PCNL术后发生SIRS的危险因素分析

[摘" "要]" "目的:探讨经皮肾镜取石术(percutaneous nephrolithotomy, PCNL)术后发生全身炎症反应综合征(systemic inflammatory response syndrome, SIRS)的危险因素,为制订防治SIRS发生的方案提供参考。方法:回顾性分析2019年1月—2020年12月于南通大学附属常熟医院行PCNL 97例患者的临床资料。根据术后是否出现SIRS,分为SIRS组和非SIRS组。比较两组患者性别、年龄、BMI、高血压病、糖尿病、术前尿WBC、肾周脂肪条索影(perirenal fat stranding, PFS)、结石长径、手术通道、手术时间的差异。使用多因素Logistic回归分析SIRS发生的危险因素。结果:两组患者性别、年龄、BMI、高血压病、糖尿病、结石长径、手术通道、手术时间差异均无统计学意义(均P>0.05);术前尿WBC、PFS差异有统计学意义(P<0.05)。纳入BMI、糖尿病、术前尿WBC、PFS、手术通道和手术时间行多因素Logistic回归分析显示,术前尿WBC阳性、存在PFS是SIRS发生的独立危险因素(P<0.05)。结论:PCNL术后发生SIRS和术前尿WBC阳性、存在PFS相关,关注术前尿WBC和PFS,必要时给予充分的抗感染治疗可能是减少SIRS发生的重要措施。
[关键词]" "全身炎症反应综合征;经皮肾镜取石术;肾周脂肪条索影;危险因素
[中图分类号]" "R691.4" " " " " " " "[文献标志码]" "A" " " " " " " "[文章编号]" "1674-7887(2024)02-0159-04
Analysis of risk factors for post-PCNL SIRS*
FU Zhenyu**#, LU Ke**#, HU Jun, SHI Ming, YU Muyuan, BEI Minglong, GU Yifeng, CHEN Yongchang, ZHANG Ge***" " " " (Department of Urology, Affiliated Changshu Hospital of Nantong University, Jiangsu 215500)
[Abstract]" "Objective: The study investigates the risk factors for the occurrence of systemic inflammatory response syndrome(SIRS) after percutaneous nephrolithotomy(PCNL), aiming to provide reference for the development of strategies to prevent and treat SIRS. Methods: A retrospective analysis was conducted on the clinical data of 97 patients who underwent PCNL at the Affiliated Changshu Hospital of Nantong University from January 2019 to December 2020. The patients were divided into SIRS group and non-SIRS group based on the presence or absence of SIRS after surgery. The differences in gender, age, BMI, hypertension, diabetes, preoperative WBC count, perirenal fat stranding(PFS), stone size, surgical approach, and operative time were compared between the two groups. Multivariate Logistic regression analysis was employed to identify the risk factors for the occurrence of SIRS. Results: The two groups showed no statistically significant differences in terms of gender, age, BMI, hypertension, diabetes, stone size, surgical approach, and operative time(all Pgt;0.05). However, there were statistically significant differences in preoperative WBC count and PFS between the two groups(Plt;0.05). Multivariate Logistic regression analysis, incorporating BMI, diabetes, preoperative WBC count, PFS, surgical approach, and operative time, revealed that a positive preoperative WBC count and the presence of PFS were independent risk factors for the occurrence of SIRS(Plt;0.05). Conclusion: The occurrence of SIRS after PCNL is correlated with preoperative positive WBC count and the presence of PFS. Focusing on preoperative WBC count and PFS, providing adequate antimicrobial treatment when necessary may be an important measure to reduce the occurrence of SIRS.
[Key words]" "systemic inflammatory response syndrome; percutaneous nephrolithotomy; perirenal fat stranding; risk factors
上尿路结石是泌尿外科常见病,经皮肾镜取石术(percutaneous nephrolithotomy, PCNL)是治疗上尿路结石的最重要方法之一[1-2],但PCNL术后发生尿脓毒血症等并发症比其他泌尿外科手术更常见的事实也不容忽视[3]。由于尿脓毒血症的初始阶段往往缺乏典型的症状,这使临床上很难在早期识别其发生而延误治疗[4],可能发展成危及生命的败血症,即使在后期加强治疗,也很难获得良好的效果[5]。因此,在临床工作中,尽量避免并及早发现尿脓毒血症至关重要。
有学者[6]建立PCNL术后全身炎症反应综合征(systemic inflammatory response syndrome, SIRS)与早期尿脓毒血症关系的临床风险预测模型,发现SIRS是PCNL术后是否发生尿脓毒血症较为敏感的指标。据文献[7-8]报道,PCNL术后发生SIRS的诱因众多,与术前感染的不良控制、术中肾盂压力过高、双J管引流不畅等因素有关。近年来,南通大学附属常熟医院采用PCNL治疗上尿路结石的过程中,尽量避免上述危险因素,但SIRS仍时有发生,在一定程度上增加了医疗负担。故本文回顾性分析PCNL术后发生SIRS患者的临床资料,探寻其他可能的危险因素,旨在为制订防治SIRS发生的方案提供参考。
1" "资料与方法
1.1" "临床资料" "回顾性分析2019年1月—2020年12月于南通大学附属常熟医院行PCNL患者的临床资料纳入标准:(1)上尿路结石行PCNL手术;(2)由同一团队医师手术。排除标准:(1)临床资料不全;(2)功能或解剖性孤立肾;(3)有肾脏手术史或多通道PCNL手术史。有111例患者纳入研究,排除14例,其中临床资料不全4例,功能或解剖性孤立肾4例,有肾脏手术史或多通道PCNL手术史6例。最终共97例进入回顾性分析,其中男60例,女37例,年龄18~79岁,平均(54.4±12.41)岁,BMI为17~35 kg/m2,高血压病32例,糖尿病10例。所有患者肾功能正常或接近正常。
诊疗原则根据《中国泌尿外科和男科疾病诊断治疗指南:2019版》[9]。研究遵循的程序符合2013年修订的《世界医学协会赫尔辛基宣言》要求。本研究获得南通大学附属常熟医院伦理委员会批准(伦理号:2016027)。所有患者均签署手术知情同意书。
1.2" "术前准备" "常规检查尿常规和尿细菌培养。尿细菌培养阳性,根据药物敏感试验结果给予抗感染治疗,待尿培养转阴后手术。尿细菌培养阴性(尿常规WBC阴性或阳性),术前30 min静脉滴注抗生素(第二代头孢菌素类或喹诺酮类药物)。
1.3" "手术方式" "麻醉成功后,患者取斜仰卧位,16~22 Fr的取石通道,钬激光(能量:1.5~2.0 J,频率:10~20 Hz)或混合动力碎石清石系统(EMS,瑞士)(能量:3.0~3.5 J,频率:10~20 Hz)碎石取石。具体手术步骤见参考文献[10-12]。
1.4" "术后治疗" "术后常规卧床休息、监测生命体征等对症支持治疗。常规使用与术前相同的抗生素;如有SIRS发生,行血液细菌培养等相关检查,必要时更换抗生素。根据术后是否出现SIRS,分为SIRS组和非SIRS组。SIRS的诊断标准[13]:(1)体温>38 ℃或<36 ℃;(2)心率>90次/min;(3)呼吸>20次/min或存在过度通气,动脉血二氧化碳分压<4.3 kPa;(4)WBC计数>12×109/L或<4×109/L,或未成熟的WBC>10%。
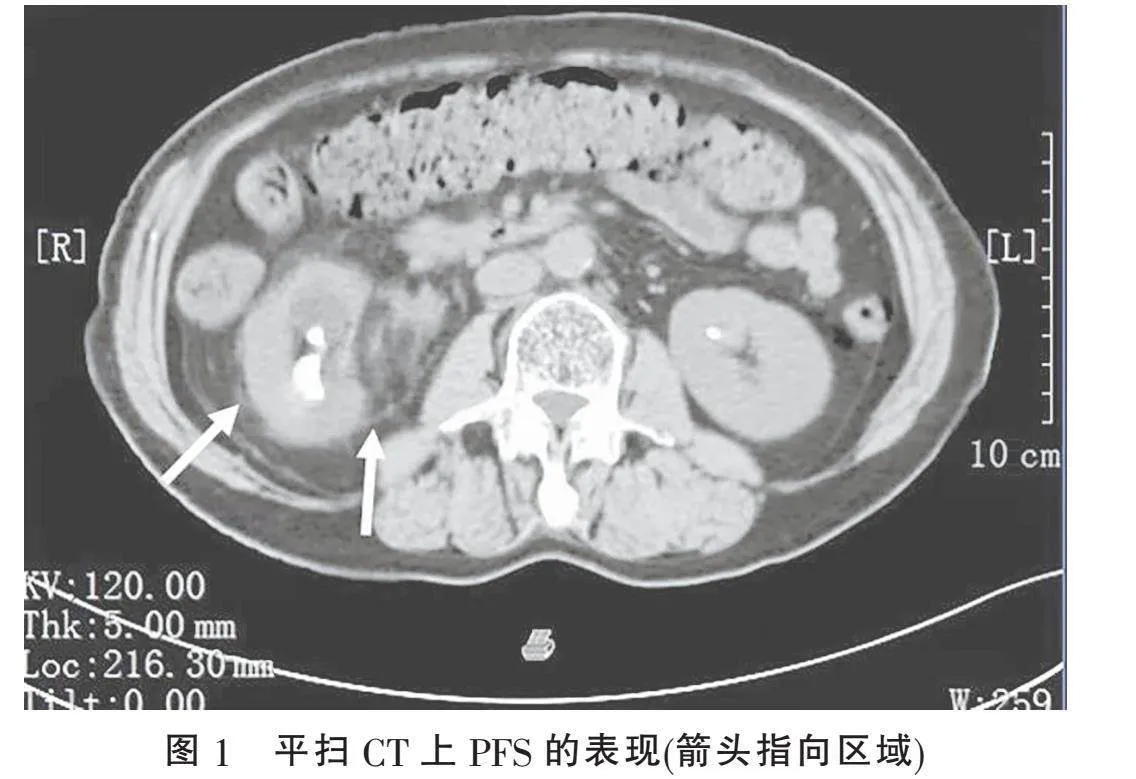
1.5" "观察指标" "收集97例患者性别、年龄、BMI、高血压病、糖尿病、术前尿WBC、肾周脂肪条索影(perirenal fat stranding, PFS)、结石长径、手术通道、手术时间的临床资料并进行统计分析。PFS被定义为平扫CT中肾周脂肪组织间隙内出现软组织条索影[10],均由同一位放射科医师对CT影像进行评估是否为PFS(图1)。
1.6" "统计学方法" "采用SPSS 27.0统计软件包处理数据。正态分布的计量资料以±s表示,简单关联性分析用t检验;偏态分布的计量资料以M(P25, P75)表示,简单关联性分析用秩和检验;计数资料以百分比表示,采用简单关联性分析χ2检验;当T<5时,采用Fisher确切概率法。使用多因素Logistic回归分析SIRS发生的危险因素。以P<0.05为差异有统计学意义。
2" "结" " " 果
2.1" "两组临床资料单因素分析" "97例均顺利完成手术,SIRS组22例(其中尿脓毒血症4例),非SIRS组75例。两组患者性别、年龄、BMI、高血压病、糖尿病、结石长径、手术通道、手术时间差异均无统计学意义(均P>0.05);术前尿WBC、PFS差异有统计学意义(P<0.05)(表1)。
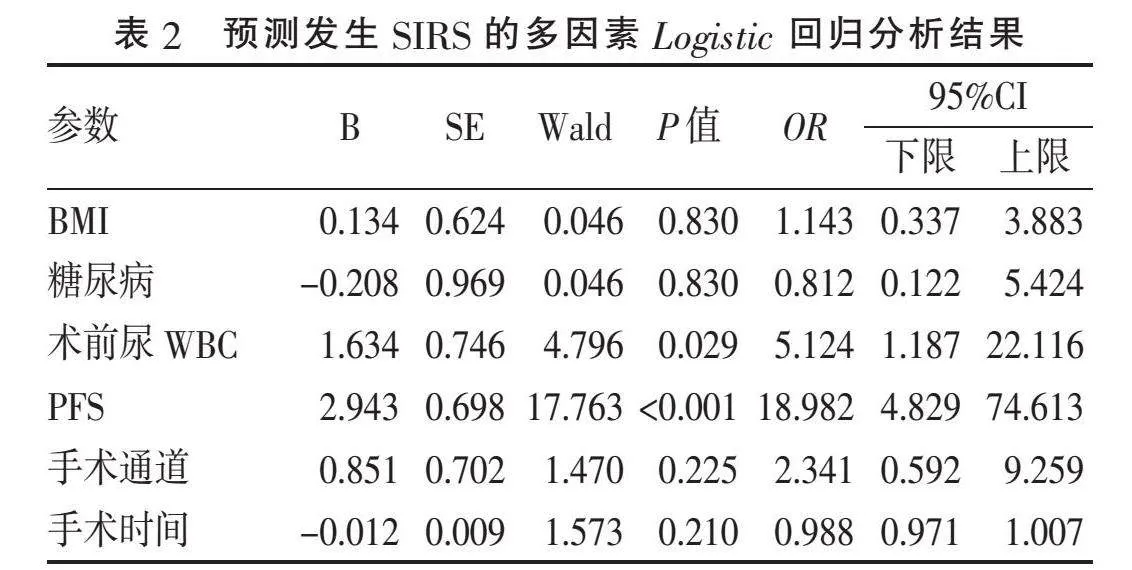
2.2" "多因素Logistic回归分析" "纳入BMI、糖尿病、术前尿WBC、PFS、手术通道和手术时间行多因素Logistic回归分析显示,术前尿WBC阳性、PFS是SIRS发生的独立危险因素(表2)。
3" "讨" " " 论
PCNL以其最高结石排净率的优势,在上尿路结石治疗中占有重要地位,但其可能导致严重的感染、大出血等危及患者生命的风险不容忽视[13, 15]。有学者[6]发现,PCNL术后SIRS和尿脓毒血症之间密切关联,SIRS是较好地鉴别是否感染的依据。文献[16]报道,诱发PCNL术后感染的因素众多。本研究将患者围术期常见的、易获取的指标进行单因素差异分析,发现性别、年龄、BMI、高血压病、糖尿病、结石长径、手术通道和手术时间是否发生SIRS差异无统计学意义;而术前尿WBC、PFS与是否发生SIRS差异有统计学意义。因为理论上性别、年龄、高血压病是SIRS发生诱因的可能性小,加之结石长径可能是手术时间的混杂因素,本研究仅将BMI、糖尿病、术前尿WBC、PFS、手术通道和手术时间纳入多因素Logistic回归分析。结果显示,术前尿WBC阳性、PFS是PCNL术后发生SIRS发生的独立危险因素。
术前尿WBC阳性和PCNL术后发生SIRS密切相关。尿WBC阳性一定程度反映尿路感染的存在,与术后发生SIRS、尿脓毒血症风险密切相关,尿WBC阳性增加了术后感染的风险3~10倍[17-18]。文献[19]报道PCNL感染的风险很高,对于尿培养阴性、尿WBC阳性患者使用抗生素预防措施可显著降低感染的风险,且单次剂量就能达到预防作用。但本研究数据表明,对于尿培养阴性患者,PCNL术前仅给予二代头孢菌素或喹诺酮类药物单剂抗感染,术后尿WBC阳性比尿WBC阴性患者发生SIRS的比例要高。提示加强术前尿WBC阳性患者的抗感染对于预防术后PCNL的感染是必要的。
PFS和PCNL术后发生SIRS密切相关。PFS是由于尿液外渗到肾周间隙导致肾周脂肪组织肿胀,而产生的线状致密改变,平扫CT可以有效识别PFS[20]。有报道[21-22]尿路感染患者PFS的检出率为29.1%~72%。PFS是泌尿系统急性或慢性感染的证据之一,提示肾脏存在隐匿感染[15]。CT提示PFS的患者应在术后密切监测发热、尿路感染和尿脓毒血症的发生[10]。术者对上尿路结石患者是否伴有尿路感染的判断依据多为尿常规、尿培养和血常规等,如上述指标无明显异常,可能忽视隐匿的泌尿系感染而行PCNL手术,从而诱发SIRS。本研究发现,PFS是SIRS发生的独立危险因素,但将PFS用于PCNL术后是否发生SIRS的评估,尚未见报道。因此,术前关注患者的肾CT检查,必要时给予足够的抗感染治疗,可能会减少PCNL术后SIRS发生的概率。
研究的局限性:样本量较少,不能很好地反映群体;为单中心研究,代表性不够强,希望以后通过多中心、前瞻性研究,进一步寻找PCNL术后患者发生SIRS的诱因。
[参考文献]
[1]" "TAILLY T, TSATURYAN A, EMILIANI E, et al. Worldwide practice patterns of percutaneous nephrolithotomy[J]. World J Urol, 2022, 40(8):2091-2098.
[2]" "陈远波, 张志甫, 陆剑君, 等. 3D可视化经皮肾穿刺规划及术中辅助定位引导PCNL的应用[J]. 临床泌尿外科杂志, 2021, 36(12):965-969.
[3]" "KNOLL T, DAELS F, DESAI J, et al. Percutaneous nephrolithotomy: technique[J]. World J Urol, 2017, 35(9):1361-1368.
[4]" "WOLLIN D A, PREMINGER G M. Percutaneous nephrolithotomy: complications and how to deal with them[J]. Urolithiasis, 2018, 46(1):87-97.
[5]" "FONT M D, THYAGARAJAN B, KHANNA A K. Sepsis and septic shock-basics of diagnosis, pathophysiology and clinical decision making[J]. Med Clin North Am, 2020, 104(4):573-585.
[6]" "TANG Y M, ZHANG C, MO C Q, et al. Predictive model for systemic infection after percutaneous nephrolithotomy and related factors analysis[J]. Front Surg, 2021, 8:696463.
[7]" "OSMAN Y, ELSHAL A M, ELAWDY M M, et al. Stone culture retrieved during percutaneous nephrolithotomy: is it clinically relevant?[J]. Urolithiasis, 2016, 44(4):327-332.
[8]" "OMAR M, NOBLE M, SIVALINGAM S, et al. Systemic inflammatory response syndrome after percutaneous nephrolithotomy: a randomized single-blind clinical trial evaluating the impact of irrigation pressure[J]. J Urol, 2016, 196(1):109-114.
[9]" "黄健. 中国泌尿外科和男科疾病诊断治疗指南: 2019版[M]. 北京: 科学出版社, 2020:237-267.
[10]" "付振宇, 孙利国, 马俊, 等. 斜仰卧位经皮肾镜取石术治疗上尿路结石临床疗效分析[J]. 中国临床医学, 2016, 23(6):805-807.
[11]" "付振宇, 孙利国, 张鸽, 等. 斜仰卧位经皮肾镜取石术在马蹄肾多发肾结石中的应用(附8例报道)[J]. 安徽医学, 2018, 39(4):428-430.
[12]" "GU Y F, CHEN Y C, ZHAO Y, et al. Analysis of the risk factors for massive hemorrhage after PCNL in the oblique supine position[J]. Arch Esp Urol, 2023, 76(9):696-702.
[13]" "QIU X, LEI Y P, ZHOU R X. SIRS, SOFA, qSOFA, and NEWS in the diagnosis of sepsis and prediction of adverse outcomes: a systematic review and meta-analysis[J]. Expert Rev Anti Infect Ther, 2023, 21(8):891-900.
[14]" "DEMIRELLI E, ?魻■REDEN E, BAYRAKTAR C, et al. The effect of perirenal fat stranding on infectious complications after ureterorenoscopy in patients with ureteral calculi[J]. Asian J Urol, 2022, 9(3):307-312.
[15]" "SIERRA-DIAZ E, D?魣VILA-RADILLA F, ESPEJO-V?魣-ZQUEZ A, et al. Incidence of fever and bleeding after percutaneous nephrolithotomy: a prospective cohort study[J]. Cir Cir, 2022, 90(1):57-63.
[16]" "ABOURBIH S, ALSYOUF M, YEO A, et al. Renal pelvic pressure in percutaneous nephrolithotomy: the effect of multiple tracts[J]. J Endourol, 2017, 31(10):1079-1083.
[17]" "CHEN D, JIANG C H, LIANG X F, et al. Early and rapid prediction of postoperative infections following percutaneous nephrolithotomy in patients with complex kidney stones[J]. BJU Int, 2019, 123(6):1041-1047.
[18]" "MA Y C, JIAN Z Y, LI H, et al. Preoperative urine nitrite versus urine culture for predicting postoperative fever following flexible ureteroscopic lithotripsy: a propensity scorematching analysis[J]. World J Urol, 2021, 39(3):897-905.
[19]" "XU P, ZHANG S K, ZHANG Y Y, et al. Enhanced antibiotic treatment based on positive urine dipstick infection test before percutaneous nephrolithotomy did not prevent postoperative infection in patients with negative urine culture[J]. J Endourol, 2021, 35(12):1743-1749.
[20]" "HILLER N, BERKOVITZ N, LUBASHEVSKY N, et al. The relationship between ureteral stone characteristics and secondary signs in renal colic[J]. Clin Imaging, 2012, 36(6):768-772.
[21]" "YANO T, TAKADA T, FUJIISHI R, et al. Usefulness of computed tomography in the diagnosis of acute pyelo-nephritis in older patients suspected of infection with unknown focus[J]. Acta Radiol, 2022, 63(2):268-277.
[22]" "YU T Y, KIM H R, HWANG K E, et al. Computed tomography findings associated with bacteremia in adult patients with a urinary tract infection[J]. Eur J Clin Microbiol Infect Dis, 2016, 35(11):1883-1887.
[收稿日期] 2024-01-03