视神经疾病患者颅内压与眼内压变化的相关性
王大江,田 磊,赵 军,秦丽敏解放军总医院 眼科,北京 00853;辽河油田总医院 眼科,辽宁盘锦 400
视神经疾病患者颅内压与眼内压变化的相关性
王大江1,田 磊1,赵 军2,秦丽敏11解放军总医院 眼科,北京 100853;2辽河油田总医院 眼科,辽宁盘锦 124010
目的 探讨视神经疾病患者腰椎穿刺前后颅内压(intracranial pressure,ICP)与眼内压(intraocular pressure,IOP)变化的相关性。方法 前瞻性分析2013年1 - 5月解放军总医院眼科诊断视神经疾病12例(24眼)患者的相关资料。对诊断视神经疾病的12例入院患者的相关资料进行研究。所有患者住院期间通过腰椎穿刺留取定量脑脊液行脑脊液常规检查并测定ICP,同时采用回弹式眼压计测量腰椎穿刺前后双眼眼压变化,并计算其平均值。所有患者腰椎穿刺术后每2 h测量1次眼压,共12次,并绘制24 h眼压曲线。结果 共有12例(24眼)纳入本次研究,其中男7例,女5例,诊断为视神经炎6例,缺血性视神经病变5例,未明确诊断1例。患者年龄16 ~ 55(38.125±12.438)岁。所有患者全身状况良好,无高血压、糖尿病等常见全身疾病。腰椎穿刺前后ICP与双眼平均IOP之间无明显的相关性(r=0.126,P=0.697)。腰椎穿刺前后双眼IOP的差异(t=8.002,P<0.001)、ICP的差异(t=7.936,P<0.001)均有统计学意义。结论 IOP与ICP虽然有一定相关性,但是两者变化之间没有规律,以眼压推测颅压或者反之目前还不能得出有意义的结论。
青光眼;颅内压;眼内压
青光眼性视神经萎缩是青光眼患者的常见致盲原因。大量研究表明,高眼压是青光眼视神经损害进展的最主要危险因素,但临床上发现很多眼压正常患者的视神经损害。目前,对于正常眼压性青光眼(normal tension glaucoma,NTG)的发病机制还不完全清楚。最近的研究中,很多学者将焦点集中于颅内压(intracranial pressure,ICP)与眼内压(intraocular pressure,IOP)之差,也就是跨筛板压力差(眼压与脑脊液压力的差值)的变化上,认为这种压力差是造成正常眼压性青光眼视神经损害的主要原因[1-5]。那么究竟颅内压与眼内压存在怎样的关系,颅内压的变化是否会引起相应的眼内压变化,两者的变化是否存在一定规律性?本研究以视神经疾病患者为研究对象,测量腰椎穿刺前后颅内压变化及24 h眼压变化,为进一步揭示两者的相关性提供依据。
资料和方法
1 一般资料 2013年1 - 5月解放军总医院眼科诊断视神经疾病12例(24眼),其中男7例,女5例,诊断为视神经炎6例,缺血性视神经病变5例,未明确诊断1例。年龄16 ~ 55(38.13±12.44)岁。所有患者全身状况良好,无高血压、糖尿病等常见全身疾病。
2 方法 所有患者住院期间先行24 h眼压(1次/ 2 h)检查。次日通过腰椎穿刺留取定量(10 ml)脑脊液行脑脊液检查并测定ICP,记录腰椎穿刺前后双眼眼压,随后绘制腰椎穿刺后双眼24 h眼压曲线,并计算其平均值。眼压测量采用手持回弹式眼压计,平卧位测量眼压。
3 统计学处理 结果应用SPSS17.0软件进行统计学分析及绘图。Kolmogorov-Smirnov检验测量结果的正态分布数据用±s表示。腰穿操作前后眼内压及颅内压比较采用两独立样本t检验或Wilcoxon秩和检验。Pearson双变量相关分析腰穿操作前后眼内压和颅内压的相关性。P<0.05为差异有统计学意义。
结 果
1 腰穿前后颅内压及眼内压变化情况 腰穿前ICP均值为(200.83±27.12) mmH2O (1 mmH2O=9.807 Pa),腰穿后为(160.83±15.35) mmH2O,腰穿前后ICP值差异有统计学意义(P<0.001)。腰穿前IOP均值为(15.72±2.73) mmHg (1 mmHg=0.133 kPa),腰穿后为(14.01±2.72) mmHg,腰穿前后IOP值差异有统计学意义(P=0.034)。见图1。
2 腰穿前后颅内压与眼内压相关性分析 腰穿前IOP与ICP呈现明显正相关性(r=0.923,P<0.001);腰穿后IOP与ICP无明显相关性(r=0.44,P<0.152)。见图2。腰穿后右眼IOP变化均值为(1.52±1.09) mmHg,左眼IOP变化均值为(1.92±1.57) mmHg。腰穿后双眼IOP变化差异无统计学意义(P<0.48)。腰穿前后眼压变化与颅压变化无明显相关性(r=0.126,P=0.697)。见图3。
3 腰穿前后24 h眼压变化 腰穿后24 h平均眼压明显低于腰穿前24 h眼压,腰穿前24 h眼压均值(14.82±0.98) mmHg,腰穿后24 h眼压均值为(12.52±0.74) mmHg。腰穿前后24 h眼压变化差异有统计学意义(P<0.001)。见图4。
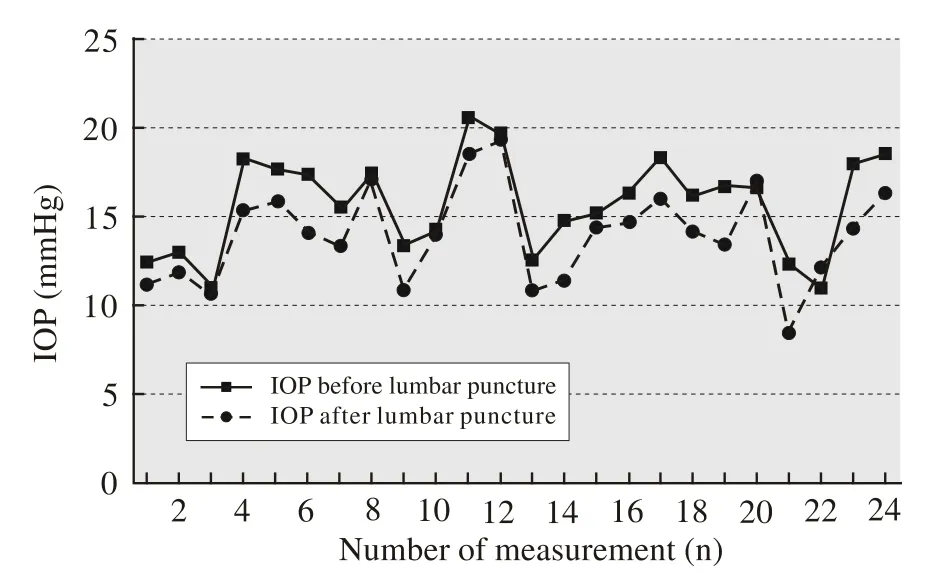
图 1 腰穿前后眼内压变化曲线Fig. 1 Curves of IOP changes before and after lumbar puncture
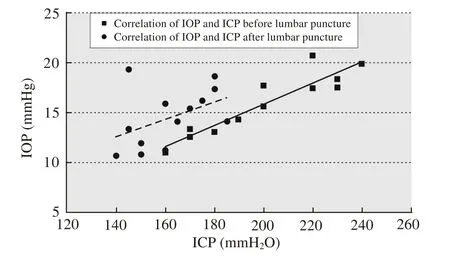
图 2 眼内压与颅内压的相关性分析Fig. 2 Correlation analysis of IOP and ICP
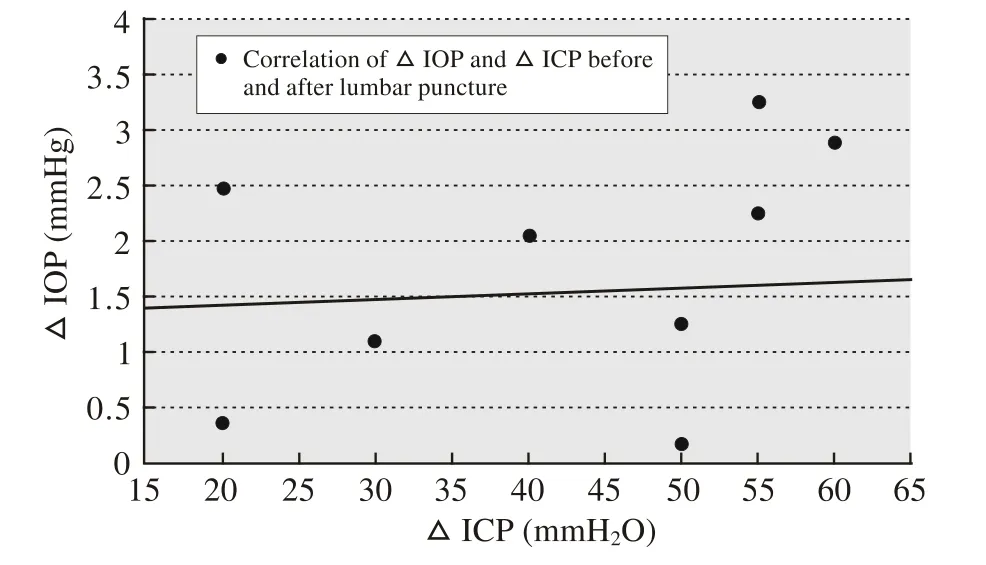
图 3 腰穿前后颅内压变化与眼内压变化的相关性分析Fig. 3 Correlation analysis of ICP and IOP changes before and after lumbar puncture
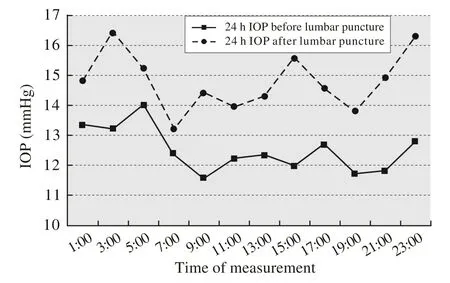
图 4 腰穿前后24 h眼内压变化曲线Fig. 4 Curve of 24 hours IOP changes before and after lumbar puncture
讨 论
随着临床上对正常眼压性青光眼认识的不断深入,ICP与IOP的关系已越来越受到眼科医生的重视[6-9]。众所周知,由于眼球与大脑邻近并与颅腔相沟通,视神经走行路径中有两处存在压力的部位:眼内和颅内。目前的一些研究表明,IOP和ICP之间的关系可能在青光眼的发生发展过程中起到重要作用[10-13]。ICP升高可通过以下机制引起IOP相应升高:1)眼内静脉大部分经眶上裂回流入颅内海绵窦,ICP升高可致眼静脉回流受阻,使上巩膜静脉压升高,影响房水循环,导致IOP升高。2)颅内及眼静脉壁薄且无瓣膜易于反流和受压,能够传递增高了的ICP。3)视神经鞘内充满脑脊液并与视交叉池相通,ICP升高通过视神经鞘内的脑脊液的传递,使眼内容量增加,导致IOP升高[14-15]。Berdahl等[12]的研究中对原发性开角型青光眼(primary open-angle glaucoma,POAG)患者、正常眼压性青光眼患者、高眼压症患者以及正常对照者的IOP和ICP进行比较,发现ICP在POAG患者和NTG患者中均比正常对照者低,而在高眼压症患者中比正常对照者高。研究结果提示,ICP在POAG和NTG的发生发展中可能起重要作用,并且在高眼压症患者中较高的颅内压可能对高眼压症发展成POAG有一定的预防作用。而在Ren等[13]的研究中,比较NTG患者、POAG患者和正常对照者的ICP和IOP的结果,发现ICP在NTG患者或正常对照者中均低,而跨筛板压力差(眼压与脑脊液压力的差值)在NTG患者和POAG患者中比正常对照者均较高,并且青光眼性视野损伤的程度和跨筛板压力差呈正相关。因此推测,在NTG患者中,脑脊液压力异常降低,导致了异常的筛板压力差,可能是导致视神经损伤的重要因素之一。Siaudvytyte等[16]的研究结果显示,青光眼患者的跨筛板压力差增大,在正常眼压性青光眼患者中,盘沿丢失与跨筛板压力差相关。国内Wang等[17]通过MRI测量视神经蛛网膜下腔的宽度替代测量颅压研究低颅压与NTG之间的关系,其研究结果显示,NTG患者的视神经蛛网膜下腔的宽度显著窄于高眼压的POAG患者及正常对照组,从而提示NTG的发病与跨筛板压力差有关,为NTG的诊断和治疗提供新的思路和方法。
但由于眼内压受到很多因素的影响,房水生成率、房水流出易度、房水流出阻力、上巩膜静脉压、ICP和血压等都会影响IOP,很难找到IOP与ICP的相关规律,并使通过IOP测定估计ICP在临床应用中也存在一定局限性。
本研究观察视神经疾病患者腰穿前后ICP的变化和IOP的变化,并首次观察腰穿前后24 h IOP的变化,期望找到ICP与IOP变化的相关性。结果显示,IOP与ICP呈正相关,ICP的降低会引起IOP的降低,在ICP恢复过程中,IOP也逐渐升高,但两者之间的变化并未见到明确的相关性,这一结果与Muchnok等[18]的研究结果一致。分析本研究的可能影响因素:1)本研究选取病人均为视神经疾病患者,可能存在一定特殊性;2)腰穿前后24 h IOP测量过程烦琐,需要患者及医护人员的协调配合,故因条件有限选取病人例数少可能影响结果。今后,我们将扩大样本量进行深入研究。
1 Morgan WH, Yu DY, Cooper RL, et al. The influence of cerebrospinal fluid pressure on the lamina cribrosa tissue pressure gradient[J]. Invest Ophthalmol Vis Sci, 1995, 36(6): 1163-1172.
2 Jonas JB, Berenshtein E, Holbach L. Anatomic relationship between lamina cribrosa, intraocular space, and cerebrospinal fluid space[J]. Invest Ophthalmol Vis Sci, 2003, 44(12): 5189-5195.
3 Burgoyne CF, Downs JC, Bellezza AJ, et al. The optic nerve head as a biomechanical structure: a new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage[J]. Prog Retin Eye Res,2005, 24(1): 39-73.
4 Berdahl JP, Allingham RR, Johnson DH. Cerebrospinal fluid pressure is decreased in primary open-angle glaucoma[J]. Ophthalmology,2008, 115(5): 763-768.
5 Ren R, Zhang X, Wang N, et al. Cerebrospinal fluid pressure in ocular hypertension[J]. Acta Ophthalmol, 2011, 89(2): e142-e148.
6 Yavin D, Luu J, James MT, et al. Diagnostic accuracy of intraocular pressure measurement for the detection of raised intracranial pressure: meta-analysis[J]. J Neurosurg, 2014, 23: 1-8.
7 Golan S, Kurtz S, Mezad-Koursh D, et al. Poor correlation between intracranial pressure and intraocular pressure by hand-held tonometry[J]. Clin Ophthalmol, 2013, 7: 1083-1087.
8 Kirk T, Jones K, Miller S, et al. Measurement of intraocular and intracranial pressure: is there a relationship?[J]. Ann Neurol,2011, 70(2): 323-326.
9 Li Z, Yang Y, Lu Y, et al. Intraocular pressure vs intracranial pressure in disease conditions: a prospective cohort study (Beijing iCOP study)[J]. BMC Neurol, 2012, 12:66.
10 Morgan WH, Chauhan BC, Yu DY, et al. Optic disc movement with variations in intraocular and cerebrospinal fluid pressure[J]. Invest Ophthalmol Vis Sci, 2002, 43(10): 3236-3242.
11 Ren R, Wang N, Zhang X, et al. Trans-lamina cribrosa pressure difference correlated with neuroretinal rim area in glaucoma[J]. Graefes Arch Clin Exp Ophthalmol, 2011, 249(7):1057-1063.
12 Berdahl JP, Fautsch MP, Stinnett SS, et al. Intracranial pressure in primary open angle glaucoma, normal tension glaucoma, and ocular hypertension: a case-control study[J]. Invest Ophthalmol Vis Sci,2008, 49(12): 5412-5418.
13 Ren R, Jonas JB, Tian G, et al. Cerebrospinal fluid pressure in glaucoma: a prospective study[J]. Ophthalmology, 2010, 117(2):259-266.
14 董云德,索班西.眼内压与颅内压关系的临床研究[J].中华神经外科杂志,1993,9(1):44-45.
15 李凤鸣.眼科全书[M].北京:人民卫生出版社,1996:288.
16 Siaudvytyte L, Januleviciene I, Ragauskas A, et al. The difference in translaminar pressure gradient and neuroretinal rim area in glaucoma and healthy subjects[J/OL]. http://www.hindawi.com/journals/ joph/2014/937360
17 Wang N, Xie X, Yang D, et al. Orbital cerebrospinal fluid space in glaucoma: the Beijing intracranial and intraocular pressure (iCOP)study[J]. Ophthalmology, 2012, 119(10): 2065-2073.e1.
18 Muchnok T, Deitch K, Giraldo P. Can intraocular pressure measurements be used to screen for elevated intracranial pressure in emergency department patients?[J]. J Emerg Med, 2012, 43(3):532-537.
Correlation of intracranial pressure and intraocular pressure changes in patients with optic nerve disease
WANG Da-jiang1, TIAN Lei1, ZHAO Jun2, QIN Li-min11Department of Ophthalmology, Chinese PLA General Hospital, Beijing 100853, China;2Department of Ophthalmology, The Central Hospital of Liaohe Oil Field, Panjin 124010, Liaoning Province, China
Objective To investigate the correlation of intracranial pressure (ICP) and intraocular pressure (IOP) changes in patients with optic nerve disease. Methods Clinical data about 12 patients with optic nerve disease admitted to our hospital from January to May in 2013 were retrospectively analyzed. The quantitative cerebrospinal fluid of all patients during hospitalization were extracted by lumbar puncture, and after that routine inspection of cerebrospinal fluid, the measurement of ICP were performed. The changes of before and after lumbar puncture were measured using spring back tonometer and the average value were calculated. 24-hour intraocular pressure curve was described with all patients undergoing the lumbar puncture once every 2 hours. Results Of the 12 cases (24 eyes), 7 cases were male and 5 cases were female with the average age of (38.125 ± 12.438) years old (range, 16-55 years old). 6 cases were diagnosed as optic neuritis, 5 cases were ischemic optic neuropathy, and 1 case was undefined diagnosis. All patients were in good condition with no high blood pressure, diabetes or any other common systemic disease. There was no significant correlation between before and after lumbar puncture ICP and eyes mean IOP (r=0.126, P=0.697). The differences of before and after lumbar puncture in IOP (t=8.002, P<0.001) and ICP (t=7.936, P<0.001) were statistically significant. Conclusion There is a certain correlation between IOP and ICP, but no regularity is found between the changes of them. Meaningful conclusion about presuming the IOP basing on the ICP or presuming the ICP basing on the IOP is yet to be educed.
glaucoma; intracranial pressure; intraocular pressure
R 778.1
A
2095-5227(2014)10-0993-04
10.3969/j.issn.2095-5227.2014.10.005
时间:2014-08-06 09:59
http://www.cnki.net/kcms/detail/11.3275.R.20140806.0959.001.html
2014-07-11
全国博士后特别资助项目(201104781)
Supported by China Postdoctoral Science Foundation(201104781)
王大江,男,副主任医师,博士,出站博士后。专业方向:青光眼、白内障及角膜病的临床基础研究。Email: wangdajiang 301@163.com
The First author: WANG Da-jiang. Email: wangdajiang301@163.com

