阿仑膦酸钠维D3片对骨质疏松合并股骨颈骨折患者髋关节置换术后假体周围骨密度及骨代谢指标的影响
曾涛 何浓 熊福生


摘要:目的 探讨阿仑膦酸钠维D3片对骨质疏松合并股骨颈骨折患者髋关节置换术后假体周围骨密度及骨代谢指标的影响。方法 选取2021年3月-2022年11月川北医学院附属遂宁市中医院收治的50例骨质疏松症合并股骨颈骨折患者作为研究对象,利用随机数字表法分为试验组及对照组,各25例。对照组术后给予碳酸钙D3片治疗,试验组在其基础上给予阿仑膦酸钠维D3片治疗,比较两组患侧股骨粗隆骨密度、血清骨钙素、Ⅰ型前胶原N-端前肽及骨特异性碱性磷酸酶水平及不良反应发生率。结果 试验组治疗后6个月股骨粗隆骨密度高于对照组(P<0.05);试验组治疗后6个月血清骨钙素、Ⅰ型前胶原N-端前肽及血清骨特异性碱性磷酸酶水平低于对照组(P<0.05);两组不良反应发生率比较,差异无统计学意义(P>0.05)。结论 阿仑膦酸钠维D3片能够调节骨代谢,有效预防因骨质疏松性股骨颈骨折而行髋关节置换术患者术后假体周围骨量丢失,且应用安全性高。
关键词:阿仑膦酸钠维D3片;骨质疏松症;股骨颈骨折;髋关节置换术;骨代谢标志物;骨密度
中图分类号:R683 文献标识码:A DOI:10.3969/j.issn.1006-1959.2024.11.018
文章编号:1006-1959(2024)11-0098-04
Effect of Alendronate Sodium and Vitamin D3 Tablets on Periprosthetic Bone Mineral Density
and Bone Metabolism Indexes in Patients with Osteoporosis Complicated
with Femoral Neck Fracture After Hip Replacement
Abstract:Objective To investigate the effects of alendronate sodium and vitamin D3 tablets on periprosthetic bone mineral density and bone metabolism indexes in patients with osteoporosis and femoral neck fracture after hip replacement.Methods A total of 50 patients with osteoporosis complicated with femoral neck fracture admitted to Suining Hospital of Traditional Chinese Medicine Affiliated to North Sichuan Medical College from March 2021 to November 2022 were selected as the research objects. They were divided into experimental group and control group by random number table method, with 25 patients in each group. The control group was treated with calcium carbonate D3 tablets after operation, and the experimental group was treated with alendronate sodium vitamin D3 tablets on the basis of the control group. The femoral trochanter bone mineral density, serum osteocalcin, procollagen type I N-terminal propeptide, bone-specific alkaline phosphatase levels and incidence of adverse reactions were compared between the two groups.Results The bone mineral density of femoral trochanter in the experimental group was higher than that in the control group at 6 months after treatment (P<0.05). The levels of serum osteocalcin, type I procollagen N-terminal propeptide and serum bone-specific alkaline phosphatase in the experimental group were lower than those in the control group at 6 months after treatment (P<0.05). There was no significant difference in the incidence of adverse reactions between the two groups (P>0.05).Conclusion Alendronate sodium and vitamin D3 tablets can regulate bone metabolism, effectively prevent periprosthetic bone loss in patients undergoing hip replacement due to prevention of osteoporotic femoral neck fracture, and have high application safety.
Key words:Alendronate sodium and vitamin D3 tablets;Osteoporosis;Femoral neck fracture;Hip replacement;Bone metabolism markers;Bone mineral density
近年来随着社会人口老龄化进程不断加快,骨质疏松症的发病率明显增加,骨质疏松症合并股骨颈骨折患者的数量亦明显增加[1]。人工髋关节置换术能够重建髋关节功能,减轻髋部疼痛,明显提高患者生活质量[2]。但是由于假体弹性模量高于人类骨骼,可产生应力遮挡,加速假体周围骨质流失,而且骨质疏松症患者破骨细胞活性明显增强,骨重建失衡,可进一步造成假体周围骨量减少,最终减少假体寿命[3]。因此,如何预防髋关节置换术后假体骨量减少是临床上降低假体置换术后并发症并改善患者术后生活质量急需解决的关键问题。阿仑膦酸钠维生素D3片是临床上常用于抗骨质吸收的药物,其治疗骨质疏松症的疗效确切[4],但是关于该药用于骨质疏松症患者髋关节置换术后的报道较少。本研究旨在探讨阿仑膦酸钠维生素D3片对骨质疏松性人工髋关节置换术后假体周围骨密度、血清骨钙素(osteocalcin, OC)、血清Ⅰ型前胶原N-端前肽(procollagen type ⅠN-peptide, PⅠNP)以及血清骨特异性碱性磷酸酶(bone-specific alkaline phosphatase, BALP)的影响,以期为临床相关治疗决策提供参考。
1资料与方法
1.1一般资料 将2021年3月-2022年11月川北医学院附属遂宁市中医医院收治的50例骨质疏松症合并股骨颈骨折的患者作为研究对象,利用随机数字表法分为试验组与对照组,每组25例。纳入标准:①年龄大于或者等于65岁,性别不限;②X线片诊断为股骨颈骨折,分型为GardenⅢ~Ⅳ型;③符合《原发性骨质疏松症诊疗指南(2017)》[5]中骨质疏松症的诊断标准;④初次行人工髋关节置换术。排除标准:①存在感染或其他严重合并病者;②存在髋关节置换术的禁忌证,如高位髋关节脱位伴骨盆骨量严重缺乏、髋外展肌肌力不足;③合并影响骨代谢的其他疾病,如恶性肿瘤、甲状旁腺疾病及肾上腺疾病等;④严重肝肾功能不全者;⑤对双膦酸盐过敏者;⑥合并严重心理、精神疾病且依从性差者。试验组男11例,女14例;年龄65~88岁,平均年龄(72.75±7.57)岁。对照组男9例,女16例;年龄65~77岁,平均年龄(70.00±3.91)岁。两组年龄及性别比较,差异无统计学意义(P>0.05),具有可比性。本研究经本院医学伦理委员会批准进行,患者及家属知情同意并签署知情同意书。
1.2方法 试验组及对照组患者入院后由同一位高级职称医师完成全髋关节置换术,术后给予常规抗凝、止痛治疗。关节置换术后1周,两组均给予钙剂治疗(碳酸钙D3片,惠氏制药有限公司,国药准字H10950029,规格:每片含钙元素600 mg,含维生素D3 125 IU),口服,1片/次,1次/d,持续治疗6个月。试验组在此基础上服用阿仑膦酸钠维D3片治疗(石药集团欧意药业有限公司,国药准字H20110079,规格:每片阿仑膦酸钠维D3片含阿仑膦酸钠70 mg,含维生素D3 2800 IU),1片/次,1次/周,每周一晨起空腹以200 ml白开水送服,服药后30 min内避免平卧,保持站立或者坐立并避免服用其他任何药品或者食物,持续服用6个月。
1.3观察指标 ①假体周围骨密度:分别在治疗前及治疗后6个月采用双能X线骨密度检测仪评估患肢股骨粗隆骨密度;②骨转换指标:分别在治疗前及治疗后3、6个月抽取患者空腹静脉血5 ml,检测血清OC、PINP及BALP;③不良反应事件:记录患者治疗期间所出现的不良反应,并由课题组医师评估及处理。
1.4统计学方法 采用Graphpad Prism 9.0软件对所得数据进行分析,计量资料以(x±s)表示,满足正态分布及方差齐性者组间采用独立样本t检验,组内采用配对t检验;计数资料以[n(%)]表示,采用χ2检验;以P<0.05为差异有统计学意义。
2结果
2.1两组假体周围骨密度比较 试验组治疗后6个月患肢股骨粗隆骨密度高于对照组,差异有统计学意义(P<0.05),见表1。
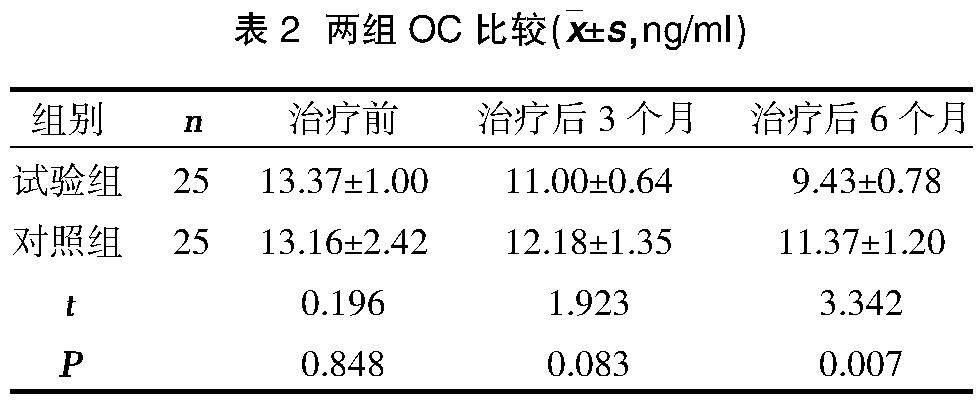
2.2两组OC比较 试验组治疗后3个月血清骨钙素低于对照组,但差异无统计学意义(P>0.05);试验组治疗后6个月血清骨钙素低于对照组,差异有统计学意义(P<0.05),见表2。
2.3两组PINP比较 试验组治疗后3个月PINP低于对照组,但差异无统计学意义(P>0.05);试验组治疗后6个月PINP低于对照组,差异有统计学意义(P<0.05),见表3。
2.4两组BALP比较 试验组治疗后3个月BALP低于对照组,但差异无统计学意义(P>0.05);试验组治疗后6个月BALP低于对照组,差异有统计学意义(P<0.05),见表4。
2.5两组不良反应事件比较 试验组与对照组患者在治疗及随访期间均无严重并发症发生,两组不良反应发生率比较,差异无统计学意义(P>0.05),见表5。
3讨论
原发性骨质疏松症患者由于雌激素缺乏、年龄增长等不可控因素的影响下,导致机体免疫活化,肿瘤坏死因子-α(tumor necrosis factor-α, TNF-α)、白介素-6(interleukin-6, IL-6)等细胞因子浓度增加,从而刺激、促进破骨细胞分化,雌激素缺乏,其对破骨细胞抑制作用减弱,破骨细胞数量增加,骨重建失衡,骨转换率增加,净骨量丢失亦增加[6,7]。在行人工髋关节置换术后,假体将股骨颈中的张力骨小梁及压力骨小梁替代,加之假体弹性模量较高,导致骨盆应力传导发生改变,假体周围骨质呈现失用性骨质疏松表现,其中股骨近端较为明显[8]。上述原因导致骨质疏松症患者行关节置换术后,假体周围骨量丢失风险明显增高,假体植入失败率上升。阿仑膦酸钠是第三代双膦酸盐,具有调节骨重建的作用,能够抑制破骨细胞介导的骨吸收,阻断类异戊二酸合成甲羟戊酸,从而诱导破骨细胞凋亡,抑制其分化、成熟[9]。目前国内外文献均表明[10-12],阿仑膦酸钠能够有效抑制破骨细胞活性,提升骨质疏松症患者中轴骨骨密度。动物试验表明[13],阿仑膦酸钠可以提高新西兰白兔股骨种植物周围骨储备;Morita A等[14]研究发现,阿仑膦酸钠联合特立帕肽能够有效预防植入假体周围骨质丢失,尤其对股骨近端影响显著(Gruen1区及7区)。
本研究结果显示,试验组治疗后6个月患肢股骨粗隆骨密度高于对照组(P<0.05);试验组治疗后6个月血清OC、PINP及BALP水平低于对照组(P<0.05);两组不良反应发生率比较,差异无统计学意义(P>0.05),与既往研究结果一致[15,16]。研究表明[17],阿仑膦酸钠与骨羟基磷灰石具有高亲和力,可特异性结合骨表面进行活骨重塑,抑制破骨细胞功能,降低骨转换。骨重建包含激活、吸收、耦联、形成与矿化过程,其中耦联过程依赖破骨细胞形成吸收陷窝并分泌耦联因子吸引成骨细胞进入吸收陷窝开始类骨质形成及矿化,此过程中OC、PINP、BALP分泌增加[18]。当阿仑膦酸钠抑制破骨细胞活性、降低骨转换时势必影响到骨重建耦联过程,耦联因子减少使得骨形成标志物水平下降[19]。骨转换标志物的下降表明了阿仑膦酸钠维D3片对预防骨质疏松患者髋关节置换术后假体骨量丢失的有效性。此外,本研究过程两组患者均出现腹胀,可能与老年患者胃肠功能较差及服用碳酸钙D3片有关[20],但并未出现严重不良反应,提示运用阿仑膦酸钠维D3片预防骨质疏松患者髋关节置换术后假体骨量丢失是安全的。
综上所述,阿仑膦酸钠维D3片能够有效预防因骨质疏松性股骨颈骨折而行髋关节置换术患者术后假体周围骨量丢失,能够降低患者血清OC、PINP、BALP水平,且治疗期间无严重并发症发生,安全性较高。但因本研究样本量较少,随访时间较短,结论尚需多中心、大样本、前瞻性随机对照试验进一步验证。
参考文献:
[1]Shanb AA,Youssef EF.The impact of adding weight-bearing exercise versus nonweight bearing programs to the medical treatment of elderly patients with osteoporosis[J].J Family Community Med,2014,21(3):176-181.
[2]Yi Z,Bin S,Jing Y,et al.Tranexamic Acid Administration in Primary Total Hip Arthroplasty:A Randomized Controlled Trial of Intravenous Combined with Topical Versus Single-Dose Intravenous Administration[J].J Bone Joint Surg Am,2016,98(12):983-991.
[3]Rahman WA,Amenábar T,Hetaimish BM,et al.Outcome of Revision Total Hip Arthroplasty in Management of Failed Metal-on-Metal Hip Arthroplasty[J].J Arthroplasty,2016,31(11):2559-2563.
[4]王康振,杨健松,张会良,等.骨力胶囊联合阿仑膦酸钠维D3片治疗老年骨质疏松的疗效及对骨代谢标记物及骨强度的影响[J].中国老年学杂志,2018,38(4):864-866.
[5]中华医学会骨质疏松和骨矿盐疾病分会.原发性骨质疏松症诊疗指南(2017)[J].中国骨质疏松杂志,2019,25(3):281-309.
[6]Schulman RC,Weiss AJ,Mechanick JI.Nutrition,bone,and aging: an integrative physiology approach[J].Curr Osteoporos Rep,2011,9(4):184-195.
[7]Feng J,Liu S,Ma S,et al.Protective effects of resveratrol on postmenopausal osteoporosis: regulation of SIRT1-NF-κB signaling pathway[J].Acta Biochim Biophys Sin (Shanghai),2014,46(12):1024-1033.
[8]Venesmaa PK,Kr?ger HP,Miettinen HJ,et al.Monitoring of periprosthetic BMD after uncemented total hip arthroplasty with dual-energy X-ray absorptiometry--a 3-year follow-up study[J].J Bone Miner Res,2001,16(6):1056-1061.
[9]康鹏德,裴福兴,王坤正.假体周围骨溶解发生的细胞、分子生物学机制及早期诊断和药物治疗[J].中华骨科杂志,2008,28(8):684-687.
[10]沈一飞,纪翠芳,李欢,等.阿法骨化醇联合阿伦磷酸钠维D3片治疗老年骨质疏松的临床疗效及其对骨代谢标志物的影响[J].中国老年学杂志,2022,42(11):2710-2712.
[11]Okimoto N,Uemura Y,Yoshioka T,et al.Treatment with once-weekly alendronate oral jelly compared with once-weekly alendronate oral tablet for Japanese patients with primary osteoporosis: An open-label,prospective,observational study[J].Health Sci Rep,2018,2(1):e107.
[12]Shen J,Ke Z,Dong S,et al.Pharmacological Therapies for Osteoporosis: A Bayesian Network Meta-Analysis[J].Med Sci Monit,2022,28:e935491.
[13]von Knoch F,Eckhardt C,Alabre CI,et al.Anabolic effects of bisphosphonates on peri-implant bone stock[J].Biomaterials,2007,28(24):3549-3559.
[14]Morita A,Kobayashi N,Choe H,et al.Effect of switching administration of alendronate after teriparatide for the prevention of BMD loss around the implant after total hip arthroplasty,2-year follow-up: a randomized controlled trial[J].J Orthop Surg Res,2020,15(1):17.
[15]Zhou J,Liu B,Qin MZ,et al.Fall Prevention and Anti-Osteoporosis in Osteopenia Patients of 80 Years of Age and Older: A Randomized Controlled Study[J].Orthop Surg,2020,12(3):890-899.
[16]Khanizadeh F,Rahmani A,Asadollahi K,et al.Combination therapy of curcumin and alendronate modulates bone turnover markers and enhances bone mineral density in postmenopausal women with osteoporosis[J].Arch Endocrinol Metab,2018,62(4):438-445.
[17]Kavanagh KL,Guo K,Dunford JE,et al.The molecular mechanism of nitrogen-containing bisphosphonates as antiosteoporosis drugs[J].Proc Natl Acad Sci U S A,2006,103(20):7829-7834.
[18]Parveen B,Parveen A,Vohora D.Biomarkers of Osteoporosis: An Update[J].Endocr Metab Immune Disord Drug Targets,2019,19(7):895-912.
[19]张炳坤,张喜善.骨代谢标志物在骨质疏松症诊治中的应用[J].中国矫形外科杂志,2022,30(16):1483-1486.
[20]Shane E,Burr D,Abrahamsen B,et al.Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research[J].J Bone Miner Res,2014,29(1):1-23.

