An unusual presentation of acute electrocution
Louay Al-Mouazzen, Emeka Oragui, Karthig Rajakulendran, Nurul AhadSpecialist Registrar Trauma & Orthopaedics, Barking, Havering & Redbridge University Hospitals, Romford, Essex, United KingdomConsultant Trauma & Orthopaedic Surgeon, Barking, Havering & Redbridge University Hospitals, Romford, Essex, United Kingdom
An unusual presentation of acute electrocution
Louay Al-Mouazzen1*, Emeka Oragui1, Karthig Rajakulendran1, Nurul Ahad2
1Specialist Registrar Trauma & Orthopaedics, Barking, Havering & Redbridge University Hospitals, Romford, Essex, United Kingdom
2Consultant Trauma & Orthopaedic Surgeon, Barking, Havering & Redbridge University Hospitals, Romford, Essex, United Kingdom
ARTICLE INFO ABSTRACT
Article history:
Received in 9 February 2015
Received in revised form 10 February 2015 Accepted 11 February 2015
Available online 12 February 2015
Keywords:
Lisfranc injury
Midfoot
Electrocution
Injury to the Lisfranc joint is usually as a result of a direct blow or indirect axial loading of the foot. Lisfranc injuries are associated with significant morbidity and early recognition and treatment is imperative. To date, there has been no description of this injury arising from electrocution. We describ the unusual presentation of a Lisfranc injury in a diabetic patient caused by electrocution of the midfoot. We discuss the surgical management of this case and review the anatomical and pathomechanical considerations of the Lisfranc injury.
Tel: 00447830839398
E-mail: almouazzen@yahoo.com
1. Introduction
Jacques Lisfranc de St Martin (1790-1847) was a pioneering French surgeon and gynaecologist who developed a method of quick amputation through the tarso-metatarsal joint for soldiers suffering from frostbite during the Napoleonic Wars. The term Lisfranc joint became synonymous with the tarso-metatarsal joint and the eponymous name Lisfranc injury, which is used to describe any acute injury across this joint[1]. Prompt recognition of this injury is important as delayed presentation of unstable injuries can result in severe pain, instability and early onset arthritis. Early recognition combined with anatomical reduction and stabilization is associated with improved outcomes. Although Lisfranc injuries are rare, they are more common in the diabetic population, where they can occur following minimal or no trauma[2]. Radiographs will usually reveal the presence of established Charcot changes in the foot[2,3]. Lisfranc injuries may also precipitate Charcot changes in the diabetic patient[4].
To date, there has been no description in the orthopaedic literature of a Lisfranc injury arising from electrocution of the foot. We discuss the unusual presentation of a severe Lisfranc injury caused by electrocution of the midfoot, in a patient with undiagnosed Charcot disease of the foot. We describ the surgical technique used to treat this injury and review the important principles of treating Lisfranc injury.
2. Case report
A 58-year-old lady presented to the Accident and Emergency Department with an acutely painful and swollen right foot. She had received an electric shock to her right midfoot whilst walking over a manhole cover supplied mistakenly by electricity following some road work in the area. She then fell on the ground landing on her right hip, with her right foot twisted underneath her, and went into inversion. The patient was initially assessed by the emergency department clinicians. She was examined thoroughly. Her vital signs were all within the normal limits, her electrocardiogram did not show any changes, and no entry or exit wounds were found. They diagnosed the isolated and minor right foot injury and discharged the patient with analgesia and advice. The patient re-presented two weeks later with persistent right foot symptoms and was unable to bear weight. She had a history of type 2 diabetes mellitus with a mild peripheral sensory neuropathy. She denied any other previous lower limb abnormalities or trauma. Clinical examination showed the right foot to be deformed, tender and swollen. Bilateral radiographs of thefeet showed evidence of a Lisfranc injury in the electrocuted right foot (Figure 1). A computed tomography scan confirmed the diagnosis, revealing a homolateral fracture dislocation in the Lisfranc joint with medial dislocation of the medial cuneiform, and plantar subluxation of the Choparts joint with avulsion fractures of the talar side of the talar-navicular joint, and the cuboid side of the cuboid-cuneiform joint (Figure 2). The resultant foot instability necessitated open reduction and internal fixation to stabilise the joint.

Figure 1. Initial radiographs of the electrocuted right foot. A: Anteroposterior; B: Lateral.
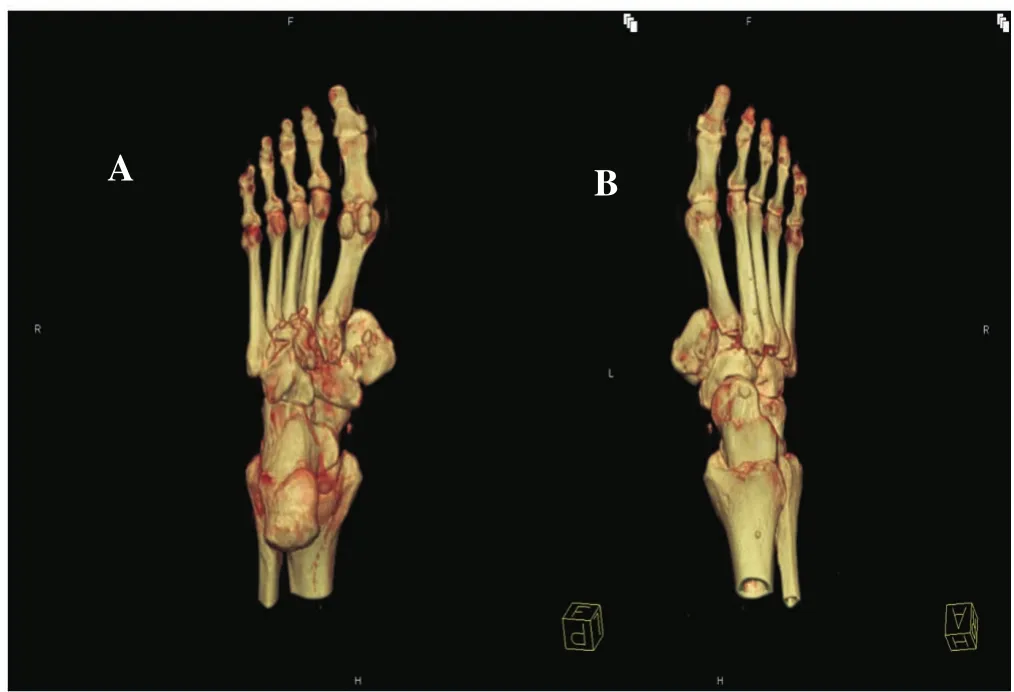
Figure 2. Dorsal and plantar computed tomographic 3D reconstruction slices of the right foot shows the disruption of the medial and the middle columns. A: Plantar; B: Dorsal.
2.1. Surgical technique
With the patient supine, a 6 cm incision was made on the antero-medial border of the 1st ray between the base of the 1st metatarsal and the talo-navicular joint. Deep dissection was performed through subcutaneous tissue and fascia down to bone. The 1st metatarsal was reduced back onto the medial cuneiform and the medial cuneiform onto the navicular. The reduction was held with a contoured dynamic compression plate. The residual subluxation of the talo-navicular joint was comparable to the contralateral side and this was accepted. A 2nd dorsal incision was made between the 2nd and 3rd metatarsal. The inferior extensor retinaculum was divided and the 2nd metatarsal was wedged back between the medial and lateral cuneiforms and held with a 2nd dynamic compression plate. The 3rd metatarsal was reduced onto the lateral cuneiform and held with a semi-tubular plate (Figure 3). Cartilage was removed at the medial cuneiform-1st metatarsal joint and bone graft introduced. The wounds were closed in layers and the patient was immobilised in a non-weight bearing cast for 8 weeks.

Figure 3. Intra-operative images of the plate fixation. A: Anteroposterior; B: Lateral.
3. Discussion
3.1. Functional anatomy and pathomechanics of the Lisfranc joint
The arches of the foot help to convert from a rigid lever to a sprung platform, thereby producing a more energyefficient gait. The transverse and longitudinal arches of the foot are formed by the tarsal and metatarsal bones. Stability of the midfoot is provided by the Roman arch configuration of the bones and their strong ligamentous attachments. Proximal intermetatarsal lig-aments connect the 2nd to 5th metatarsals, but they are absent between the 1st and 2nd metatarsal. The Lisfranc ligament complex is composed of a dorsal, interosseous and plantar ligamentous structures that connect the medial cuneiform to the 2nd metatarsal and represents the only significant attachment between the 1st and 2nd ray at the midfoot level. The interosseous ligament is the strongest of the three and is referred to as the Lisfranc ligament[5]. Disruption of the Lisfranc joint arises from direct or indirect loading. Direct trauma is usually crush injuries and may have significant associated soft tissue injuries. Indirect loading is usually due to axial loading of a plantarflexed, abducted or adducted foot[2].
Lisfranc injuries can be classified using the Myerson classification for displaced injuries[6], or the Nunley and Vertullo classification for subtle diastasis[7].
3.2. Surgical fixation of Lisfranc injuries
In Lisfranc injuries in an otherwise normal foot, the decision to treat is based on both physical examination and radiographic studies. Conceptually, unstable tarso-metatarsal injuries that lead to a loss of the arch or significant deformity, have a high risk of secondary pain and disability which should be treated surgically. Instability is suggested in anteroposterior radiographs by the presence of a gap greater than 2 mm between the 2nd metatarsal and medial cuneiform or the 1st and 2nd metatarsal. On lateral radiographs, plantar-dorsal displacement of greater than 1 mm or any dorso-plantar displacement on lateral radiographs is suggestive of instability[8]. Computed tomography scans can be used to assess subtle fractures and help with pre-operative planning. Magnetic resonance imaging provides a superior assessment of the integrity of the Lisfranc ligament[9].
Closed reduction and percutaneous pinning is suitable for injuries with greater than 2 mm of displacement but less than 15°of talo-metatarsal angulation. Open reduction is required for displacement of greater than 2 mm and 15°of talo-metatarsal angulation[8]. The principles of treatment involve stabilising or debriding osteochondral defects, reducing medial joints and stabilising the rays from medial to lateral. Stabilisation involves any combination of screws, plates and K-wires. Open fractures are usually treated with external fixators[1-10].
There is still debate about the role of arthrodesis in the primary treatment of acute Lisfranc injuries. In a prospective controlled trial, Henning et al.[11] concluded that partial arthrodesis of tarso-metatarsal joint injuries resulted in a significant reduction in the rate of follow-up surgical procedures if hardware removal was routinely performed with no significant difference in physical function. In another prospective study, Mulier et al.[12] recommended that open reduction and internal fixation with screws or partial arthrodesis are the choices of treatment in severe tarsometatarsal fracture dislocations with primary complete arthrodesis to be reserved as a salvage procedure.
Diabetic patients have an increased risk of Lisfranc injuries due to the loss of the neuroprotective sensory mechanisms of the foot, attenuation of ligaments due to calcification and poor healing of previous injuries, and the increased likelihood of repeated unperceived microtrauma similar to the neurotraumatic theory of Charcot pathogenesis[13].
Therefore, clinicians should maintain a high index of suspicion when assessing patients with diabetic peripheral neuropathy who present with acute midfoot pain following injury.
Until now, there has been no report in the literature of Lisfranc injury caused by an electrical shock. Our patient had a clear history of acute pain and deformity following an electrical injury. Prior to the index incident, they reported that the foot which had a normal morphological appearance, was pain free and they walked with a normal gait. The principles of Lisfranc injury management in a normal foot are identification of the injury and reduction and fixation of unstable joints to reduce the risk of secondary debilitation. However, the management of acute Lisfranc injuries in a Charcot foot have not been clearly defined. Some authors have suggested the use of a total contact cast[4], but at present, there is no high-level evidence available.
In this case, we opted for surgical management on the basis that despite the patient being diabetic and having an undiagnosed Charcot foot, prior to the index accident, she had been mobilizing freely without any impediment. Nonoperative management would have left the patient with a grossly deformed foot and risked the rapid development of end stage Charcot changes.
Conflict of interest statement
The authors report no conflict of interest.
References
[1] Khan W, Oragui E, Akagha A. Common fractures and injuries of the ankle and foot: functional anatomy, imaging, classification and management. J Perioper Pract 2010; 20(7): 249-258
[2] Desmond EA, Chou LB. Current concepts review: Lisfranc injuries. Foot Ankle Int 2006; 27: 653-660.
[3] Jerome JTJ. Divergent Lisfranc’s dislocation and fracture in the Charcot foot: a case report. Foot Ankle J 2008; doi: 10.3827/ faoj.2008.0106.0003.
[4] Vasquez V, Henderson S. Charcot foot? Charcot arthropathy caused by Lisfranc fracture-dislocation in a diabetic. West J Emerg Med 2010; 11(2): 146-147.
[5] Esway JE, Boyer M, Shereff M, Wukich DK. Lisfranc injuries: what have we learned since Napoleon’s era? Oper Tech Orthop 2006; 16(1): 60-67.
[6] Myerson MS. The diagnosis and treatment of injury to the tarsometatarsal joint complex. J Bone Joint Surg Br 1999; 81: 756-763
[7] Nunley J, Vertullo C. Lisfranc injuries in the athlete. Am J Sports Med 2002; 30: 871-878.
[8] Kuo RS, Tejwani NC, Digiovanni CW, Holt SK, Benirschke SK, Hansen ST Jr, et al. Outcome after open reduction and internal fixation of Lisfranc joint injuries. J Bone Joint Surg Am 2000; 82(11):1609-1618.
[9] Gupta RT, Wadhwa RP, Learch TJ, Herwick SM. Lisfranc injury: imaging findings for this important but often-missed diagnosis. Curr Probl Diagn Radiol 2008; 37: 115-126.
[10] Zgonis T, Roukis TS, Polyzois VD. Lisfranc fracturedislocations: current treatment and new surgical approaches. Clin Podiatr Med Surg 2006; 23: 303-322.
[11] Henning JA, Jones CB, Sietsema DL, Bohay DR, Anderson JG. Open reduction internal fixation versus primary arthrodesis for Lisfranc injuries: a prospective randomized study. Foot Ankle Int 2009; 30: 913-922.
[12] Mulier T, Reynders P, Dereymaeker G, Broos P. Severe Lisfrancs injuries: primary arthrodesis or ORIF? Foot Ankle Int 2002; 23: 902-905.
[13] Frykberg RG, Mendeszoon E. Management of the diabetic Charot foot. Diabetes Metab Res Rev 2000;16(Suppl 1): S59-S65.
doi:Document heading
*Corresponding author:Louay Al-Mouazzen, Specialist Registrar Trauma & Orthopaedics, Barking, Havering & Redbridge University Hospitals, Romford, Essex, United Kingdom.
 Journal of Acute Disease2015年2期
Journal of Acute Disease2015年2期
- Journal of Acute Disease的其它文章
- Cough-induced intercostal lung herniation
- A report of acute atrial fibrillation induced by misapplication of epinephrine
- Clinical manifestation as acute coronary syndrome without electrocardiographically ischemia: a clue for aortic dissection
- Report of a child with acute herpes zoster ophthalmicus induced partial third nerve palsy
- Report of a pregnant lady with bilateral elbow dislocation caused by acute fall injury
- A retrospective study of acute pertussis in Hasan Sadikin Hospital-Indonesia
