微创单髁置换术治疗膝关节单间室骨性关节炎
凌 晶 章军辉 狄正林 何志勇 曾智敏 徐荣明
(宁波市第六医院关节外科,宁波 315040)
·临床论著·
微创单髁置换术治疗膝关节单间室骨性关节炎
凌 晶 章军辉 狄正林 何志勇 曾智敏 徐荣明
(宁波市第六医院关节外科,宁波 315040)
目的探讨微创单髁置换术治疗膝关节单间室骨性关节炎的临床疗效。方法2011年10月~2013年3月,对51例(54膝)膝关节内侧间室骨性关节炎采用髓外定位法进行胫骨及股骨截骨,骨水泥固定Oxford Ⅲ单髁置换假体并植入移动半月板。观察切口长度,手术时间,手术前后血红蛋白下降量,术后直腿抬高时间,膝关节活动范围,术后髋膝踝角及并发症;采用Oxford评分法对术前、术后膝关节功能进行评估。结果2例出现内衬脱位并发症进行翻修。无感染、下肢深静脉血栓、假体位置不良,假体松动等并发症。切口长度(6.6±0.8)cm(5.5~8 cm)。手术时间(59.9±6.6)min(50~80 min),术后3 d血红蛋白下降(13.5±5.0)g/L(7~28 g/L)。术后自主直腿抬高时间(3.4±1.6)d(1~8 d)。术后2~3 d行双下肢全长片检查,髋膝踝178.2°±2.6°(177°~183°)。术后无伸直受限,最大屈曲度121.3°±6.6°(110°~130°)。51例术后随访6~23个月,平均14.5月,无感染、下肢深静脉血栓、假体位置不良,假体松动等并发症。Oxford膝关节功能评分术前(24.6±1.9)分,术后末次随访(41.6±3.5)分,术前后比较有统计学差异(t=34.313,P=0.000)。结论微创单髁置换术治疗内侧间室骨性关节炎短期效果良好,中远期疗效需要进一步随访。
关节成形术; 置换; 膝关节; 骨关节炎
单髁置换术治疗膝关节内侧间室骨性关节炎临床应用超过30年,具有创伤小、出血少、恢复快、活动度大等优点。随着对膝关节病变理解的加深以及假体设计的不断进步,微创单髁置换手术取得了满意的临床疗效。2011年10月~2013年3月我们采用微创单髁系统治疗膝关节内侧间室骨性关节炎51例,现报道如下。
1 临床资料与方法
1.1 一般资料
本组51例(54膝),男19例,女32例。年龄46~80岁,平均65.4岁。主要症状为膝关节行走疼痛,行走跛行,疼痛以膝关节内侧明显。右膝23例,左膝28例,其中双膝3例。病程3~27个月,平均8.6月。X线、MRI等影像学诊断证实为膝关节退行性改变,符合膝关节内侧间室骨性关节炎诊断。
病例选择标准:①前内侧间室骨性关节炎,Ahlback X线分级Ⅰ~Ⅲ期;②可复性关节内内翻畸形;③活动度屈曲>100°;④屈曲挛缩<15°;⑤前交叉韧带功能完好;⑥外侧间室软骨完好。排除炎性关节病及风湿性关节炎。
1.2 方法
均选用单髁假体(Oxford Phase Ⅲ,美国Biomet公司)。腰麻联合硬膜外麻醉。平卧位,止血带充气。取髌骨上缘至胫骨结节内侧纵行切口,显露内侧间室,清理胫骨平台及股骨内侧髁内侧缘骨赘,清理髁间窝骨赘,显露内侧间室骨性结构。检查前交叉韧带完整性。膝关节屈曲90°,髓外定位法固定胫骨导向器,往复锯紧贴股骨内侧髁外侧缘,位于前交叉韧带止点内侧,指向股骨头中心进行胫骨平台垂直截骨,紧贴截骨板完成胫骨平台截骨。保持膝关节屈曲90°,标记股骨内侧髁冠状位中线,放置胫骨底板与间隔器,插入股骨钻孔导向器,髓外定位杆指向股骨头中心,导向器手柄平行于胫骨长轴,调整膝关节屈曲角度,使导向器在矢状面上与股骨长轴平行,导向孔位于股骨内侧髁中线,完成股骨髁钻孔。放置截骨模板完成股骨后髁截骨,测量膝关节屈曲间隙,根据屈曲间隙进行股骨远端截骨,调整屈伸间隙平衡,达到屈曲90°与屈曲20°时间隙平衡,根据操作步骤完成后髁骨赘清理,试模,安装假体,膝关节保持屈曲45°,待骨水泥凝固,清理骨水泥,常规关闭切口。
术后24 h拔除引流管,术后第2天助行器辅助下床行走,自主屈伸活动度锻炼。术后使用抗生素48 h,术后1~3 d行血常规检查。术后足底泵及低分子肝素预防下肢深静脉血栓,出院后口服利伐沙班抗凝,药物抗凝时间术后共14 d。术后拍膝关节正侧位片及双下肢全长片,分别于术后4周,3、6个月,1年随访,行患膝正侧位X线片检查及Oxford膝关节功能评分。
1.3 观察指标
手术时间,术后72 h血红蛋白下降量,术后直腿抬高时间,膝关节活动范围,采用Oxford膝关节功能评分法对术前、术后膝关节功能进行评估。
2 结果
手术时间(59.7±6.6)min(50~80 min),术后3 d血红蛋白下降(13.5±5.0)g/L(7~28 g/L)。术后自主直腿抬高时间(3.4±1.6)d(1~8 d),手术切口长(6.6±0.8)cm(5.5~8 cm)。术后2~3 d行双下肢全长片检查,髋膝踝角178.2°±2.6°(177°~183°)。术后所有患者均无伸直受限,最大屈曲度121.3°±6.6°(110°~130°)。典型病例见图1。51例术后随访6~23个月,平均14.5月,无感染、下肢深静脉血栓、假体位置不良、假体松动等并发症。2例出现内衬脱位(1例发生在术后4个月,1例为术后8个月),再次入院行手术探查,术中清理残余后髁骨赘及骨水泥,更换半月板垫片,至末次随访,均未再次脱位,膝关节功能良好。术前与术后末次随访膝关节Oxford膝关节功能评分和膝关节活动度的比较见表1。

图1 A. 男,67岁,术前X线片提示双侧膝关节内侧间室骨性关节炎 B.行左膝微创单髁置换术,术后X线片提示假体位置良好 C.术后双下肢立位全长片提示下肢力线纠正,髋膝踝角179° D.术后4 d膝关节主动屈曲角度 E.术后4 d可自主直腿抬高,提示股四头肌肌力恢复良好

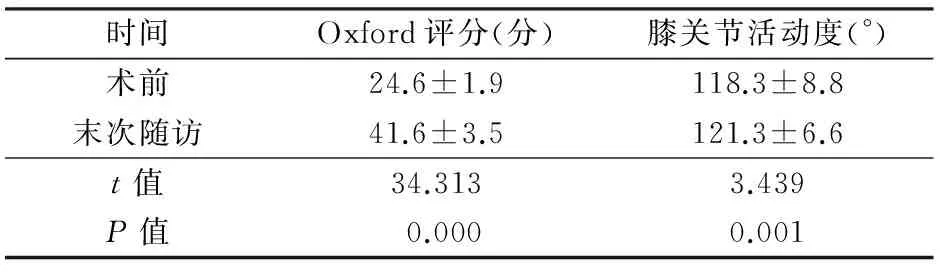
时间Oxford评分(分)膝关节活动度(°)术前24.6±1.9118.3±8.8末次随访41.6±3.5121.3±6.6t值34.3133.439P值0.0000.001
3 讨论
膝关节骨性关节炎是困扰中老年患者常见疾病。文献[1]报道接受人工膝关节置换手术患者中,25%~36%患者为单髁置换适应证。单髁置换术治疗膝关节内侧间室关节炎取得了满意的临床疗效,中远期假体生存率满意[2~4],15年假体生存率93%[5]。
对于内侧间室骨性关节炎,通常的治疗选择有全膝置换术、单髁置换术、胫骨高位截骨术。相对于全膝而言,单髁置换术保留了前后交叉韧带,截骨量少,与正常膝关节生物力学更接近[6],手术创伤小,术后并发症少,关节功能恢复快,本体感觉如关节活动觉较好[7]。传统全膝置换术与单髁置换术对比研究结果显示,单髁置换术侧术后效果优于全膝置换术侧[8]。与胫骨高位截骨术相比,Spahn等[9]荟萃分析认为单髁置换术与胫骨高位截骨2种术式术后12年生存率相仿。Weale等[10]报道术后17年胫骨高位截骨生存率65%,单髁置换术后17年生存率88%。胫骨高位截骨术创伤较大,术后无法早期负重,术后翻修手术较单髁置换困难,且围手术期并发症几率更高。
传统单髁置换手术采用膝正中切口,向外脱位髌骨,创伤较大。微创单髁系统仅需暴露膝关节内侧间室,不脱位髌骨,切口较全膝置换手术明显减少,同时使用移动窗口技术,避免皮下切口延长,不干扰股四头肌,手术创伤较小,术后疼痛较轻,术后股四头肌肌力恢复快,本组术后直腿抬高时间平均3.4 d(1~8 d)。
传统观点将髌股间室退变作为单髁置换手术禁忌证,但Beard等[11]对术前存在髌股关节软骨缺损的患者随访结果显示,术前存在的髌股关节退变对单髁置换术后膝关节功能及假体生存率无影响,在对Oxford评分中远期随访中,无一例因髌股关节问题而进行翻修。对于外侧间室及髌股间室存在退变的患者,Emerson等[12]随访结果显示对一些低活动量要求的患者,即使存在三间室的骨性关节炎,单髁置换仍可以获得满意的效果。本组髌股关节退变、年龄、体重指数不作为手术禁忌证。
术中操作时需要时刻警惕保护内侧副韧带,内侧副韧带损伤通常发生在胫骨截骨及清理骨赘过程中,如进行内侧副韧带松解会导致过度纠正力线,影响手术效果[13],并导致聚乙烯内衬脱位[14]。股骨髁截骨是手术的关键点,在Oxford Phase Ⅲ操作手册中,推荐使用髓内定位方法,但由于髓内开口位置不同患者存在较大变异、术中可能存在髌骨遮挡、髓内杆过细晃动等原因,髓内定位方法存在误差几率。我们使用髓外定位方法进行股骨髁远端截骨,术中采用多种方法进行效验。本组术后髋膝踝角度平均为178.2°(177°~183°),证实髓外定位法具有良好准确率与可重复性。由于避免股骨开髓,有助于减少围手术期出血,本组术后72 h血红蛋白下降(13.5±5.0)g/L,无一例需要输血。
Oxford单髁系统使用移动半月板平台,该设计可以更好地恢复下肢生物力学,增大股骨髁假体与半月板接触面积,降低局部应力,减少聚乙烯磨损[15]。与固定平台设计比较,聚乙烯垫片脱位为其特有并发症,本组2例出现聚乙烯垫片脱位,并进行翻修手术,1例术中发现股骨后髁骨赘与移动半月板发生撞击,1例术中发现内侧副韧带延长导致内侧松弛,并有骨水泥残留,清理骨水泥后增加2 mm厚度聚乙烯内衬,由于下肢力线仍保持良好,未翻修全膝。2例术后随访未再次发生脱位,膝关节功能良好。聚乙烯内衬脱位与残余股骨后髁骨赘、骨水泥发生撞击、内侧韧带松解、屈伸间隙不稳等因素有关。我们认为术中保护内侧副韧带,清理后髁骨赘及残余骨水泥,平衡屈伸间隙,避免假体位置不良是避免内衬脱位的关键。
综上,微创单髁置换术治疗膝关节内侧间室骨性关节炎效果短期效果良好,中远期疗效需要进一步随访。
1 Willis-Owen CA, Brust K, Alsop H, et al. Unicondylar knee arthroplasty in the UK National Health Service: An analysis of candidacy, outcome and cost efficacy. Knee,2009,16(6):473-478.
2 Borus T, Thornhill T. Unicompartmental knee arthroplasty. J Am Acad Orthop Surg,2008,16(1):9-18.
3 Faour-Martín O, Valverde-García JA, Martín-Ferrero MA, et al. Oxford phase 3 unicondylar knee arthroplasty through a minimally invasive approach: long-term results. Int Orthop,2013,37(5):833-838.
4 Kristensen PW, Holm HA, Varnum C, et al. Up to 10-year follow-up of the oxford medial partial knee arthroplasty-695 cases from a single institution. J Arthroplasty,2013,28(9 Suppl):S195-S198.
5 Foran JR, Brown NM, Della Valle CJ, et al. Long-term survivorship and failure modes of unicompartmental knee arthroplasty. Clin Orthop Relat Res,2013,471(1):102-108.
6 Hopkins AR, New AM, Rodriguez-y-Baena F, et al. Finite element analysis of unicompartmental knee arthroplasty. Med Eng Phys,2010,32(1):14-21.
7 Isaac SM,Barker KL,Danial IN,et a1.Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompamnental arthroplasty.Knee,2007,14(3):212-217.
8 徐建平,徐卫东,林国兵,等.双膝骨关节炎患者行小切口单髁置换术与全膝关节置换术临床疗效对比分析.中华外科杂志,2013,51(2):157-160.
9 Spahn G,Hofmann GO,von Engelhardt LV,et al. The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc,2013,21(1):96-112.
10 Weale AE, Newman JH. Unicompartmental arthroplasty and high tibial osteotomy for osteoarthrosis of the knee. A comparative study with a 12- to 17-year follow-up period. Clin Orthop Relat Res,1994,(302):134-137.
11 Beard DJ, Pandit H, Gill HS, et al. The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Joint Surg(Br),2007,89(12):1597-1601.
12 Emerson RH Jr, Hansborough T, Reitman RD, et al. Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res,2002,(404):62-70.
13 Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br,1998,80(6):983-989.
14 Shakespeare D, Waite J.The Oxford medial partial knee replacement. The rationale for a femur first technique. Knee,2012,19(6):927-932.
15 Apostolopoulos AP, Michos IV, Mavrogenis AF, et al. Fixed versus mobile bearing knee arthroplasty: a review of kinematics and results. J Long Term Eff Med Implants,2011,21(3):197-203.
(修回日期:2013-11-25)
(责任编辑:李贺琼)
MinimallyInvasiveUnicompartmentKneeArthroplastyforUnicompartmentKneeOsteoarthritis
LingJing,ZhangJunhui,DiZhenglin,etal.
DepartmentofJointSurgery,NingboNo. 6thHospital,Ningbo315040,China
ObjectiveTo explore the clinical efficacy of minimally invasive unicompartment knee arthroplasty(MI-UKA) for unicompartment knee osteoarthritis.MethodsFrom October 2011 to March 2013,51 patients (54 knees) with unicompartment knee osteoarthritis were treated with MI-UKA. Tibia and femur osteotomy were performed via extramedullary alignment guidance, and then meniscal-bearing unicompartment prosthesis (Oxford Phase Ⅲ) was fixed with bone cement. Incision length,operative time, decreased hemoglobin values before and after surgery, time to straight leg raise, range of motion, postoperative hip-knee-ankle angle and complications were observed. The function results were assessed preoperatively and postoperatively by Oxford scores.ResultsTwo patients underwent revision surgery due to bearing dislocation. The mean incision length was (6.6±0.8) cm(range, 5.5-8 cm); the mean operative time was (59.9±6.6) min(range, 50-80 min); the mean decreased hemoglobin values was (13.5±5.0) g/L(range, 7-28 g/L) 72 h postoperatively; the mean time to straight leg raise was (3.4±1.6) d(range, 1-8 d) after the surgery; and the mean postoperative hip-knee-ankle angle measured by lower limbs X-ray was 178.2°±2.6° (range, 177°-183°). The range of motion of knee reached a mean of 121.3° (range, 110°-130°). There was a statistical difference in Oxford scores between before and after the surgery [(24.6±1.9) points vs. (41.6±3.5) points,t=34.313,P=0.000]. Fifty-one cases were followed up for 6 to 23 months (mean, 14.5 months), and no infection, deep venous thrombosis or prosthesis mal-position and loosening were observed.ConclusionMinimally invasive unicompartment knee arthroplasty is an effective alternative for the treatment of unicompartment knee osteoarthritis, however, mid- and long-term studies are still required.
Arthroplasty; Replacement; Knee joint; Osteoarthritis
R687.4+2
:A
:1009-6604(2014)03-0243-03
10.3969/j.issn.1009-6604.2014.03.015
2013-08-26)