3D OCT检测黄斑区视网膜厚度在青光眼诊断中的价值
庞燕华 赵桂玲 柯毅 谭志 朱敏怡 李瑞庄
3D OCT检测黄斑区视网膜厚度在青光眼诊断中的价值
庞燕华 赵桂玲 柯毅 谭志 朱敏怡 李瑞庄
光学相干断层扫描;黄斑;视网膜厚度;青光眼
目的应用3D光学相干断层扫描(optical coherence tomography,OCT)检测青光眼患者黄斑区视网膜厚度,并与正常人眼黄斑区视网膜厚度进行比较,以探讨其在青光眼诊断中的价值。方法选取2012年9月至2013年6月于我院就诊的青光眼患者40例(46眼)为青光眼组,另选取于我院同期健康体检的正常人50例(50眼)作为对照组,应用Topcon 3D OCT进行黄斑区视网膜厚度检测,观察正常人和青光眼患者黄斑地形图的图像特征,并分析青光眼黄斑区视网膜平均厚度与视野平均缺损值的相关性。结果对照组及青光眼组黄斑视网膜厚度地形图均表现为黄斑中心凹最薄,对照组黄斑区内环视网膜较外环厚,青光眼组内环及外环视网膜局限性或弥漫变薄。青光眼组与对照组黄斑中心凹1 mm内及黄斑中心凹视网膜厚度比较,差异均无统计学意义(t=1.39、1.64,P=0.17、0.10);青光眼组内环、外环各象限视网膜厚度、黄斑区视网膜体积及视网膜厚度均较对照组变薄或变小,差异均有统计学意义(均为P<0.05)。青光眼患者黄斑区视网膜厚度与视野缺损值呈负相关(r=-0.612,P=0.01)。结论黄斑区视网膜OCT检测将有可能是青光眼诊断、追踪的重要手段之一。
[眼科新进展,2014,34(5):468-470]
青光眼是一种临床常见的眼科疾病,以视网膜神经节细胞(retinal ganglion cells,RGC) 进行性丢失、视网膜神经纤维层(retinal nerve fiber layer,RNFL)变薄及视野缺失为其主要病理特征。临床上常常检测视盘参数及视盘旁RNFL厚度以评估青光眼病情的进展,但即使在正常人群,视盘参数也存在相当大的变异,而且视盘表面的大血管极易干扰RNFL厚度的检测,这些都为青光眼诊断和预后判断增加了难度。相对视盘而言,黄斑区则是比较简单的解剖区域,且缺乏大血管。在正常个体,约50%的RGC位于以黄斑中心凹为中心的20°范围内[1]。Zeimer等[2]早在1998年提出利用后极部视网膜地形图来检测青光眼性眼底损伤,为早期诊断青光眼提供依据。近年来,Nakatani 等[3]认为在早期青光眼的诊断上,黄斑区的参数和RNFL厚度一样具有很高的诊断价值。光学相干断层扫描(optical coherence tomography,OCT)能快速、高分辨率地扫描视网膜内超微结构,常用于测量视盘参数、视盘旁RNFL厚度及黄斑区厚度,在青光眼诊断和预后判断中起到较为重要的作用[4-5]。本研究采用Topcon 3D OCT对40例(46眼)青光眼患者黄斑区视网膜进行测量,观察各参数与视野平均缺损(mean defect,MD)值的相关性,并与50例正常人进行比较,以探讨黄斑区各参数在青光眼诊断中的价值。
1 资料与方法
1.1一般资料选取2012年9月至2013年6月于我院就诊的青光眼患者40例(46眼)为青光眼组,其中男20例(24眼),女20例(22眼),年龄(59.77±10.64)岁,原发性慢性闭角型青光眼35眼,原发性开角型青光眼11眼。排除视神经疾病、黄斑病变、视网膜血管性病变、内眼手术等眼部其他疾患。另选取于我院同期健康体检的正常人50例(50眼)作为对照组,其中男25例,女25例,年龄(55.64±6.87)岁。两组性别比例及年龄差异均无统计学意义(均为P>0.05),具有可比性。对照组纳入标准:(1)视力或矫正视力≥1.0,屈光度≤±6.0 D;(2)眼压≤21 mmHg(1 kPa=7.5 mmHg);(3)视盘C/D≤0.5,双眼C/D差值<0.2;排除眼部及系统性疾病,同时排除青光眼家族史。所有研究对象均签署知情同意书。
1.2OCT检查青光眼组及对照组均接受常规眼部检查,包括视力、验光、裂隙灯、眼压、眼底、中心30°快速阈值视野检查。OCT检查采用Topcon 3D 1000 OCT(Ver 2.4)检测,无需散瞳。采用镜头内的黄斑注视点,光源波长840 nm,轴向分辨率5 μm,横向分辨率20 μm,扫描速度18 000 A·s-1,扫描深度2 mm,扫描模式选用512×64,扫描范围6 mm×6 mm。结合相应的彩色眼底扫描照片,测量和分析黄斑部位视网膜的厚度和结构变化。所有OCT均由同一技师操作检查。
1.3数据采集使用Topcon 3D OCT机器自带Fastmap2.4软件自动分析图像,采用ETDRS的分区方法对黄斑区进行分区。采集数据包括:黄斑中心凹1 mm内视网膜厚度,距黄斑1~3 mm内环上、颞、下、鼻各象限视网膜厚度,距黄斑3~6 mm外环上、颞、下、鼻各象限视网膜厚度,黄斑区视网膜体积及视网膜厚度,黄斑中心凹视网膜平均厚度。
1.4统计学方法所有数据均采用SPSS17.0软件进行统计分析,两组间黄斑区各参数的比较采用两独立样本的t检验,黄斑区视网膜厚度与MD之间的相关分析采用Pearson相关分析,P<0.05为差异有统计学意义。
2 结果
2.1两组黄斑区OCT图像特征对照组及青光眼组黄斑区厚度地形图均表现为黄斑中心凹最薄,对照组内环视网膜较外环视网膜厚,青光眼组内环及外环视网膜弥漫变薄或局限性变薄(图1)。
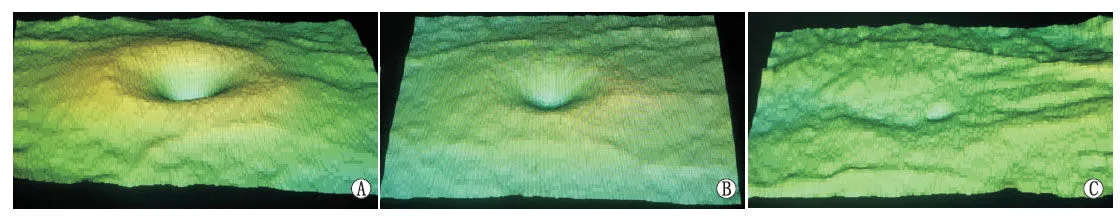
Figure 1 Macular images detected by 3D OCT of two groups.A:Control group,the inner-ring retina was thicker than the outer-ring;B:Glaucoma group,the local retina was thin;C:Glaucoma group,all retina was thin 两组黄斑区3D OCT图像特征。A:对照组内环视网膜较外环视网膜厚;B:青光眼组黄斑视网膜局限性变薄;C:青光眼组黄斑视网膜弥漫变薄
2.2两组黄斑区各参数比较两组黄斑区参数比较见表1。从表1可知,两组除黄斑中心凹1 mm内视网膜厚度、黄斑中心凹视网膜厚度差异比较无统计学意义(t=1.39、1.64,P=0.17、0.10)外,青光眼组黄斑内环各象限及黄斑外环各象限视网膜厚度、黄斑区视网膜体积及视网膜厚度均较对照组变薄或变小,差异均有统计学意义(均为P<0.05)。
2.3黄斑区视网膜厚度与MD的相关性青光眼组患者MD值为(9.96±6.28)dB;相关分析显示,青光眼组黄斑区视网膜厚度与MD呈负相关(r=-0.612,P=0.01)。
3 讨论
作为一种视功能不可逆性损伤的常见疾病,青光眼的诊断和随访非常重要,一旦在随访过程中发现病情进展,临床上即需要采取相应的治疗措施来干预,以阻止视功能进一步恶化。Na等[6]认为应用3D OCT综合检测视盘神经纤维层、视盘参数及黄斑区各参数能很好地评估青光眼病情的进展,但由于视盘结构相对复杂,视盘神经纤维层及视盘参数的检测并非总能得到较准确的结果。本研究应用3D OCT检测了青光眼患者黄斑区各参数,并与正常人眼进行了比较。
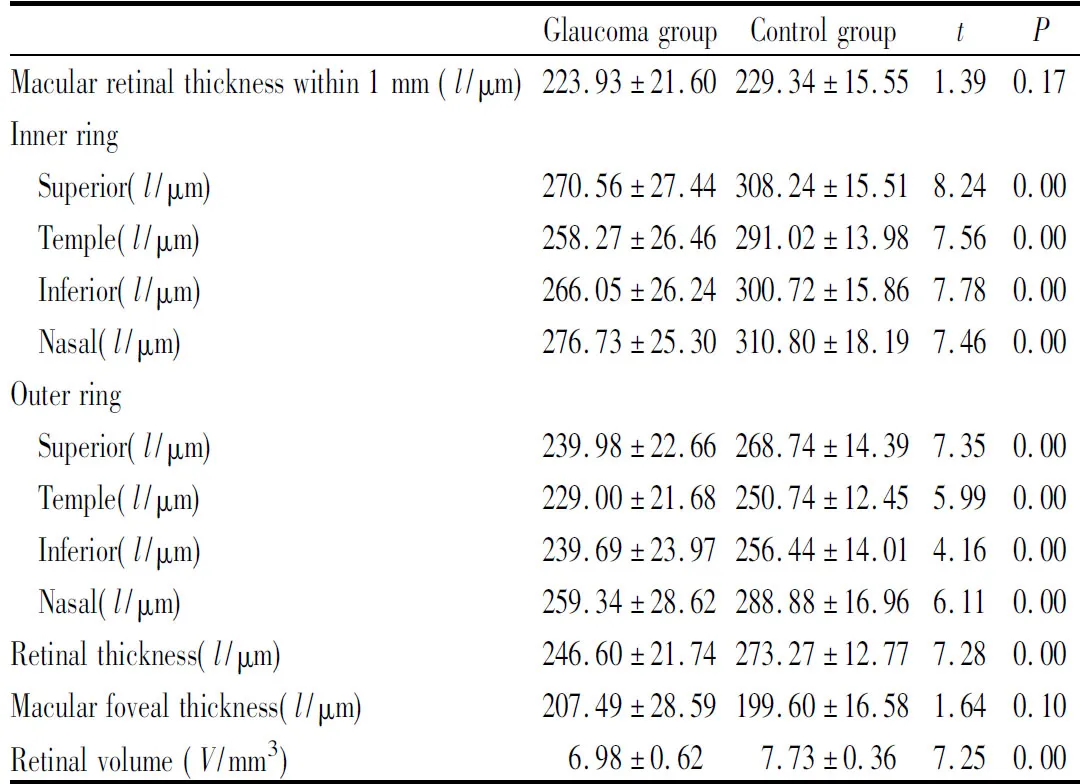
表1 两组黄斑区各参数比较Table 1 Comparison of each macular parameter between two groups

视野缺损是诊断青光眼的条件之一,只是目前其还是患者的主观检查,检查结果的准确性完全取决于患者的反应程度,且有些青光眼患者的RNFL和(或)视盘参数已经发生了改变,但视野检查并未出现异常[9-10]。因此,对视功能及神经视网膜结构改变要综合分析,才能更好地评估青光眼的进程。在本研究中青光眼黄斑区视网膜厚度与MD呈负相关,说明在青光眼的诊断和追踪上应用3D OCT检测黄斑区视网膜厚度与视野检查具有较好的一致性。
既往用时域OCT追踪黄斑区视网膜厚度,Medeiros等[11]认为运用时域OCT检测视盘旁RNFL厚度追踪青光眼病情发展比黄斑区视网膜厚度及视盘参数要好。随着OCT的发展,目前频域OCT扫描速度大大提高,且轴向最小分辨率从10 μm发展到现在的5 μm。Kotera等[12]认为在早期青光眼患者的黄斑区视网膜厚度和RNFL还没有改变的时候,内层视网膜厚度即比正常人要薄。随着OCT软硬件技术、设施的不断升级,应用OCT检测黄斑区内层视网膜厚度将有可能成为青光眼早期诊断、进展追踪的重要手段。
综上所述,目前视盘各参数及视盘旁RNFL厚度仍然是评估青光眼患者眼底结构改变的主要指标,但由于黄斑区解剖结构特点及OCT技术的不断革新,采用OCT检查可以方便、快捷地检测黄斑区视网膜厚度参数,利于青光眼的诊断和追踪,因此黄斑区视网膜OCT检测将有可能是青光眼诊断、追踪的重要手段之一。
1 Niessen AG,Van Den Berg TJ,Langerhorst CT,Greve EL.Retinal nerve fiber layer assessment by scanning laser polarimetry and standardized photography[J].AmJOphthalmol,1996,121(5):484-493.
2 Zeimer R,Asrani S,Zou S,Quiqley H,Jampel H.Quantitative detection of glaucomatous damage at the posterior pole by retinal thickness mapping.A pilot study[J].Ophthalmology,1998,105(2):224-231.
3 Nakatani Y,Higashide T,Ohkubo S,Takeda H,Suqiyama K.Evaluation of macular thickness and peripapillary retinal nerve fiber layer thickness for detection of early glaucoma using spectral domain optical coherence tomography[J].JGlaucoma,2011,20(4):252-259.
4 Guedes V,Schuman JS,Hertzmark E,Wollstein G,Correnti A,Mancini R,etal.Optical coherence tomography measurement of macular and nerve fiber layer thickness in normal and glaucomatous human eyes[J].Ophthalmology,2003,110 (1):177-189.
5 Leung CK,Chan WM,Yung WH,Ng AC,Woo J,Tsang MK,etal.Comparison of macular and peripapillary measurements for the detection of glaucoma:an optical coherence tomography study [J].Ophthalmology,2005,112 (3):391-400.
6 Na JH,Sung KR,Lee JR,Lee KS,Baek S.Detection of glaucomatous progression by spectral-domain optical coherence tomography[J].Ophthalmology,2013,120(7):1388-1395.
7 邢业娇,王大博,纪珍,刘鹏辉.海德堡OCT测量后极部视网膜厚度对青光眼诊断价值[J].青岛大学医学院学报,2013,49(1):38-43.
9 Kass MA,Heuer DK,Hagginbotham EJ,Johnson CA,Keltner JL,Miller JP,etal.The Ocular Hypertension Treatment Study:a randomized trial determines that topical ocular hypertensive medication delays or prevents the onset of primary open-angle glaucoma[J].ArchOphthalmol,2002,120(6):701-713.
10 Quigley HA,Katz J,Derick RJ,Gilbert D,Sommer A.An evaluation of optic disc and nerve fiber layer examinations in monitoring progression of early glaucoma damage[J].Ophthalmology,1992,99(1):19-28.
11 Medeiros FA,Zangwill LM,Alencar LM,Bowd C,Sample PA,Susanna R Jr,etal.Detection of glaucoma progression with stratus OCT retinal nerve fiber layer,optic nerve head,and macular thickness measurements[J].InvestOphthalmolVisSci,2009,50(12):5741-5748.
12 Kotera Y,Hangai M,Hirose F,Mori S,Yoshimura N.Three-dimensional imaging of macular inner structures in glaucoma by using spectral-domain optical coherence tomography[J].InvestOphthalmolVisSci,2011,52(3):1412-1421.
date:Sep 2,2013
Macular retinal thickness measured by three dimensional optical coherence tomography for glaucoma diagnosis
PANG Yan-Hua,ZHAO Gui-Ling,KE Yi,TAN Zhi,ZHU Min-Yi,LI Rui-Zhuang
optical coherence tomography;macular;retinal thickness;glaucoma
Objective To measure macular retinal thickness parameters in glaucoma patients and compare them with normal subjects using three dimensional optical coherence tomography (3D OCT),and discuss its value in glaucoma diagnosis.Methods A total of 40 patients (46 eyes) with glaucoma in our hospital from September 2012 to June 2013 were chosen as glaucoma group,and 50 healthy subjects (50 eyes) in control group.OCT imaging of macular area were examined using 3D OCT.The changes of macular thickness parameters in two groups were observed,the differences of image feature of macular topographic map were compared,and the correlation between macular retinal thickness and mean defect of visual field was analyzed.Results Macular retinal thickness in healthy subjects and patients with glaucoma topographic maps were the fovea at the thinnest.While inner-ring retinal thickness was much thicker than outer-ring retina in healthy subjects,inner-ring and outer-ring retinal thickness in patients with glaucoma were localized or diffuse thinning.The inner-ring retinal thickness,outer-ring retinal thickness,macular volume and average macular thickness in glaucoma group were thinner or smaller than those in control group,there were statistical differences(allP<0.05),but there were no statistical difference in central macular thickness with 1 mm and central fovea of macula thickness between two groups (t=1.39,1.64,P=0.17,0.10).The macular retinal thickness in glaucoma group was negative correlated with mean defect of visual field (r=-0.612,P=0.01).Conclusion Macular images detected by 3D OCT can be a useful method to determine glaucoma status and has a potential for tracking glaucoma progression.
庞燕华,女, 1980年6月出生,广西东兴人,主治医师。研究方向:青光眼、眼底病。联系电话:13553563810;E-mail:pangyh123@163.com
AboutPANGYan-Hua:Female,born in June,1980.Attending doctor.Tel:13553563810;E-mail:pangyh123@163.com
2013-09-02
524023 广东省湛江市,广东医学院附属医院眼科
李瑞庄,联系电话:13702886288
.庞燕华,赵桂玲,柯毅,谭志,朱敏怡,李瑞庄.3DOCT检测黄斑区视网膜厚度在青光眼诊断中的价值[J].眼科新进展,2014,34(5):468-470.
��
10.13389/j.cnki.rao.2014.0128
修回日期:2014-01-18
本文编辑:周志新
Accepteddate:Jan 18,2014
From theDepartmentofOphthalmology,AffiliatedHospitalofGuangdongMedicalCollege,Zhanjiang524023,GuangdongProvince,China
Responsibleauthor:LI Rui-Zhuang,Tel:13702886288
[RecAdvOphthalmol,2014,34(5):468-470]

