A report of acute atrial fibrillation induced by misapplication of epinephrine
Yu-Jang SuDepartment of Emergency Medicine, Mackay Memorial Hospital, Taipei 0449, TaiwanDepartment of Oral Hygiene, College of Oral Medicine, Taipei Medical University, Taipei, Taiwan
A report of acute atrial fibrillation induced by misapplication of epinephrine
Yu-Jang Su
1Department of Emergency Medicine, Mackay Memorial Hospital, Taipei 10449, Taiwan
2Department of Oral Hygiene, College of Oral Medicine, Taipei Medical University, Taipei, Taiwan
ARTICLE INFO ABSTRACT
Article history:
Received 27 January 2015
Received in revised form 1 February 2015 Accepted 5 February 2015
Available online 11 February 2015
Keywords:
Atrial fibrillation
Cardiac ischemia
Labetalol
Epinephrine
如果进一步把特色小镇建设分为低、中、高三种情况,三种情况下轻、重资产型特色小镇每平方公里社会投入分别对应为8亿元、16亿元、24亿元和16亿元、32亿元、48亿元,三种情况下资金需求总量如表2所示。从预测结果可以看出,只有低情况和资金均衡下,才最为接近《广西培育特色小镇意见》计划的2000亿元固定资产投入。同时考虑到广西农业发展和旅游业的天然优势,未来广西特色小镇建设轻、重资产类型数量比为21较为合理,符合广西经济社会发展实际。
Urticaria
Urticaria is a systemic allergic reaction leading to wheal formation with skin itching. Occasionally we come across some intractable cases, in which we may administrate epinephrine infusion besides steroid and anti-histamine. A 19 year-old man suffered from intractable urticaria for 2 days, although anti-histamine and steroids were used. Titration of adrenaline was considered in the treatment of intractable urticaria. He was administrated 1 mg epinephrine intravenous bolus due to mis-dilution by the nurse. Transient atrial fibrillation with cardiac ischemia occurred. After 12.5 mg labetalol i.v., and 11-hour observation in the emergency room, he gradually recovered to normal sinus rhythm without ST-T change. In the past, ventricular tachycardia, hypertension, chest pain, pulmonary edema, the need to intubate, renal failure requiring renal transplant, coronary artery spasm, myocardial ischemia/infarction and hypokalemia have been reported after mis-diluted or excessive doses of epinephrine in treating anaphylaxis. To our knowledge, our case is the first worldwide to describe transient atrial fibrillation after epinephrine overdose, and the patient was successfully resuscitated by 12.5 mg labetalol. It is important to know how to rescue accidental epinephrine intravenous injection patients.
Tel: 886-2-25433535 ext. 3126
E-mail: yjsu@ms1.mmh.org.tw1,2*
1. Introduction
Anaphylaxis is a commonly seen problem in the emergency department (ED). The onset and clinical course are variable. Often, the patient is initially seen with erythematous and pruritis wheal formation that progresses to urticaria and angioedema. Other non-specific symptoms such as dizziness, nausea, vomiting, and diarrhea may also be found. For severe anaphylactic reactions with lifethreatening conditions such as upper airway obstruction related hoarseness, dysphonia, or difficulty swallowing and lower airway obstruction related wheezing and chest tightness possibly occurred. In the treatment of anaphylaxis, epinephrine is often underused due to variably adverse effects (cardiac arrhythmia, cardiac ischemia, coronary artery spasm) whereas antihistamines and corticosteroids are often relied on as first line agents. Here we present a case of transient atrial fibrillation (AF) with cardiac ischemia after mis-dilution by the nurse using epinephrine in treating intractable urticaria. He was successfully resuscitated with 12.5 mg labetalol intravenous (i.v.) bolus, and the electrocardiogram (ECG) rhythm returned to normal sinus rhythm. He recovered after an 11-hour ED observation.
2. Case report
A 19-year-old man suffered from skin itching andskin rashes that were noted for two days. He went to the ED for help yesterday, but the symptoms flared up again this morning. On arrival to our ED, he had no shortness of breath. He received an intramuscular injection of diphenylhydramine 30 mg, and 4 mg i.v. betamethasone yesterday, but the rashes reappeared. Oral medications with 60 mg fexofenadine twice daily and 5 mg prednisolone four times a day were also prescribed to him. Owing to the sustained skin rashes, 30 mg diphenylhydramine i.v. every six hours, 40 mg methylprednisolone i.v. every six hours, and 10 mg chlorpheniramine were administrated. Prescription of 1 mg epinephrine in 500 mL normal saline i.v. infusion every 30 mL per hour was applied to treat the intractable urticaria. The nurse mis-applied the epinephrine as 1 mg i.v. push, and then the young man screamed. He was experiencing sudden chest pain with palpitations. Pallor in his extremities and face were also found. At that time, the systolic blood pressure was taken as 166 mmHg, and the heartbeat was 126 per minute. Electrocardiogram (ECG) (Figure 1) showed atrial fibrillation with rapid ventricular response, and depressed ST segment indicating cardiac ischemic change over the leads V4, 5, 6. We monitored (ECG, blood pressure, pulse-oxymeter) him closely and gave 12.5 mg labetalol i.v., and then he gradually relaxed. Blood tests were within the normal limits except the troponin-I level (1.00 ng/mL, normal <1.0). After 11 hours of observation, he was discharged with remission of rashes, no more chest pain, and stable vital signs (blood pressure=102/63; heartbeat 83 per minute).
3. Discussion
Anaphylaxis is the reaction from the invasion of an antigen into the body which initializes a hypersensitive reaction typically medicated by immunoglobin E (IgE) Symptoms of anaphylaxis ranged variably from itching skin to death. When anaphylactic patients have lifethreatening conditions such as upper airway obstruction related hoarseness, dysphonia, or difficulty swallowing and lower airway obstruction related wheezing, chest tightness, and shock, epinephrine should be given[1]. The initial adult dose ranges from 0.3 mL to 0.5 mL of a 1:1 000 dilution (0.3 to 0.5 mg) subcutaneously or intramuscularly[2]. The dose of epinephrine can be repeated every 10 to 15 minutes as necessary up to a maximum of 1 mL (1 mg) dose.
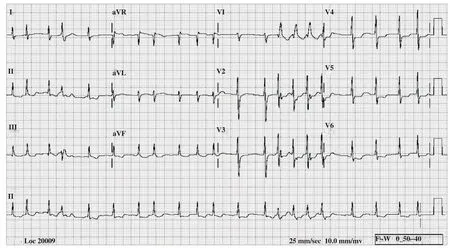
Figure-1: Atrial fibrillation with rapid ventricular response and depressed ST segment indicating cardiac ischemic change over the leads V4, 5, 6 were noted after 1 mg of epinephrine IV bolus.
There are some articles that have mentioned inappropriate administration of epinephrine related complications in treating anaphylaxis such as ventricular tachycardia, hypertension, chest pain, pulmonary edema, the need to intubate with ICU admission, renal failure requiring renal transplant, myocardial ischemia or infarction and hypokalemia[3-5]. To our knowledge, our case is the first one in the world describing AF after epinephrine overdose in treating urticaria, although it happened due to misdilution by the nurse in charge.
AF is the most commonly encountered arrhythmia in clinical practice resulting from the absence of coordinated atrial systole. Multiple reentrant electrical wavelets that move randomly around the atria lead to AF. When the ventricular rate exceeds 100 per minute, a situation of AF with rapid ventricular response occurs and could lead to decompensation in the form of either myocardial ischemia or leading to congestive heart failure (CHF). Risk factors for AF include age, male sex, long-standing hypertension, valvular heart disease (VHD), left ventricular hypertrophy (LVH), coronary artery disease (CAD), diabetes mellitus, smoking, and any form of myocarditis. In children, AF is not commonly seen except after cardiac surgery[6]. In our case, epinephrine triggers multiple reentrant electrical wavelets and moves randomly around the atria leading to AF.
In the treatment of urticaria, the dose of diphenhydramine is 1 to 2 mg/kg or 25 to 50 mg/dose, which should optimally be given parenterally to counteract histamine induced vasodilation. Corticosteroids have many theoretical benefits including prevention or shortening the duration of protracted reactions, particularly those associated with bronchospasm. Steroids may take up to 4 or 6 hours to take full effect. If the antihistamines and steroids, and initial i.v. epinephrine dose do not work to treat urticaria, the epinephrine infusion should initially be titrated with a rate at 1 μg/min, which can be increased to 2 to 10 μg/ min[4]. Electrocardiographic monitoring is mandatory if epinephrine is given intravenously. After all, these adverse outcomes may be more likely to occur when the i.v. epinephrine has been given too rapidly, inadequately diluted, or in excessive doses[2]. Before injection of epinephrine, the nurse should check the physician’s instructions and follow them prudently.
4. Conclusion
In conclusion, as discussed previously, epinephrine, along with stabilizing measures, such as oxygen and fluids, are well assumed as first line treatments in anaphylaxis. Epinephrine route, dose, and concentration should be determined according to the status of the patient. Steroids, antihistamines, and H2 blockers can be considered as second line treatments. An intra-muscular dose of epinephrine is generally recommended to administrate initially. If additional epinephrine is required, a controlled intravenous infusion might be safer than intravenous bolus administration[7]. Before administration of epinephrine, the nurse should check the physician’s instructions and follow them prudently, and prepare ECG monitoring for the patient. It is important to know how to rescue accidental epinephrine intravenous injection patients.
Conflict of interest statement
The authors report no conflict of interest.
References
[1] Pongracic JA, Kim JS. Update on epinephrine for the treatment of anaphylaxis. Curr Opin Pediatr 2007; 19(1): 94-98.
[2] McLean-Tooke AP, Bethune CA, Fay AC, Spickett GP. Adrenaline in the treatment of anaphylaxis: what is the evidence? BMJ 2003; 327(7427): 1332-1325.
[3] Shaver KJ, Adams C, Weiss SJ. Acute myocardial infarction after administration of low-dose intravenous epinephrine for anaphylaxis. CJEM 2006; 8(4): 289-294.
[4] Anchor J, Settipane RA. Appropriate use of epinephrine in anaphylaxis. Am J Emerg Med 2004; 22(6): 488-490.
[5] Karch SB. Coronary artery spasm induced by intravenous epinephrine overdose. Am J Emerg Med 1989; 7(5): 485-488.
[6] Savelieva I, Camm J. Update on atrial fibrillation: part I. Clin Cardiol 2008; 31(2): 55-62.
[7] Brown SG. Anaphylaxis: clinical concepts and research priorities. Emerg Med Australas 2006; 18(2): 155-169.
doi:Document heading
*Corresponding author:Yu-Jang Su, M.D. M.D. Department of Emergency Medicine, Mackay Memorial Medical Center, No. 92, Sec. 2, Chung-Shan N. Road, Taipei, Taiwan.
 Journal of Acute Disease2015年2期
Journal of Acute Disease2015年2期
- Journal of Acute Disease的其它文章
- Cough-induced intercostal lung herniation
- Clinical manifestation as acute coronary syndrome without electrocardiographically ischemia: a clue for aortic dissection
- Report of a child with acute herpes zoster ophthalmicus induced partial third nerve palsy
- Report of a pregnant lady with bilateral elbow dislocation caused by acute fall injury
- An unusual presentation of acute electrocution
- A retrospective study of acute pertussis in Hasan Sadikin Hospital-Indonesia
