A Case of Thoracic Spinal Stenosis Secondary to Paget's Disease
Yu Zhao, Yi-peng Wang, Gui-xing Qiu,Jian-xiong Shen, Xi-sheng Weng, Xiang Li, and Nai-guo Wang
Department of Orthopedic Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
PAGET'S disease, also called osteitis deformans, is a metabolic bone disorder. It is characterized by increased bone resorption and the compensatory formation of new bones. The increased bone conversion and remodeling lead to the incrustation of woven bones and lamellar bones and finally result in the expansion, loosening, and excessive vascularization of the affected bones, rendering them susceptible to deformity and fracture.1Paget's disease occurs much more commonly in Anglo-Saxons than in Asians and Africans. Only a few cases have been reported in China, and the condition in those cases involved the pelvis and tibia.2A patient with Paget's disease was admitted into our hospital in June 2009 and was treated with surgery for secondary thoracic spinal stenosis. Given the rarity of Paget's disease, we expected to contribute to the study in this field by reporting the case with spinal involvement requiring surgical treatment, which has rarely been documented so far.
CASE DESCRIPTION
In June 2009, a 46-year-old female rural patient was hospitalized in the Department of Orthopedic Surgery, complaining of back pain, and concurrent numbness and weakness in the lower limbs. The symptoms had persisted for 9 months and worsened over the previous 4 months. Upon admission, she did not have superficial lymphadenopathy but demonstrated bilateral hypoesthesia along the trunk below the navel and along the lower limbs. The muscle tone of the lower limbs was mildly increased (Grade III-IV in left leg and Grade IV in right leg). The bilateral abdominal reflexes could not be elicited, but the bilateral patellar and Achilles reflexes were active. Babinski's sign was positive, and clonus was noted in both ankles. On the other hand, the sensation, movement, and reflexes of the upper limbs were normal.
Laboratory results revealed normal serum calcium and phosphorus levels, but the serum alkaline phosphatase (ALP) level was found significantly elevated to 755 U/L (reference value, 30-110 U/L). No abnormality was detected in the series tests for myeloma. Doppler ultrasonography did not reveal any abnormality in the abdomen, breasts, thyroid gland, or parathyroid glands. Myelography and computed tomographic myelography (CTM) detected ossification of yellow ligaments at T10-T12 and compression of the local dural sac (Fig. 1). Multiple thoracic and lumbar segments manifested osteomalacia-like changes (Fig. 2). Posteroanterior pelvic radiography revealed that the bone trabeculae had become hypertrophic, sparse, and irregularly arranged (Fig. 3). A lateral plain film of the skull showed typical cotton-wool appearance (Fig. 4).
After consulting with an endocrinologist, the diagnosis of Paget's disease was confirmed, and zoledronic acid was administered on June 10, 2009. The serum ALP level was reduced to 425 U/L within 3 weeks after the administration of zoledronic acid; however, the back pain and the numb- ness, pain, and weakness in the patient's lower limbs were not ameliorated obviously. The patient underwent surgical procedure on June 30, 2009, including posterior laminectomy at T10-T12, bone cement augmentation of screw fixation for T5-L2 vertebral pedicles, and graft fusion. The volume of intraoperative hemorrhage was approximately 4 000 mL; therefore, apart from 1 500 mL of autologous blood, 8 units of allogeneic erythrocyte suspension and 400 mL of plasma were transfused.
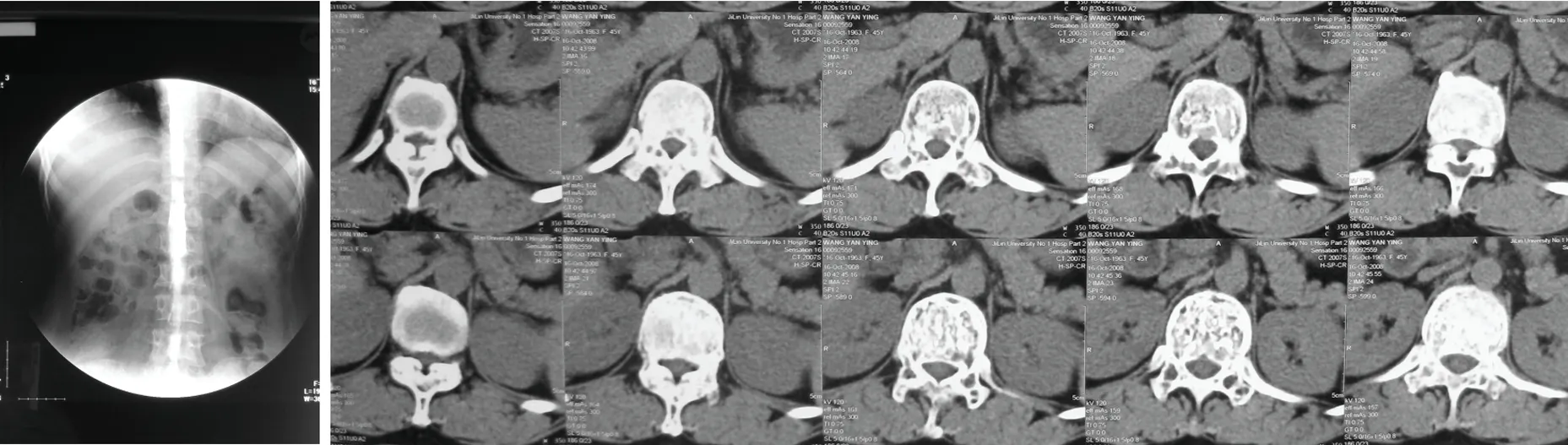
Figure 1. Myelography reveals ossification of yellow ligaments at T10-T12 (A) and computed tomographic myelography (CTM) reveals compression of the local dural sac (B).

Figure 2. Osteomalacia-like changes in multiple thoracic and lumbar segments in the lateral lumbar and thoracolumbar spine radiography.

Figure 3. Hypertrophic, sparse, and irregularly arranged bone trabeculae in posteroanterior pelvic radiography.

Figure 4. Typical cotton-wool appearance in a plain skull radiography.
The volume of drainage from the wound on day 1 and day 2 after the operation was 500 mL and 200 mL, respectively. The drainage tube was removed on day 3. The back pain was ameliorated when the patient started to take some off-bed activities, and the strength of her left leg recovered slightly compared to preoperative level, but the numbness and pain persisted. The wound healed well.
Immediate postoperative radiography revealed that a screw was inappropriately placed on the left of T9 segment (Fig. 5), although the patient did not complain of any discomfort. Postoperative pathological examination confirmed the diagnosis of Paget's disease at the mixed stage.
At the follow-up visit three months after the operation, scars were found to have healed, the ambulation function improved, and the lumbodorsal pain was partially ameliorated; however, the numbness and pain in her lower limbs were not ameliorated significantly.

Figure 5. Immediate postoperative anteroposterior view (A)and lateral view (B) of the thoracic and lumbar spine.A screw is revealed to be inappropriately placed on the left of T9 segment.
DISCUSSION
Paget's disease is a metabolic bone disorder that was first described by John Paget in 1877.3Its etiology remains unknown and is thought to be associated with viral infection and genetic factors. The incidence varies significantly with race, age, and diagnostic techniques. It affected 1%-2% of the American population and was more prevalent in the age group of 65-74 years.4Its mean incidence was calculated at 2.32% (SD, 0.54%). However, no significant gender difference was found in its prevalence.
The spinal column is the second most commonly affected next only to pelvis in Paget's disease, and the spinal involvement is noted in 15.2% of the patients.5Patients with thoracic vertebrae involvement exhibit symptoms because of the relatively small canal volume in this segment; however, lumbar vertebrae are in fact the most commonly involved spinal segment (58%), according to imaging studies.5
Bone remodeling in Paget's disease usually occurs in periostea. Periosteal bone deposition, which is found to be the most common form in remodeling, ultimately leads to spinal stenosis by causing expansive growth of the vertebral bodies, producing clinical symptoms of nerve damage. Meanwhile, the height of the vertebrae remains constant since the superior and inferior surfaces are not covered by periosteum, unless the condition is complicated by a pathological fracture. The presence of these features differentiates Paget's disease from other disorders.6
In the present case, ossification of the yellow ligaments was noted primarily in the segment with the highest degree of stenosis. Pathological examination of the resected vertebral plates revealed typical features of Paget's disease, although these features were not evident in imaging examinations. This finding suggested that the ossification of the yellow ligaments might be one of the factors causing spinal stenosis. Hepgül et al7reported a patient receiving surgical treatment for thoracic spinal stenosis associated with Paget's disease. At the surgery, the yellow ligaments were found to be calcified, and the epidural adipose tissue at the stenotic sites severely compressed the dura mater. The postoperative pathological findings revealed that the structural abnormalities of the bone in Paget's disease extended to the bone-ligament junctions, indicating that calcification of the soft tissue structures might be a pathological change directly associated with Paget's disease. Other less common causes of spinal stenosis in Paget's disease are epidural hematoma, pathological fracture, and osteosarcomatous changes.8Therefore, clinical data should be closely reviewed before operation to identify the cause of nerve compression and to select appropriate treatment accordingly.
For patients demonstrating symptoms of nerve damage due to spinal stenosis, medical treatment is preferred. Apart from the commonly used bisphosphonates and calcitonin, zoledronic acid is being increasingly used for its convenient activity duration of one year per dose.1,8
For patients not responding to medication, surgical decompression should be considered. Sadar et al9reported that nerve damage symptoms were ameliorated by surgery to various degrees in 85% patients; however, the surgical mortality was as high as 11% and was mainly attributable to hemorrhagic shock due to excessive blood loss. Preoperative radionuclide bone scanning was recommended for controlling intraoperative hemorrhage. Furthermore, in cases where the speed of blood flow at the surgical sites is found to rise to an abnormal level, drugs against Paget's disease should be preoperatively administered until the local blood flow returns to normal.5For this purpose, calcitonin should be administered for 2-3 months and mithramycin for 2-3 weeks; intravenous administration of bisphosphonates would achieve similar therapeutic effect.5In the present case, despite preoperative medication and back-to-normal serum ALP level, the volume of intraoperative hemorrhage was up to 4 500 mL. In addition to the cancellous bones in the process of decompression, the paraspinal muscles and the wound were all bleeding sites during the operation, posing difficulties for hemostasis. Intraoperative autologous transfusion is therefore strongly recommended for patients requiring surgical intervention.
In addition to the imaging findings and bone metabolism parameters, the clinical outcomes of patients are the main indices of the therapeutic effectiveness. Sadar et al9found that some patients with Paget's disease exhibited progressive clinical symptoms of nerve damage although myelography did not reveal any sign of spinal stenosis. These findings indicated that osseous compression might not be the only cause of nerve damage symptoms in patients with Paget's disease. Radioisotope bone blood flow scanning revealed that the blood supply to the bones accounts for 18% of the cardiac output in patients with Paget's disease, compared with only 5% in normal control subjects.10Increased blood supply to the vertebrae relatively decreased the blood supply to the spinal cord, resulting in arterial blockage.4Obviously, simple surgical intervention cannot treat such a condition. Medication could reduce the activity of bone metabolism and is likely to increase the blood supply to the spinal cord, thereby improving nerve function.
The spinal stability should be taken into account when decompression is considered for all types of spinal disorders. In the present case, multiple vertebral segments were involved; posterior screw fixation for the vertebral pedicles was performed to avoid iatrogenic kyphosis that could be caused by simple laminectomy. The intraoperative use of bone cement strengthened the holding force of the screws, preventing them from loosening due to osteoporosis. Detailed reports are still needed on the long-term clinical outcomes of the application of vertebral pedicle screws for Paget's disease and on whether the use of bone cement could reduce the risk of internal fixation failure. Further investigations are therefore necessary for better and clearer understanding of those problems.
1. Malik AR, Lone NA, Rather HA, et al. Asymptomatic Paget's disease of bone presenting with complete atrioventricular block. Chin Med J (Engl) 2008; 121:2357-9.
2. Yan TQ, Guo W, Shen DH. Osteitis deformans. Chin J Orthop 2002; 22:100-2.
3. Paget J. On a form of chronic inflammation of bones (Osteitis deformans). Med Chir Trans 1877; 60:37-63.
4. Altman RD, Bloch DA, Hochberg MC, et al. Prevalence of pelvic Paget's disease of bone in the United States. J Bone Miner Res 2000; 15:461-5.
5. Hadjipavlou AG, Gaitanis IN, Katonis PG, et al. Paget's disease of the spine and its management. Eur Spine J 2001; 10:370-84.
6. Dell'Atti C, Cassar-Pullicino VN, Lalam RK, et al. The spine in Paget's disease. Skeletal Radiol 2007; 36:609-26.
7. Hepgül K, Nicoll JA, Coakham HB. Spinal cord compression due to pagetic spinal stenosis with involvement of extradural soft tissues: a case report. Surg Neurol 1991; 35:143-6.
8. Hadjipavlou AG, Gaitanis IN, Kontakis GM. Paget's disease of the bone and its management. J Bone Joint Surg Br 2002; 84:160-9.
9. Sadar ES, Walton RJ, Gossman HH. Neurological dysfunction in Paget's disease of the vertebral column. J Neurosurg 1972; 37:661-5.
10. Poncelet A. The neurologic complications of Paget's disease. J Bone Miner Res 1999; 14 Suppl 2:88-91.
 Chinese Medical Sciences Journal2010年2期
Chinese Medical Sciences Journal2010年2期
- Chinese Medical Sciences Journal的其它文章
- Lipids-induced Apoptosis Is Aggravated by Acyl-coenzyme A: Cholesterol Acyltransferase Inhibitor△
- Gaussia Luciferase Reporter Assay for Assessment of Gene Delivery Systems in Vivo△
- DTNBP1 Gene Is Associated with Some Symptom Factors of Schizophrenia in Chinese Han Nationality△
- Association between the Epidermal Growth Factor Gene and Intelligence in Major Depression Patients△
- Role of Acetylated p53 in Regulating the Expression of map2 in Retinoic Acid-induced P19 Cells△
