张力带钢丝固定转子间四部分骨折合并髋关节疾病的全髋关节置换疗效分析
曹参 杨静 裴福兴 沈彬 周宗科 康鹏德
. 论著 Original article .
张力带钢丝固定转子间四部分骨折合并髋关节疾病的全髋关节置换疗效分析
曹参 杨静 裴福兴 沈彬 周宗科 康鹏德
目的 探讨全髋关节置换结合张力带钢丝固定治疗合并髋关节疾病的转子间四部分骨折的手术方法及疗效。方法 纳入 2005 年 9 月至 2009 年 9 月,于华西医院骨科采用全涂层有领股骨假体行全髋关节置换治疗转子间四部分骨折合并髋关节疾病患者 28 例。其中,骨折前合并骨关节炎 19 例,合并髋关节发育不良骨关节炎 4 例,合并股骨头坏死 2 例,合并类风湿性髋关节炎 3 例,髋臼侧均有病变累及。骨折类型为四部分骨折,即 Evans-Jensen III 型。术前行疼痛视觉模拟 ( visual analogue scales,VAS ) 评分,术前、术后第 2 天常规 X 线摄片,术后 1、2、3、6、12 个月门诊随访,以后每年 1 次。每次随访均行 Harris 评分,VAS 评分,X 线摄片及体格检查。至骨折愈合前每月行 X 线检查 1 次。结果 所有患者随访 5~8 年,平均6.3 年。术后 1 个月 Harris 评分平均 ( 69.4±7.3 ) 分,术后半年平均 ( 90.3±5.7 ) 分,末次随访平均 ( 92.4± 5.6 ) 分,21 例为优,5 例为良,2 为可,优良率为 92.8%。术后半年 Harris 评分高于术后 1 个月,差异有统计学意义 ( t=-47.55,P=0.00 ),末次随访高于术后半年,差异有统计学意义 ( t=-8.87,P=0.00 )。术前 VAS评分平均为 ( 6.0±1.0 ) 分,术后 1 个月平均为 ( 2.0±0.7 ) 分,末次随访平均为 ( 0.5±0.6 ) 分,术后 1 个月低于术前,差异有统计学意义 ( t=28.69,P=0.00 ),末次随访低于术后 1 个月,差异有统计学意义 ( t=8.80,P=0.00 )。1 例术后 2 周因摔倒致后脱位,行闭合复位,后未再发生脱位。所有患者术后第 2 天 X 线片均显示假体压配满意,骨折术后 4 个月均已愈合,钢丝无断裂,至末次随访假体均无松动、下沉,无假体周围骨折,无深部感染,Trendelenburg 征均阴性,无明显跛行。结论 全涂层有领股骨假体全髋关节置换结合张力带钢丝捆绑固定大、小转子骨折块治疗合并髋关节疾病的转子间四部分骨折可取得良好的疗效。
髋骨折;关节成形术,置换,髋;骨折固定术,内;髋假体
股骨转子间骨折在老年人是一个常见问题,且随着人口老龄化及骨质疏松的增加,转子间骨折发病率不断增加,其中不稳定骨折约占 35%~40%,给家庭和社会带来了巨大的负担[1]。越来越多的作者报道了此类患者行半髋及全髋关节置换取得的良好效果[2-3]。在临床上,骨折前已合并骨关节炎,髋关节发育不良,股骨头坏死,类风湿性髋关节炎等髋关节疾病的患者并不少见,有行全髋关节置换术的适应证。我院于 2005 年 9 月至 2009 年9 月,对合并髋关节疾病的转子间四部分骨折患者行采用非骨水泥型全涂层有领股骨假体 ( AML,强生公司 ) 的全髋关节置换术结合张力带钢丝捆绑固定大、小转子骨折块 28 例,收到良好的效果。现报道如下。
资料与方法
一、临床资料
本组 28 例,男 13 例,女 15 例,年龄 58~79 岁,平均 69.6 岁。其中,骨折前合并骨关节炎19 例,合并髋关节发育不良骨关节炎 4 例,合并股骨头坏死 2 例,合并类风湿性髋关节炎 3 例,髋臼侧均有病变累及。骨折类型为 Evans-Jensen III 型。大部分患者合并内科系统疾病,其中高血压 12 例,糖尿病 6 例,冠心病 8 例,慢性支气管炎 3 例,慢性肾功能不全 2 例,有些患者同时合并 2 种甚至3 种疾病。
二、手术方法
手术均采用全身麻醉,后外侧入路,均采用非骨水泥型全涂层有领假体柄 ( AML )。充分显露髋臼和骨折断端,先对骨折进行暂时复位,复位后用骨折复位钳钳夹或钢丝捆绑临时固定骨折,再行髋关节脱位、截断股骨颈,保留股骨距。取出股骨头显露髋臼,先行髋臼侧置换。股骨侧扩髓至适当大小后再插入股骨假体试模。置入假体时用假体领压住复位的股骨距及小转子,再以假体为支撑对大、小转子进行复位捆绑。一般采用 3 根 1 mm 粗双股钢丝 ( 图 1 )。大转子用 2 根双股钢丝依“张力带固定原则”固定,大转子骨折块中上部钻孔后 A 钢丝穿过,双股钢丝向下方于股外侧肌下方交叉后再向内侧绕至小转子下部,先收紧钢丝再拧紧固定;B 钢丝同样穿过钻孔的大转子块,钻洞位于大转子骨折块中部,绕至小转子下部或上部,收紧钢丝拧紧固定。据小转子复位固定情况,可加用 1 根或数根双股钢丝环扎小转子。C 钢丝位于大转子下股外侧肌下方,向内绕至小转子上,收紧钢丝拧紧固定。通过假体领及 3 根钢丝的共同作用,保证大、小转子的牢靠固定。术毕留置引流管 1 根,逐层缝合切口。因骨折块大小、形状,复位后稳定性等情况的个体差异,在遵循张力带固定的原则上,钢丝捆绑方式可做灵活调整 ( 图 2 )。
三、围手术期处理
除对内科合并疾病的评估及处理外,术前常规下肢静脉彩超了解有无血栓;皮肤切开前 30 min 给予预防性抗生素 1 次,手术时间超过 3 h 加用抗生素 1 次;术后常规低分子肝素钙抗凝预防下肢深静脉血栓形成,高危患者加用间断性足底静脉泵。48 h 内拔除引流管。麻醉清醒后行踝关节主动屈伸运动,术后第 2 天下床活动,患肢部分负重 1 个月,坚持行髋部屈曲及外展肌力锻炼。
四、疗效评价
术前行疼痛视觉模拟评分 ( visual analoguescales,VAS ),术前、术后第 2 天常规 X 线摄片,术后 1、2、3、6、12 个月门诊随访,以后每年1 次。每次随访均行 Harris 评分,VAS 评分,X 线摄片及体格检查。至骨折愈合前每月行 X 线检查1 次。X 线摄片评价假体位置是否满意、大小转子骨折块是否愈合、钢丝有无断裂、有无松动、下沉、有无假体周围骨折及假体周围感染征象,用 Engh等[4]所用的方法判断股骨假体压配及“骨长入”情况;X 线片结合查体检查患者双下肢长度差异。同时记录有无跋行及其它各种术后并发症。以各种原因所致翻修或患者死亡为随访终点。Harris 评分:总分 100 分,≥90 分为优,81~90 分为良,70~80 分为可,<70 分为差。VAS 评分:在纸上面划一条 10 cm 的横线,横线的一端为 0,另一端为 10。0 分:无痛;1~3 分:有轻微的疼痛,能忍受;4~6 分:患者疼痛并影响睡眠,尚能忍受;7~10 分:患者有渐强烈的疼痛,疼痛难忍,影响食欲,影响睡眠。让患者根据自我感觉在横线上划一记号,表示疼痛的程度。
五、统计学处理
采用 SPSS 13.0 统计软件对术后 Harris 评分及术前术后 VAS 评分结果进行处理,两两比较采用配对t 检验,检验水准为 0.05,数据用±s 表示。

图 1 左示大、小转子的双股钢丝捆绑方式,实线示骨前方钢丝,虚线示骨后方钢丝;右为典型术后 X 线片图 2 患者,女,74 岁,合并有类风湿性髋关节炎,此为术后第 2 天 X 线片。大转子的固定依一般方法中 A、B 钢丝捆绑方法固定,因下转子骨折块较小,在假体领及钢丝的作用下以已达牢靠固定,故未用 C 钢丝Fig.1 The left part showed how double-strand wires tied. The full lines mean in front of the bone, and the dotted lines mean behind the bone. The right part was the typical postoperative X-ray flm.Fig.2 Postoperative X-ray flm of a 74 years old womanwho had rheumatoid arthritis of the hip. The greater trochanter was fxed in a general way. The lesser trochanter fragment was quite small, and was frm after A and B wires, therefore C wire was not used.
结 果
所有患者均在入院 72 h 内顺利完成手术。所有患者随访 5~8 年,平均 6.3 年。术后 1 个月 Harris评分平均 ( 69.4±7.3 ) 分,半年平均 ( 90.3±5.7 )分,末次随访平均 ( 92.4±5.6 ) 分,21 例为优,5 例为良,2 为可,优良率为 92.8%。术后半年 Harris评分高于术后 1 个月,差异有统计学意义 ( t= -47.55,P=0.00 ),末次随访高于术后半年,差异有统计学意义 ( t=-8.87,P=0.00 )。术前 VAS 评分平均为 ( 6.0±1.0 ) 分,术后 1 个月平均为 ( 2.0±0.7 )分,末次随访平均为 ( 0.5±0.6 ) 分,术后 1 个月低于术前,差异有统计学意义 ( t=28.69,P=0.00 ),末次随访低于术后 1 个月,差异有统计学意义 ( t= 8.80,P=0.00 )。1 例术后 2 周因摔倒致后脱位,行闭合复位,后未再发生脱位。所有患者术后第 2 天X 线片均显示假体位置满意,压配满意,骨折术后4 个月均已愈合,钢丝无断裂,至末次随访假体均无松动、下沉,影像学显示其中“骨长入”27 例,“稳定纤维长入”1 例,无假体周围骨折,无深部感染,双下肢长度差异均<6 mm,Trendelenburg 征均阴性,无明显跛行。
讨 论
一、手术方式的选择
单纯转子间骨折的治疗,主流有内固定和关节置换两种方式,对于一些患者手术方式的选择有争议[2-3,5]。但对于此组骨折前合并髋臼侧有病变的髋关节疾病的患者,行内固定术治疗后关节疼痛依然存在,且因髋关节疾病引起的疼痛,关节活动度降低,软组织挛缩甚至关节僵硬,致患者活动过程中内固定物固定处应力增高,影响骨折愈合[6]。行全髋关节置换术可以一次性解决骨折及合并髋关节疾病的双重问题,是此类患者的最佳选择。
二、股骨侧假体的选择
本组患者选用全涂层有领股骨假体 ( AML )。选择非骨水泥假体,而不选择骨水泥假体。转子间骨折常常发生在骨质疏松的老年人,Choy 等[7]的研究证实,骨质疏松并不影响现代非骨水泥假体 ( AML假体 ) 的固定效果,即使是在 Singh 指数 3 级以下的重度骨质疏松患者,仍可取得良好的固定效果,且 40 例平均随访 40.5 个月,无 1 例假体周围骨折发生。骨水泥假体在假体击入时,因骨折的存在,影响骨水泥加压,且骨水泥有进入骨折缝影响骨折愈合的可能。假体松动是影响假体使用寿命的重要因素,Engh 等[4]通过 X 线片评价非骨水泥股骨假体是否达初始压配固定,且将远期固定分为“骨长入固定”、“稳定纤维长入固定”和“不稳定固定”三种,其结果提示是否达初始压配固定对假体松动率的影响极为重要。因转子间骨折的存在,假体近端初始稳定性不能保证,故本组选用全涂层的远端固定假体。假体领可压住股骨距,有助于小转子部位骨折片的固定,故本组选用有领假体。本组患者全部达到初始压配固定,末次随访均显示为稳定固定,且“骨长入固定”率达 96.4%,与 Engh 等初始压配固定组相当。
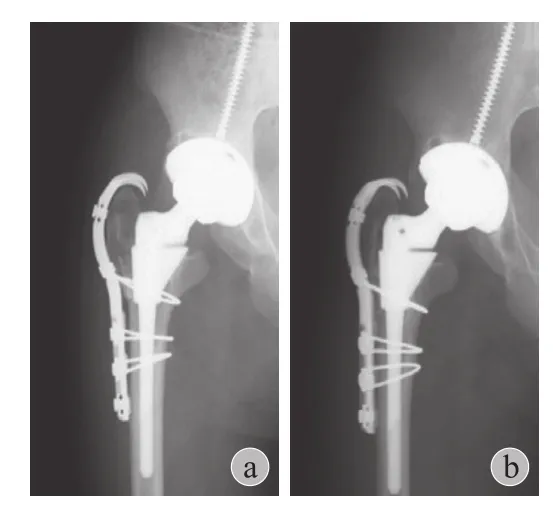
图 3 示钢索爪板系统固定大转子块 [13]。a 为术后 3 个月 X 线片,b 为术后 12 个月 X 线片,示大转子已骨性愈合Fig.3 Cited from the article of Patel S [13], showing the cable-plate device. ( a ) was the X-ray film 3 months postoperatively, and ( b ) was the X-ray film 12 months postoperatively when thegreater trochanter had obtained bony union
三、张力带钢丝固定方法
大转子骨折块的固定在此类患者很重要,大转子不愈合可以导致术后脱位风险增高和 Trendelenburg步态等问题[8-9]。大转子骨折块的固定有钢丝、钢索、钢索-爪板系统、锁定钢板等方式 ( 图 3 )[10-13]。钢索-爪板系统和锁定钢板固定方法可取得满意的固定效果,但费用昂贵。钢丝及钢索固定应用较多,实验研究显示,双股钢丝固定可取得与钢索固定同等的压力,但经济性较钢索优越[14]。钢丝捆扎固定的方法多种多样,延迟愈合或不愈合等并发症并不少见。本组采用双股钢丝,在大转子上钻孔固定,如图 1 所示,A 钢丝提供向下拉力抵抗大转子向上移位,B 钢丝防止 A 钢丝造成大转子上端向外翘起,同时 A、B 两根钢丝组成张力带,变肌肉牵拉大转子的张应力为骨折块之间的压应力,促进骨折的愈合。此方法在本组患者取得了满意的临床效果,无大转子不愈合发生。
综上所述,全涂层有领股骨假体全髋关节置换结合张力带钢丝捆绑固定大、小转子骨折块治疗合并髋关节疾病的股骨转子间四部分骨折,在适应证选择得当,围手术期管理得当,手术操作技术良好的前提下可有效避免术后并发症的发生,获得良好的术后效果。但本研究有样本量较小的不足之处,且远期效果有待进一步观察。
[1] Grimsrud C, Monzon RJ, Richman J, et al. Cemented hip arthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fractures. J Arthroplasty, 2005, 20(3): 337-343.
[2] Karthik K, Natarajan M. Unstable trochanteric fractures in elderly osteoporotic patients: role of primary hemiarthroplasty. Orthop Surg, 2012, 4(2):89-93.
[3] Sidhu AS, Singh AP, Singh AP, et al. Total hip replacement as primary treatment of unstable intertrochanteric fractures in elderly patients. Int Orthop, 2010, 34(6):789-792.
[4] Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg (Br), 1987,69(1):45-55.
[5] Gavaskar AS, Subramanian M, Tummala NC. Results of proximal femur nail antirotation for low velocity trochanteric fractures in elderly. Indian J Orthop, 2012, 46(5):556-560.
[6] Donegan RP, Garver JV, Lynch F, et al. Functional improvement after humeral shaft nonunion in a patient with glenohumeral ankylosis. Am J Orthop (Belle Mead NJ), 2013, 42(12):561-565.[7] Choy WS, Ahn JH, Ko JH, et al. Cementless bipolar hemiarthroplasty for unstable intertrochanteric fractures in elderly patients. Clin Orthop Surg, 2010, 2(4):221-226.
[8] Capello WN, Feinberg JR. Trochanteric excision following persistent nonunion of the greater trochanter. Orthopedics,2008, 31(7):711.
[9] Amstutz HC, Maki S. Complications of trochanteric osteotomy in total hip replacement. J Bone Joint Surg (Am), 1978, 60(2): 214-216.
[10] Lee YK, Ha YC, Chang BK, et al. Cementless bipolar hemiarthroplasty using a hydroxyapatite-coated long stem for osteoporotic unstable intertrochanteric fractures. J Arthroplasty, 2011,26(4):626-632.
[11] Barrack RL, Butler RA. Current status of trochanteric reattachment in complex total hip arthroplasty. Clin Orthop Relat Res, 2005, 441:237-242.
[12] Laflamme GY, Leduc S, Petit Y. Reattachment of complex femoral greater trochanteric nonunions with dual locking plates. J Arthroplasty, 2012, 27(4):638-642.
[13] Patel S, Soler JA, El-Husseiny M, et al. Trochanteric fxation using a third-generation cable device-minimum follow-up of 3 years. J Arthroplasty, 2012, 27(3):477-481.
[14] Liu A, O'Connor DO, Harris WH, et al. Comparison of cerclage techniques using a hose clamp versus monofilament cerclage wire or cable. J Arthroplasty, 1997, 12(7):772-776.
( 本文编辑:王永刚 )
Effects of total hip replacement combined with tension band wire fixation for intertrochanteric four-part fractures with hip diseases
CAO Can, YANG Jing, PEI Fu-xing, SHEN Bin, ZHOU Zong-ke, KANG Peng-de. Department of Orthopaedic Surgery, West China Hospital of Sichuan University, Chengdu, Sichuan, 610041, PRC
YANG Jing, Email: cd-yangjing@163.com
Objective To explore the surgical technique and effcacy of total hip replacement combined with tension band wire fixation for intertrochanteric four-part fractures with hip diseases. Methods Twenty-eight cases of intertrochanteric four-part fractures and hip diseases treated with total hip replacement by a full coated, collared femoral prosthesis from September, 2005 to September, 2009 were included. Before fracture, there were 19 cases with osteoarthritis, 4 cases with osteoarthritis secondary to hip developmental dysplasia, 2 cases with femoral head necrosis,3 cases with rheumatoid arthritis of hip, all acetabular sides had lesions involved. All were of four-part fractures ( type III in the Evans-Jensen classifcation ). Preoperatively, visual analogue scales ( VAS ) were marked. X-ray flms were taken before and the frst day after the surgery. Follow-up evaluations were performed at1, 2, 3, 6, and 12 months, and every year thereafter. Harris score and VAS were recorded, X-ray flms and physical examination were taken in each follow-up. Results All cases were followed for 5-8 years, with an average of 6.3 years. One month after the surgery,the average Harris score was 69.4±7.3. Half a year after the surgery, the average Harris score was 90.3±5.7. At the last follow-up, the average Harris score was 92.4±5.6. Results were excellent in 21 cases, good in 5 cases, fair in 2 cases, with an excellent and good rate of 92.8%. The score half a year after the surgery was signifcantly higher thanthat 1 month after the surgery with statistical signifcance ( t=-47.55, P=0.00 ), and the score at the last follow-up was signifcantly higher than that half a year after the surgery with statistical signifcance ( t=-8.87, P=0.00 ). Before the surgery, the average visual analogue scale was 6.0±1.0; 1 month after the surgery, the average scale was 2.0±0.7; at the last follow-up, the average scale was 0.5±0.6. The scale 1 month after the surgery was signifcantly lower than that before the surgery with statistical signifcance ( t=28.69, P=0.00 ), and the scale at the last follow-up was signifcantly higher than that 1 month after the surgery with statistical signifcance ( t=8.80, P=0.00 ). One patient had hip dislocation by falling 2 weeks after surgery, but no more dislocations happened after the closed reduction. All X-ray flms showed the satisfed press-ftting the day after surgery, and the prostheses were well fxed. At 4-months follow-up, all fractures healed with no wires broken. Until the last evaluation, there were not any complications of loosening, subsidence or periprosthetic fracture, deep infection. All trendelenburg signs were negative and no obvious limp. Conclusions Total hip replacement by a full coated, collared femoral prosthesis combined with tension band wire fxation of the greater and less trochanters fragments for intertrochanteric four-part fractures with hip diseases can gain satisfed outcomes.
Hip fractures; Arthroplasty, replacement, hip; Fracture fxation, internal; Hip prosthesis
10.3969/j.issn.2095-252X.2015.12.014
R687.4
卫生部 2013 年度卫生行业科研专项项目 ( 201302007 )作者单位:610041 成都,四川大学华西医院骨科
杨静,Email: cd-yangjing@163.com
2014-12-20 )