下颌部畸形26例治疗体会
韩思源, 贺佳妮, 冷 冰, 郭家妍, 李 怒, 左 娜, 刘海燕, 胡 枫
作者单位:110001 辽宁 沈阳,中国医科大学附属第一医院 整形外科
颌面整形
下颌部畸形26例治疗体会
韩思源, 贺佳妮, 冷 冰, 郭家妍, 李 怒, 左 娜, 刘海燕, 胡 枫
作者单位:110001 辽宁 沈阳,中国医科大学附属第一医院 整形外科
目的 总结近5年我科收治下颌部畸形的治疗经验,以指导临床工作。方法 收集26例下颌部畸形的病历资料,对其进行回顾性分析总结。安氏骨性Ⅲ类畸形、下颌前突、偏突颌畸形12例,其中,11例行下颌支矢状骨劈开术,1例行经口内入路下颌支垂直骨切开术,3例同期行颏成形术;下颌角肥大9例,其中,7例行下颌角外板劈开截除术,2例行下颌角磨骨术;小颏畸形5例,其中,3例行膨体隆颏术,2例行硅胶假体隆颏术。结果 所有患者术后效果满意,并发症发生率为7.69%。结论 下颌支矢状骨劈开术可以通过向前、向后移动或旋转远心骨段来完成下颌后缩、前突及偏突畸形的矫正,效果确切;下颌角磨骨术对于外翻型下颌角肥大治疗效果较好,对于下颌角肥大向外侧与后方较明显突出的患者应选用下颌角外板劈开截除术;填充颏成形术仅适用于轻、中度的小颏畸形,其他类型的畸形应考虑颏成形术。
下颌支矢状骨劈开术; 下颌前突; 偏突颌畸形; 下颌角肥大
1 临床资料
本组患者共26例。男性5例,女性21例;年龄17~39岁,平均22.7岁。10例患者存在颞下颌关节弹响。安氏骨性Ⅲ类畸形、下颌前突、偏突颌畸形12例,其中11例行下颌支矢状骨劈开术(sagittal split ramus osteotomy, SSRO),1例行经口内入路下颌支垂直骨切开术(intraoral vertical ramus osteotomy, IVRO),12例中3例同期行颏成形术;下颌角肥大9例,其中7例行下颌角外板劈开截除术,2例行下颌角磨骨术;小颏畸形5例,3例行膨体隆颏术;2例行硅胶假体隆颏术。
2 手术方法
2.1 安氏骨性Ⅲ类畸形、下颌前突、偏突颌畸形 治疗程序均按照术前正畸、模型外科、正颌手术、术后正畸与康复治疗[5]进行。术前颌面部三维CT重建按正颌手术要求精确测量。经鼻气管插管全身麻醉。11例患者行SSRO,远心骨段移动距离为3.00~13.00 mm,平均6.72 mm,以钛板与单皮质骨螺钉固定,其中2例患者同时行上颌Lefort Ⅰ型骨切开术,前徙距离分别为5.00 mm、7.00 mm,平均6.00 mm;前徙7.00 mm者,颧牙槽嵴处骨缺损用下颌骨截除外板进行植骨,钻孔后丝线缝合固定,其中3例患者同时行颏成形术。1例患者行IVRO,术后4周解除颌间橡皮圈固定。术后1个月左右开始术后正畸治疗,同时进行恢复颌周肌肉及颞颌关节功能的康复训练。
2.2 下颌角肥大 7例患者行下颌角外板劈开截除术(mandibular angle splitting ostectomy, MASO),按设计线截骨后至欲截除下颌角部分后,将下颌角部分骨质全层截断,并将截除的骨外板及下颌角部全层骨组织一并取出,打磨骨质边缘。2例下颌角外翻患者行下颌角磨骨术。
2.3 小颏畸形 经口内横切口行硅胶假体或膨体置入术,3例行膨体隆颏术,2例行硅胶假体隆颏术。
3 结果

4 典型病例

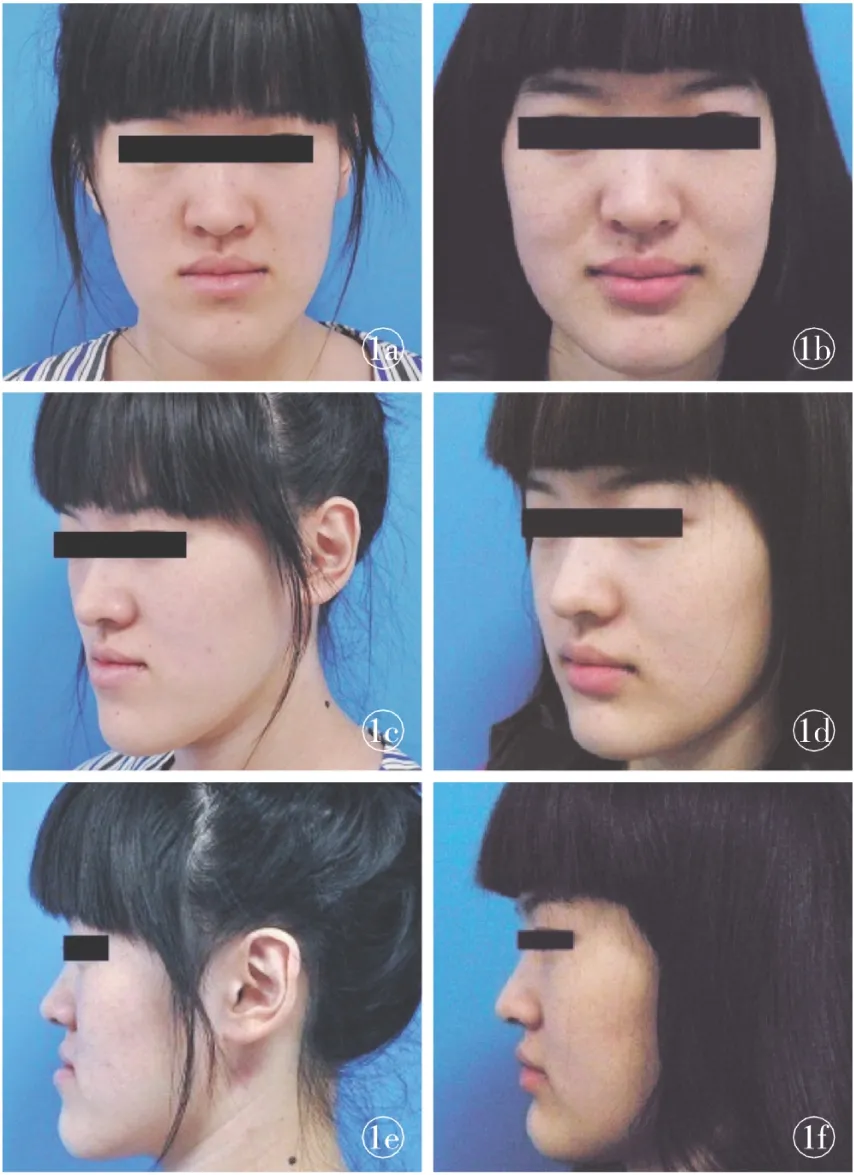
图1 下颌过度前突治疗前后对比 a.术前正位 b.术后1个月正位 c.术前斜位 d.术后1个月斜位 e. 术前侧位f. 术后1个月侧位
Fig 1 Comparison between preview and postview of the treatment of lower mandible with excessive protraction. a. frontal preview.b. frontal postview at 1 month. c. oblique preview. d. oblique postview at 1 month. e. lateral preview. f. lateral postview at 1 month.



Fig 2 Comparison between preview and postview of the treatment of bilateral SSRO. a. preview. b. postview at 1 month. c. preview with occlusion. d. postview with occlusion at 1 month.
5 讨论
5.1 安氏骨性Ⅲ类畸形、下颌前突、偏突颌畸形 目前,国际上公认的矫治术式有SSRO和IVRO[6-7]。使用最普遍的矫正下颌前突畸形的手术方法是SSRO[8],适用于矫正下颌发育不足和下颌发育过度,当伴有上颌发育不足、小颏畸形时可同期行上颌Lefort Ⅰ型骨切开术、颏成形术,手术顺序为上颌手术、下颌手术、颏部手术。术中应用钛板坚固内固定。改良的SSRO有如下优点:⑴口内切口,面部不留瘢痕;⑵矢状截骨使牙槽神经血管束得以完整保留,减少并发症的发生;⑶近远心骨段有较大的骨接触面,有利于骨段间愈合;⑷可以有很大的后退量, 有利于严重下颌前突的矫治[9];⑸对面部侧方形态影响不大,咀嚼肌适应迅速。两种截骨术改变了原来的颌骨形态和位置,也改变了颞下颌关节前、上、后间隙,从而导致髁突位置在术后也发生了改变。但因影响这种改变的因素复杂,移位方向也多种多样,有向前移位[10]、向内向后旋转[11],颞颌关节的各个间隙在术前术后也有明显改变[12]。IVRO由于术后不需要进行坚固内固定,术后近心端骨段可以发生旋转移位。Bell等[13-14]报道IVRO后髁状突向前向下移位,但是当全身神经肌肉恢复后,髁状突有回到原来位置的倾向[15]。有报道称,IVRO术后颞颌关节紊乱症状消失[16-18]。Lai等[19]建议应用单侧IVRO联合对侧SSRO的方法来改善下颌不对称畸形,同时改善颞颌关节紊乱的症状。
5.2 下颌角肥大 下颌角缩小成形术主要包括磨骨术和MASO。MASO适用于向外侧与后方较明显突出者,对于正面观下颌角骨质外翻的患者尤其适合磨骨术,术中需注意预防出血[20]。该术式不会导致骨折和颞下颌关节损伤,创伤小。本研究中应用MASO的下颌角肥大病例在操作中一次性将骨外板与下颌角截除,效果确切,值得推广。
5.3 小颏畸形 隆颏术作为常见的美容整形手术,手术难度不大,但易出现下唇外翻、假体移位等并发症。这些并发症的产生与切口的选择有关[21]。下唇及颏部有3对肌肉与口内切口相关,即颏肌、下唇方肌和下唇三角肌,作用均为降下唇,上提颏部皮肤[22]。切口应顺应颏肌、下唇方肌和下唇三角肌等肌肉的辐射状走向,最大程度地保留下唇正常解剖结构,可最大限度地减少术后并发症的发生,可以选用双侧纵切口及口内环系带U形切口。
下颌部畸形的矫治术式多种多样,但目前没有一种术式适合所有的下颌部畸形患者[23]。应根据畸形的类型,从下颌部整体轮廓考虑,制定最佳的手术方案,才能达到理想的美学效果。
[1] Lee ST, Mori Y, Minami K, et al. Does skeletal surgery for asymmetric mandibular prognathism influence the soft tissue contour and thickness[J]? J Oral Maxillofac Surg, 2013,71(9):1577-1587.
[2] Guglielmi M, Schneider KM, Iannetti G, et al. Orthognathic surgery for correction of patients with mandibular excess: don′t forget to assess the gonial angle [J]. J Oral Maxillofac Surg, 2013,71(6):1063-1072.
[3] Haraguchi S, Takada K, Yasuda Y. Facial asymmetry in subjects with skeletal Class Ⅲ deformity [J]. Angle Orthod, 2002,72(1):28-35.
[5] 张志愿. 口腔颌面外科学[M]. 7版. 北京:人民卫生出版社, 2014:502.
[6] Huseyin AB, Cenk K, Altan V, et al. A morphometric study of the maxillary artery and lingula in relation to mandibular ramus osteotomies and TMJ surgery[J]. Eur J Dent, 2010,4(2):166-170.
[7] Yazdani J, Talesh KT, Motamedi MH, et al. Changes in the gonial angle following bilateral sagittal split osteotomy and vertical ramus osteotomy for mandibular excess[J]. Eplasty, 2010,10(1):20-22.
[8] 任 敏, 滕 利, 归 来, 等. 口内入路改良下颌升支矢状劈开截骨术矫治下颌前突[J]. 中国美容医学, 2006,15(12):1383-1385.
[9] Guven O, S aracoglu U. Changes in pharyngeal airway space and hyoid bone positions af ter body ostectomies and sagittal split ramus osteotomies[J]. J Craniofac Surg, 2005,16(1):23-30.
[10] 杨学文, 龙 星, 叶翁三杰, 等. 正颌正畸联合治疗下颌偏突颌畸形[J]. 中华医学美学美容杂志, 2006,12(1):5-8.
[11] Baek SH, Kim TK, Kim MJ. Is there any difference in the condylar position and angulation after asymmetric mandibular setback[J]. Oral Surg Oral Pathol Oral Radiol Endod, 2006,101(2):155-163.
[12] Ueki K, Moroi A, Sotobori M, et al. Changes in temporomandibular joint and ramus after sagittal split ramus osteotomy in mandibular prognathiam patients with and without asymmetry[J]. J Craniomaxillofac Surg, 2012,40(8):821-827.
[13] Bell WH, Yamaguchi Y, Poor MR. Treatment of temporomandibular joint dysfunction by intraoral vertical ramus osteotomy[J]. Int J Adult Orthodon Orthognath Surg, 1990,5(1):9-27.
[14] Bell WH, Yamaguchi Y. Condyle position and mobility before and after intraoral vertical ramus osteotomies and neuromuscular rehabilitation[J]. Int J Adult Orthodon Orthognath Surg, 1991,6(2):97-104.
[15] Choi YS, Jung HD, Kim SY, et al. Remodelling pattern of the ramus on submentovertex cephalographs after intraoral vertical ramus osteotomy[J]. Br J Oral Maxillofac Surg, 2013,51(8):259-262.
[16] Jung HD, Jung YS, Park HS. The chronologic prevalence of temporomandibular joint disorders associated with bilateral intraoral vertical ramus osteotomy[J]. J Oral Maxillofac Surg, 2009,67(4):797-803.
[17] Hall HD, Navarro EZ, Gibbs SJ. Prospective study of modified condylotomy for treatment of nonreducing disk displacement[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2000,89(2):147-158.
[18] Hall HD, Navarro EZ, Gibbs SJ. One-and three-year prospective outcome study of modified condylotomy for treatment of reducing disc displacement[J]. J Oral Maxillofac Surg, 2000,58(1):7-17.
[19] Lai W, Yamada K, Hanada K, et al. Postoperative mandibular stability after orthognathic surgery in patients with mandibular protrusion and mandibular deviation[J]. Int J Adult Orthodon Orthognath Surg, 2002,17(1):13-22.
[20] 赵弘宇, 罗永萍, 林 华. 局部浸润麻醉口内切口下面部整形术[J]. 中华医学美学美容杂志, 2005,11(5):70-71.
[21] 王毅敏, Chua CH, 穆雄铮. 隆颏术径路及并发症的比较[J]. 组织工程与重建外科杂志, 2007,3(5):273-274.
[22] Bracaglia R, Tambasco D, Gentileschi S, et al. A simple procedure to facilitate chin implants placement via submental approach[J]. J Plast Surg Hand Surg, 2013,47(3):200-203.
[23] Han K, Kim J. Reduction mandibuloplasty: ostectomy of the lateral cortex around the mandibular angle[J]. J Craniofac Surg, 2001,12(4):314-325.
Experience of treatment of mandibular deformity on 26 cases
HANSi-yuan,HEJia-ni,LENGBing,etal.
(DepartmentofPlasticSurgery,TheFirstAffiliatedHospitalofChinaMedicalUniversity,Shenyang110001,China)
Objective To summarize the experience of treatment of mandibular deformity in recent 5 years in our department to guide the clinical work in the future. Methods The data collected from 26 cases of mandibular deformities were performed retrospective analysis and summarized. Of 26 cases, 12 cases were skeletal class Ⅲ malformation, mandibular protrusion, laterognathism of the mandible, in which 11 cases underwent sagittal split ramus osteotomy and 1 case underwent intraoral vertical ramus osteotomy and 3 of 12 cases underwent genioplasty, 9 cases were prominent mandibular angle, in which 7 cases underwent mandibular angle splitting ostectomy and 2 cases underwent mandibular angle ostectomy; 5 cases were microgenia, in which 3 cases underwent augmentation with Teflon and 2 cases with silicone prosthesis. Results All of the patients were satisfied after operation. The complication rate was 7.69%. Conclusion Sagittal split ramus osteotomy could correct mandibular protrusion and laterognathism by forward or backward movement of the mandible and rotation of the distal fragment. Mandibular angle ostectomy was effective for eversion type of prominent mandibular angle. Mandibular angle splitting ostectomy should be considered in the mandibular angle with outward or backward prominent. Chin augmentation was only suitable for light to moderate microgenia. Genioplasty should be considered in other types.
Sagittal split ramus osteotomy; Mandibular protrusion; Laterognathism; Prominent mandibular angle
韩思源(1963-),男,辽宁沈阳人,副主任医师.
10.3969/j.issn.1673-7040.2015.07.002
R782.2
A
1673-7040(2015)07-0389-04
2015-05-15)