advanced gastric cancer received totally laparoscopy (laparoscopy group) and 72 patients with advanced gastric cancer received open surgery (open surgery group) in Shaanxi Nuclear Geology 215 Hospital were analyzed. Clinical parameters including operation time, blood loss, postoperative exhausting time, postoperative hospital stay, complications, and the number of lymph nodes dissected, length of proximal and distal margin to the cancer, 1-year and 3-year survival rates of two groups were observed. Results The operation time in laparoscopic group was longer than that in open surgery group, but the volume of bleeding was less than that in laparoscopic group, the differences were statistically significant(P < 0.01); and the postoperative exhausting time and hospital stay after operation were shorter than that in open surgery group, the difference were statistically significant (P < 0.01). Compared the number of lymphadenectomy in the two groups , the difference was not statistically significant (P > 0.05). There were no significant differences between two groups in rate of complications, number of lymph nodes and length of proximal and distal margin to the cancer (P > 0.05). The 1-year and 3-year survival rates were 100.0%, 89.7% in laparoscopy group and 100.0%, 90.3% in open surgery group respectively, and there were no significant differences between two groups (P > 0.05). Conclusion Totally laparoscopic D2 gastrectomy is safe and feasible for advanced gastric cancer, and has similar radical effect compared with open surgery.

