The clinical rehabilitation of spine and spinal cord disorders: detection and evaluation using SPECT/CT
The clinical rehabilitation of spine and spinal cord disorders: detection and evaluation using SPECT/CT
Spine-related disorders are caused by several factors including (1) spinal nerve/visceral nerve stimulation by perivertebral aseptic in fl ammation, (2) spinal nerve/visceral nerve compression by injured periverterbal soft tissue, dislocated perivertebral small joint, and proliferative/degenerative tissue and, (3) secondary damage to the spinal cord, peripheral nerve, vessels and autonomic nerve, which further stimulate nerve root sheath and surrounding pain-carrying nerve fi bers. In many cases, the source of pain cannot be detected by standard image modalities. Particularly in anatomically complex regions like the spine, SPECT/CT can be helpful for some aspects by introducing a metabolical dimension to the classical way of morphology-based diagnostic. The aim of the present review was to give an overview of the adoption of SPECT/CT in a clinical spine-focused setting.
Introduction
Beside degenerative alterations, fractures of the spine are a common cause of pain. Despite their small incidence they are of great importance due to potentially severe consequences even in those cases with no involvement of the spinal cord. Therefore, both degenerative alterations as well as fractures are an important fi eld of work within orthopaedic surgery and traumatology.
In order to reduce associated morbidity and mortality, a timely therapeutic intervention is necessary. Therefore, a suf fi cient diagnostic work-up is essential.
However, with standard image modalities, some fractures, especially those of the Pars intra articularis or occult fractures of the vertebral body can often not be detected. Furthermore, origin of back pain in cases of degenerative diseases is diagnosable in only about ten percent by the current imaging techniques (Janssen et al., 2011).
Within these techniques, myelography, plain radiography, computed tomography (CT), and magnetic resonance imaging (MRI) have to be mentioned. Newer imaging modalities are single-photon emissions computer tomography (SPECT) and hybrid imaging techniques like SPECT/CT. Latter combines the highly sensitive but non-speci fi c SPECT with very speci fi c but less sensitive CT (Gregory et al., 2004; Groves et al., 2004; Van der Wall and Fogelman, 2007; Hirschmann et al., 2010). Thus, identi fi cation of potential pain foci is mentioned to be as high as 92% in the cervical spine and 86% in the lumbar spine (Matar et al., 2013). For this reason, SPECT/CT is considered to be a valuable diagnostic addition. The aim of the present review was to give a short overview of the adoption of SPECT/CT in a clinical setting.
Traumatic spinal injuries
The estimated incidence of spinal fractures in literature is around 64 per 100,000 persons. In young patients, they usually occur in the presence of a substantial external force, whereas in elderly they can be the result of simple falls and represent the most common fi rst manifestation of osteoporosis. Consequences are often underestimated, especially in those cases with no involvement of the spinal cord. However, mortality rates in elderly after an osteoporotic spinal fracture are comparable to those after femoral neck fractures (Cauley JA et al., 2000). Thus, suf fi cient diagnostic work-up is essential in order to initiate a timely therapeutic intervention.
In this process, nuclear medicine imaging technologies today still play a minor role in general. Usually, most of the fractures might be diagnosed by means of a conventional X-ray or CT. However, several studies in the past have demonstrated advantages of planar scintigraphy, especially when searching for occult fractures and subtle lesions (Spitz et al., 1992; Heinrich et al., 1994). In these affected regions, bone metabolism is locally increased and perifocal hematoma, necrosis, as well as calcification may occur. The resulting phosphate complex then bonds with the Tc-99m-methylen-diphosphonate, which is utilized in SPECT (Love et al., 2003; Palestro et al., 2009).
Other neglected lesions by conventional imaging techniques are traumatic spondylolysis. These lesions occur on the basis of fractured pars inter articularis of the vertebral body and are believed to be caused by an axial loading injury to the lumbar spine in hyperextension. Due to the anatomical localization, they are frequently not visible on conventional radiographs or CT scans (Hession and Butt, 1996; Sairyo et al., 2006; Zukotynski et al., 2010). Due to the increased metabolic turnover of the affected region, sensitivity and speci fi city of SPECT is superior even partly to magnetic resonance imaging (Zukotynski et al., 2010). In combination with computed tomography, the lesions can readily be anatomically localized by SPECT/CT (Standaert and Herring, 2007; Zukotynski et al., 2010). Beside these acute traumatic injuries, stress fractures of the vertebral body occur with an incidence of around 6% and are normally located in the fourth or fi fth lumbar vertebra (Van der Wall et al., 2007). They are the result of repetitive stress leading to an imbalance of continuous bone resorption and formation. Especially young athletic patients are affected, whereby they complain about an acute onset of pain (Kainberger et al., 2006). Using CT, these fractures are missed in up to 15% of cases, whereas they are visible in SPECT/CT due to increased local bone uptake caused by increased osteoblast activity (Roub et al., 1979; Congeni et al., 1997).
In patients with normal bone turnover, the sensitivity for the detection of a fresh fracture using SPECT/CT is within the first 48 hours around 95% and after 72 hours 100% (Holder et al., 1990; Lee and Worsley, 2006). In elderly patients, time to initial fracture detection may be increased up to one week. Within 6-9 months, the visualized bone uptake continuously decreases as bone healing progresses (Matin, 1983), but may be visible up to three years following a fracture.
Due to the steady decrease of tracer uptake, SPECT/CT is of great interest in evaluation about fractures age. Particularly in cases of multiple spine deformities, such as compression fractures in elderly patients, this is of great interest to distinguish between fresh and old lesions. Besides the resulting diagnostic benefit, the information is of great importance to choose the right treatment. Especially the quality of percutaneous kyphoplasty depends on the selective use of this modality in patients with acute (> 6 weeks old) or sub-acute fractures (> 3 months old) because suboptimal outcome has been reported in patients with chronic fractures (Crandall et al., 2004; Buchbinder et al., 2009; Kallmes et al., 2009). To secure this, SPECT/CT is a helpful alternative compared to MRI, especially in patients where MRI is not practicable e.g., patient having pain while prolonged lying or due to motion artefacts which lead to inconclusive results.
Furthermore, SPECT/CT allows an accurate differentiation between malignant and benign compression fractures (Tokuda et al., 2011).
Degenerative spinal diseases
Osteoarthrosis is one of the most common articular af fl ictions and can affect every joint. In the spine, degenerative diseases occur within the cartilaginous joints, the uncovertebral joints, synovial joints and the fi brous joints.
Radiography, CT and MRI imaging may reveal signs of degeneration in patients with low back pain including disc space narrowing, vacuum phenomena, sclerotic vertebral margin, osteophysis, eburnation, perivertebral calci fi cation and spinal stenosis due to disc degeneration or facet joint cysts. However, similar fi ndings may be partly observed in asymptomatic patient, too. Thus, the relationship between imaging fi nding and clinical symptoms remains unclear to a certain extent. In contrast to mentioned imaging modalities SPECT/CT visualizes the morphologic changes as well as metabolic activities of osseous lesions. Due to the precise localisation of the increased tracer uptake conclusions can be drawn which lead to the source of suffered pain.
Most affected locations are the facet joints of the lumbar spine (Carstensen et al., 2011). Diagnosis is not always clear because osteoarthritis of these structures is commonly seen on radiographs in symptomatic as well as in asymptomatic individuals. Furthermore, other diseases like post-discectomy syndrome, spondylolisthesis or segmental instability can be associated with facet joint arthrosis as well. Using SPECT/CT, the affected facet joint can be visualised by increased tracer uptake (Matar et al., 2013). With this information the right therapy can be chosen e.g., targeted in fi ltration with corticosteroids and anaesthetics.
Degenerative changes of the discs can be visualized by signal changes within the functional unity of the disc and the cartilaginous endplate. Due to the degenerative alterations of the disc the mechanical (over) load increases within the endplate. As a result subchondral sclerosis and exophytic outgrowth as a sign of intervertebral osteochondrosis occur. In many cases degenerative changes appear at different location and extreme spinal osteophytosis is in great contrast to clinical symptoms. In these cases increased tracer uptake helps to differentiate between affected functional units (Figure 1). Due to the simultaneously conducted CT scan morphological information can be obtained to differentiate between degenerative changes and other skeletal abnormalities, in particular metastasis.

Figure 1 A 80 years old female with osteoporotic compression fracture of several vertebral bodies of the thoracic spine and lumbar spine (latter not shown).
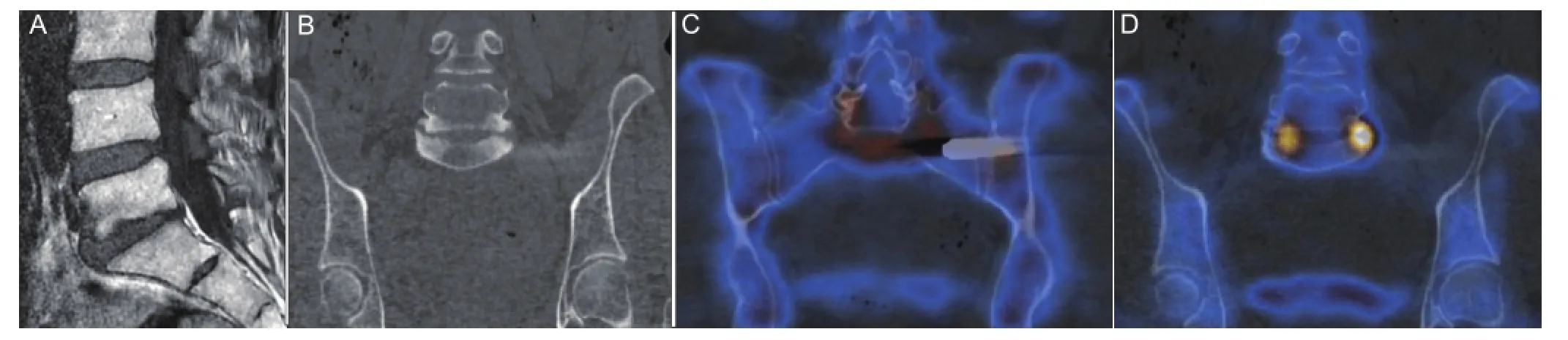
Figure 2 A 62 year old female patient with status post implantation of an “ifuse” rod for arthrodesis of the left iliosacral joint.
Malignant spinal lesions
To assess the presence and extend of bone metastases bone scinitgraphy using99mTc-labelled disphosphonates has long been the mainstay investigation. It is extremely sensitive, which makes it useful for screening for early stage metastatic bone lesions in patients with malignant tumors (Schmidt et al., 2005). The main de fi ciency of planar bone scans is their relative lack of speci fi city (Minoves, 2003). Thus, it can be dif fi cult to differentiate between metastases and other pathological fi ndings such as degenerative diseases, infections, lack of fi xation of metallic implants or benign bone tumors. Especially degenerative diseases often coexist in the cancer population due to in general older age. To clarify diagnosis, SPECT has been used to improve sensitivity (Kobayashi et al., 2005). In this context, certain patterns of tracer accumulation, like the focal uptake involving the vertebral body and the pedicles, have been shown to be more indicative for malignant diseases (Evan-Sapir et al., 1993). Further, the expansion of the lesion to the spinal canal with involvement or compression of the spinal cord is an ominous sign. Otherwise, increased uptake at the edge of the vertebral body adjacent to the disc or focal uptake in the facet joints without involvement of the pedicles is more characteristic for benign degenerative diseases (Evan-Sapir et al., 1993). However, the value of SPECT to exclude malignant involvement is controversial. Due to the additional anatomical imaging modality, SPECT/CT improves speci fi city compared with SPECT alone (Horger et al., 2004; Römer et al., 2006). In this context previous investigations by Horger and Bares demonstrated correct classi fi cation using SPECT/CT in over 85% of cases with equivocal foci, compared to 36% using SPECT alone.
Postoperative indications
Some patients report persistent pain following treatment of degenerative or traumatic af fl ictions of the spine with consecutive ilio-sacral arthrodesis or dorsal spine instrumentation and fusion. Due to persistent pain, previous vestigations demonstrated the need of additional surgeries within four years after surgery to be as high as 14% (Martin et al., 2007).
Beside other questions to be answered by a chosen imaging technique, the assessment of implant loosening like pedicle screws is of great value in those patients with persistent pain following instrumentation. Usually the question is addressed to conventional X-rays or CT scans. Despite recent developments regarding new sequence modalities, MRI due to signal artefacts often leads to inconclusive results (Rutherford et al., 2007). In this context, SPECT/CT provides an alternative since alteration by metal artefacts is decreased (Lusins et al., 1989; Larsen et al., 1996; Gates and McDonald, 1999) and loosening can be detected on the metabolical imaging component even if the CT is inconclusive based on metal artifacts.
Further pseudarthrosis after spinal fusion can be a cause of persistent pain, too. Usually, decrease of tracer uptake can be observed by SPECT/CT within the third postoperative month (Rager et al., 2012). In cases with consistently high uptake for more than a year after operation, non-union can be suspected (Gates and McDonald, 1999; Damgaard et al., 2010). Hereby previous investigations demonstrated that SPECT/CT seems to increase speci fi city for detection of non-union of interbody devices compared with CT scan alone (Rager et al., 2012). Especially to evaluate anterior fusion SPECT/CT seems to be superior (Rager et al., 2012).
After kyphoplasty or vertebroplasty, one of the most thoroughly documented complications are new vertebral compressions fractures of the adjacent segments (Uppin et al., 2003; Lin et al., 2004; Syed et al., 2005). Beside other risk factors like osteoporosis, prior vertebral fracture, cement leakage into the disk after treatment and older age the degree of height restoration of the cemented vertebrae increased the fracture risk of adjacent vertebrae (Kim et al., 2004). The following increased mechanical burden to the adjacent segments can be visualized by SPECT/CT (Figure 2). With this knowledge, a well-founded estimation can be made about the risk of adjacent fractures and whether a patient might pro fi t from an additional preventive operation.
Further questions to be answered by SPECT/CT are instability of the instrumentation, low-grade infection and fi nally epi- or subfusional degeneration by evaluating increased uptake due to (erosive) osteochondrosis (Rager et al., 2012).
Infection
In patients with suspicion of local infection due to trauma or surgery, confi rmation and determination of the exact location is of great interest. Using computed tomography or magnetic resonance imaging observed infection-related changes are normally very unspeci fi c nature and usually evident only in late stages. Furthermore, implant associated artefacts may substantially deteriorate image quality. Compared to CT and MRI, SPECT/CT allows the detection of an infection despite metal artefacts in the CT-component and the exact localization by visualising cortical destructions, foreign bodies, or sequestrums. Due to the detailed anatomical correlation it is furthermore helpful to differentiate between osteomyelitis and soft tissue infections (Bar-Shalom et al., 2006). Therefore, it plays an important role in the detection of implant-associated infections (Navalkissoor et al., 2013). To securethis and to improve sensitivity and speci fi city a combination between Dicarboxypropandiphosphonat (DPD) scintigraphy with radioactively marked leucocytes is recommended (Navalkissoor et al., 2013). In Europe, anti-granulocyte scintigraphy is more popular and has been proven equal in value (Richter et al., 2011). However, it must be mentioned that sensitivity and speci fi city vary depending on the body region. In the area of the spine FDGPET/CT is currently the standard imaging modality and superior to SPECT/ CT. Latter is used when detecting an infection of an extremity (Stumpe et al., 2002; Linke et al., 2010).
Conclusion
Beside the common imaging modalities, SPECT/CT has proved to be very helpful in clinical routine by introducing a physiological dimension to our classical way of morphology based diagnostic. However, applicability for spinal cord pathologies is rare, it is of great interest in anatomically complex regions such as the spine to evaluate the enclosing structures of the spinal cord.
Max J. Scheyerer1, Clément M.L.Werner2, Patrick Veit-Haibach3,4
1 Centre for Orthopaedic and Trauma Surgery, University Medical Center, Josef-Stelzmann-Str.9, Cologne, Germany
2 Department of Surgery, Division of Trauma, Surgery, University Hospital Zurich, Zurich, Switzerland
3 Department of Medical Radiology, Division of Nuclear Medicine, University Hospital Zurich, Zurich, Switzerland
4 Department of Medical Radiology, Diagnostic and Inverventional Radiology, University Hospital Zurich, Zurich, Switzerland
Author contributions: Scheyerer MJ drafted the manuscript and created images. Werner CML made criticle revisions. Veit-Haibach P drafted the manuscript, created images and made criticle revisions. All authors approved the final version of this paper.
Con fl icts of interest: Patrick Veit-Haibach received IIS Grants from Bayer Healthcare, Siemens Medical Solutions, GE Healthcare, Roche Pharma and speaker fees from GE Healthcare. The remaining authors declare that they have no conflict of interest.
Bar-Shalom R, Yefremov N, Guralnik L, Keidar Z, Engel A, Nitecki S, Israel O (2006) SPECT/CT using 67Ga and 111In-labeled leukocyte scintigraphy for diagnosis of infection. J Nucl Med 47:587-594.
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B (2009) A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 361:557-568.
Carstensen MH, Al-Harbi M, Urbain JL, Belhocine TZ (2011) SPECT/CT imaging of the lumbar spine in chronic low back pain: a case report. Chiropr Man Therap 19:2.
Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D (2000) Risk of mortality following clinical fractures. Osteoporos Int 11:556-561.
Crandall D, Slaughter D, Hankins PJ, Moore C, Jerman J (2004) Acute versus chronic vertebral compression fractures treated with kyphoplasty: early results. Spine J 4:418-424.
Congeni J, McCulloch J, Swanson K (1997) Lumbar spondylolysis. A study of natural progression in athletes. Am J Sports Med 25:248-253.
Damgaard M, Nimb L, Madsen JL (2010) The role of bone SPECT/CT in the evaluation of lumbar spinal fusion with metallic fi xation devices. Clin Nucl Med 35:234-236.
Even-Sapir E, Martin RH, Barnes DC, Pringle CR, Iles SE, Mitchell MJ (1993) Role of SPECT in differentiating malignant from benign lesions in the lower thoracic and lumbar vertebrae. Radiology 187:193-198.
Gates GF, McDonald RJ (1999) Bone SPECT of the back after lumbar surgery. Clin Nucl Med 24:395-403.
Gregory PL, Batt ME, Kerslake RW, Scammell BE, Webb JF (2004) The value of combining single photon emission computerised tomography and computerised tomography in the investigation of spondylolysis. Eur Spine J 13:503-509.
Groves AM, Bird N, Tabor I, Cheow HK, Balan KK (2004) 16-Detector multislice CT-skeletal scintigraphy image co-registration. Nucl Med Commun 25:1151-1155.
Heinrich SD, Gallagher D, Harris M, Nadell JM (1994) Undiagnosed fractures in severely injured children and young adults. Identi fi cation with technetium imaging. J Bone Joint Surg Am 76:561-572.
Hession PR, Butt WP (1996) Imaging of spondylolysis and spondylolisthesis. Eur Radiol 6:284-290.
Hirschmann MT, Iranpour F, Davda K, Rasch H, Hugli R, Friederich NF (2010) Combined single-photon emission computerized tomography and conventional computerized tomography (SPECT/CT): clinical value for the knee surgeons? Knee Surg Sports Traumatol Arthrosc 18:341-345.
Holder LE, Schwarz C, Wernicke PG, Michael RH (1990) Radionuclide bone imaging in the early detection of fractures of the proximal femur (hip): multifactorial analysis. Radiology 174:509-515.
Horger M, Eschmann SM, Pfannenberg C, Vonthein R, Besenfelder H, Claussen CD, Bares R (2004) Evaluation of combined transmission and emission tomography for classi fi cation of skeletal lesions. Am J Roentgenol 183:655-661.
Janssen M, Nabih A, Moussa W, Kawchuk GN, Carey JP (2011) Evaluation of diagnosis techniques used for spinal injury related back pain. Pain Res Treat 2011:478798.
Kainberger F, Weidekamm C, Matzner M, Trieb K (2006) Sports injury of the spine: imaging diagnosis. Rontgenpraxis 56:47-57.
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W, Ghdoke B, Annesley-Williams DJ, Ralston SH, Jarvik JG (2009) A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 361:569-579.
Kim SH, Kang HS, Choi JA, Ahn JM (2004) Risk factors of new compression fractures in adjacent vertebrae after percutaneous vertebroplasty. Acta Radiol 45:440-445.
Kobayashi K, Okuyama C, Kubota T, Nakai T, Ushijima Y, Nishimura T (2005) Do shorttime SPECT images of bone scintigraphy improve the diagnostic value in the evaluation of solitary lesions in the thoracic spine in patients with extraskeletal malignancies? Ann Nucl Med 19:557-566.
Larsen JM, Rimoldi RL, Capen DA, Nelson RW, Nagelberg S, Thomas JC, Jr. (1996) Assessment of pseudarthrosis in pedicle screw fusion: a prospective study comparing plain radiographs, fl exion/extension radiographs, CT scanning, and bone scintigraphy with operative fi ndings. J Spinal Disord 9:117-120.
Lee E, Worsley DF (2006) Role of radionuclide imaging in the orthopedic patient. Orthop Clin North Am 37:485-501, viii.
Lin EP, Ekholm S, Hiwatashi A, Westesson PL (2004) Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol 25:175-180.
Linke R, Kuwert T, Uder M, Forst R, Wuest W (2010) Skeletal SPECT/CT of the peripheral extremities. AJR Am J Roentgenol 194:W329-335.
Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ (2003) Radionuclide bone imaging: an illustrative review. Radiographics 23:341-358.
Lusins JO, Danielski EF, Goldsmith SJ (1989) Bone SPECT in patients with persistent back pain after lumbar spine surgery. J Nucl Med 30:490-496.
Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA (2007) Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine (Phila Pa 1976) 32:2119-2126.
Matar HE, Navalkissoor S, Berovic M, Shetty R, Garlick N, Casey AT, Quigley AM (2013) Is hybrid imaging (SPECT/CT) a useful adjunct in the management of suspected facet joints arthropathy? Int Orthop 37:865-870.
Matin P (1983) Bone scintigraphy in the diagnosis and management of traumatic injury. Semin Nucl Med 13:104-122.
Minoves M (2003) Bone and joint sports injuries. The role of bone scintigraphy. Nucl Med Commun 13:31-35.
Navalkissoor S, Nowosinska E, Gnanasegaran G, Buscombe JR (2013) Single-photon emission computed tomography-computed tomography in imaging infection. Nucl Med Commun 34:283-290.
Palestro CJ, Love C, Schneider R (2009) The evolution of nuclear medicine and the musculoskeletal system. Radiol Clin North Am 47:505-532.
Rager O, Schaller K, Payer M, Tchernin D, Ratib O, Tessitore E (2012) SPECT/CT in differentiation of pseudarthrosis from other causes of back pain in lumbar spinal fusion: report on 10 consecutive cases. Clin Nucl Med 37:339-343.
Richter WS, Ivancevic V, Meller J, Lang O, Le Guludec D, Szilvazi I, Amthauer H, Chossat F, Dahmane A, Schwenke C, Signore A (2011) 99mTc-besilesomab (Scintimun) in peripheral osteomyelitis: comparison with 99mTc-labelled white blood cells. Eur J Nucl Med Mol Imaging 38:899-910.
Römer W, Nömayr A, Uder M, Bautz W, Kuwert T (2006) SPECT-guided CT for evaluating foci of increased bone metabolism classi fi ed as indeterminate on SPECT in cancer patients. J Nucl Med 47:1102-1106.
Roub LW, Gumerman LW, Hanley EN, Jr., Clark MW, Goodman M, Herbert DL (1979) Bone stress: a radionuclide imaging perspective. Radiology 132:431-438.
Rutherford EE, Tarplett LJ, Davies EM, Harley JM, King LJ (2007) Lumbar spine fusion and stabilization: hardware, techniques, and imaging appearances. Radiographics 27:1737-1749.
Sairyo K, Katoh S, Takata Y, Terai T, Yasui N, Goel VK, Masuda A, Vadapalli S, Biyani A, Ebraheim N (2006) MRI signal changes of the pedicle as an indicator for early diagnosis of spondylolysis in children and adolescents: a clinical and biomechanical study. Spine 31:206-211.
Schmidt GP, Schoenberg SO, Resier MF, Baur-Melnyk A (2005) Whole-body imaging of bone marrow. Eur J Radiol 55:33-40.
Spitz J, Becker C, Tittel K, Weigand H (1992) Clinical relevance of whole body skeletal scintigraphy in multiple injury and polytrauma patients. Unfallchirurgie 18:133-147.
Standaert CJ, Herring SA (2007) Expert opinion and controversies in sports and musculoskeletal medicine: the diagnosis and treatment of spondylolysis in adolescent athletes. Arch Phys Med Rehabil 88:537-540.
Stumpe KD, Zanetti M, Weishaupt D, Hodler J, Boos N, Von Schulthess GK (2002) FDG positron emission tomography for differentiation of degenerative and infectious endplate abnormalities in the lumbar spine detected on MR imaging. AJR Am J Roentgenol 179:1151-1157.
Syed MI, Patel NA, Jan S, Harron MS, Morar K, Shaikh A (2005) New symptomatic vertebral compression fractures within a year following vertebroplasty in osteoporotic women. AJNR Am J Neuroradiol 26:1601-1604.
Tokuda O, Harada Y, Ueda T, Ohishi Y, Matsunaga N (2011) Malignant versus benign vertebral compression fractures: can we use bone SPECT as a substitute for MR imaging? Nucl Med Commun 32:192-198.
Uppin AA, Hirsch JA, Centenera LV, P fi efer BA, Pazianos AG, Choi IS (2003) Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology 226:119-124.
Van der Wall H, Fogelman I (2007) Scintigraphy of benign bone disease. Semin Musculoskelet Radiol 11:281-300.
Zukotynski K, Curtis C, Grant FD, Micheli L, Treves ST (2010) The value of SPECT in the detection of stress injury to the pars interarticularis in patients with low back pain. J Orthop Surg Res 5:13.
Max J. Scheyerer, M.D., Centre for Orthopaedic and Trauma Surgery, University Medical Center, Josef-Stelzmann-Str.9, Cologne 50924, Germany, maxjscheyerer@gmail.com .
10.4103/1673-5374.131593 http://www.nrronline.org/
Accepted: 2014-04-11
Scheyerer MJ, Werner CML, Veit-Haibach P. The clinical rehabilitation of spine and spinal cord disorders: detection and evaluation using SPECT/CT. Neural Regen Res. 2014;9(8):795-797.
- 中国神经再生研究(英文版)的其它文章
- The synthetic thyroid hormone, levothyroxine, protects cholinergic neurons in the hippocampus of naturally aged mice
- Citalopram increases the differentiation ef fi cacy of bone marrow mesenchymal stem cells into neuronal-like cells
- Fusion protein of single-chain variable domain fragments for treatment of myasthenia gravis
- Similar effects of substance P on learning and memory function between hippocampus and striatal marginal division
- Regulatory effects of anandamide on intracellular Ca2+concentration increase in trigeminal ganglion neurons
- Virtual reality interface devices in the reorganization of neural networks in the brain of patients with neurological diseases

