Cardiovascular risk factors affecting COVID-19 outcomes at a tertiary referral hospital in northwest Iran:A prospective cohort study
Mahsa Behnemoon ,Mojdeh Mehrno ,Naser Gharebaghi ,Milad Hamdi
1Department of Cardiology,School of Medicine,Urmia University of Medical Science,Urmia,Iran
2Medical Center,Urmia University of Medical Science,Urmia,Iran
3Department of Dermatology and Infectious Disease,School of Medicine,Urmia University of Medical Science,Urmia,Iran
ABSTRACT Objective: To investigate cardiovascular risk factors affecting COVID-19 outcomes in a tertiary referral hospital.Methods: This prospective cohort study analyzed 269 participants with COVID-19.The primary outcomes were ICU admission,prolonged hospital stay duration,and in-hospital death.The secondary outcomes included death,chronic symptoms,and NYHA functional class during follow-up periods.Results: A total of 412 patients with COVID-19 symptoms were enrolled in the study,and out of which 269 patients had complete medical records and positive SARS-CoV-2 PCR test results,fulfilling the study criteria were analyzed.The patients were divided into two groups,with cardiovascular comorbidities (group A,n=122),such as established cardiovascular disease,diabetes mellitus,and hypertension,and without cardiovascular comorbidities (group B,n=147).Binary logistic regression analysis showed that patients with underlying hypertension,diabetes,and established cardiovascular disease had a 1.55 (95% CI:1.28-2.26),1.62 (95% CI:1.34-2.13),and 1.63 (95% CI:1.07-5.34)-fold risk of mortality,respectively in the adjusted model.Conclusions: Hospitalized COVID-19 patients with predisposing cardiovascular risk factors are more susceptible to develop worse outcomes.More attention should be paid to the management and follow-up of these patients.
KEYWORDS: COVID-19;Outcome;Cardiovascular;Chronic symptoms;Diabetes mellitus;Hypertension
Significance
Little is known about the effects of cardiovascular comorbidities on COVID-19 chronic symptoms and its outcomes.Our study showed that the majority of affected individuals report chronic symptoms,but just the occurrence of chest pain was different between patients with and without cardiovascular risk factors.The most important risk factor increasing in-hospital mortality was established cardiovascular disease such as underlying heart failure and coronary artery disease.
1.Introduction
COVID-19 was a newly diagnosed pneumonia reported to the World Health Organization in December 2019[1].It affects millions of people around the world and remains one of the major medical concerns nowadays[2].Although the number of cases and deaths is decreasing,still some unsolved problems remain in detecting its complications.
COVID-19 affects multiple organs and causes complications such as pneumonia,abnormalities in renal and liver functions,as well as cardiac injuries[3-5].An early study reported that approximately 12% of patients with COVID-19 suffered from underlying cardiac conditions[6].Previous studies found that hospitalized COVID-19 patients with underlying cardiovascular disease may have poorer prognosis compared to other patients[7-9].While most infected people recover and return to their normal lives after a few weeks,some reports show that symptoms may persist even months after recovery from acute illness,especially in patients with underlying cardiovascular comorbidities[10].
Given that COVID-19 patients with underlying cardiovascular disease (CVD) have higher mortality and morbidity[11],and also cardiovascular manifestations are common in severe COVID-19[7],there is a great need to better understand the interactions between COVID-19 and CVDs.Although the acute course and complications of the new coronavirus infection are relatively well understood,little is known about the long-term effects of the disease especially in high-risk groups of patients.Considering all the above-mentioned issues,we conducted this study to describe chronic symptoms and clinical outcomes of COVID-19 patients suffering from underlying cardiovascular comorbidities as compared to the others in a followup period of at least six months.
2.Patients and methods
2.1.Study setting and design
This prospective cohort study was conducted at a referral hospital in the northwest province of Iran between August 1st,and November 30th,2020.
2.2.Ethical approval
The study was conducted in accordance with the principles set forth in the Helsinki Declaration 2008,and approved by the Ethics Committee of Urmia University of Medical Science in January 2020 (approval ID:IR.UMSU.REC.1399.351).In addition,the participants were given a participant information statement and signed a written informed consent form.Individual personal information was kept confidential.
2.3.Inclusion and exclusion criteria
Inclusion criteria were all patients over 18 years old admitted to our tertiary center with COVID-19 symptoms.Exclusion criteria were:mortality before hospital admission at the emergency department,lack of consent to access the patient’s in-hospital and follow-up data,incomplete medical records,and negative SARS-CoV-2 PCR test on arrival.
2.4.Data collection
Patients signed the informed consent form.The subjects were divided into two groups:with cardiovascular comorbidities (group A,n=122) and without cardiovascular comorbidities (group B,n=147) (e.g.congestive heart failure and ischemic heart disease),diabetes mellitus,and hypertension.All participants were treated according to the global health guidelines updated for COVID-19,and medical consults were prescribed based on the patient’s medical circumstances.
Demographic and clinical data were obtained from the patient’s medical records and reviewed by two medical doctors.Baseline characteristics including age,sex,comorbidities,the New York Heart Association (NYHA) functional class,systolic blood pressure,diastolic blood pressure,heart rate,and oxygen saturation were obtained on the first day of admission,and patients were followed for at least 6 months,post-discharge.Information about the presence or absence of any cardiovascular symptoms (e.g.,chronic cough,dyspnea on exertion,chest pain,etc.),as well as the patient’s functional status during follow-up were recorded using telephone calls or serial inperson visits in cases of suspected complications.The follow-up period duration was between 6-12 months.
2.5.Primary and secondary outcomes
The primary outcomes were ICU admission,prolonged hospital stay duration,and in-hospital death.The secondary outcomes included death,chronic symptoms,and NYHA functional class during follow-up periods.
2.6.Statistical analysis
Data were presented as mean±standard deviation,median,frequencies,and percentages wherever applicable.Differences between groups were assessed using independent t-tests for continuous and normally distributed variables and chi-squared test (or Fisher’s exact test) for categorical variables.To evaluate the relationship between baseline variables and in-hospital and followup death,at first,we put each variable in a data set,separately by using univariate analysis.Then we entered all variables with a probable relationship with mortality (P<0.1) into the binary logistic regression model by using a stepwise backward method,in order to demonstrate the prognostic factors of in-hospital and follow-up mortality.The odds ratio (OR) and confidence interval (CI) were calculated for each independent parameter in crude and adjusted model by sex and age,and the P<0.05 was considered statistically significant.All analyses were performed using IBM SPSS software for Windows version 22.
3.Results
A total of 412 patients with COVID-19 symptoms were enrolled in the study.Eighteen cases deceased on arrival before admission to the specific ward.Only 281 patients signed the informed consent form,and out of which 269 patients had completed medical records and positive SARS-CoV-2 PCR test results,fulfilling the study criteria (Figure 1).

Figure 1. The study flowchart.
The mean age of the patients was (55.0±16.1) years and 150 (55.8%) were male.In group A,85 patients (31.6%) had hypertension,45 (16.7%) suffered from diabetes mellitus,and 39 (14.5%) had documented cardiovascular disease (e.g.heart failure or ischemic heart disease).52 Patients died during hospital stay (n=47) and follow-up period (n=5) (Table 1).

Table 1. Baseline demographic and clinical characteristics among the studied COVID-19 patients (n=269).
Patients in Group A were older (61.1±14.3 vs.49.8±15.7,P=0.001) and more likely to be hospitalized in intensive care units (50.0% vs.25.9%,P=0.001).Moreover,they were more likely to be on NYHA functional class 2 or higher during the follow-up period (18.8% vs.14.3%,P=0.031),as well as having a higher rate of inhospital death as compared to the other group (24.6% vs.11.6%,P=0.005).However,there was no significant difference in terms of other baseline characteristics or long-term mortality between the two groups (Table 2).
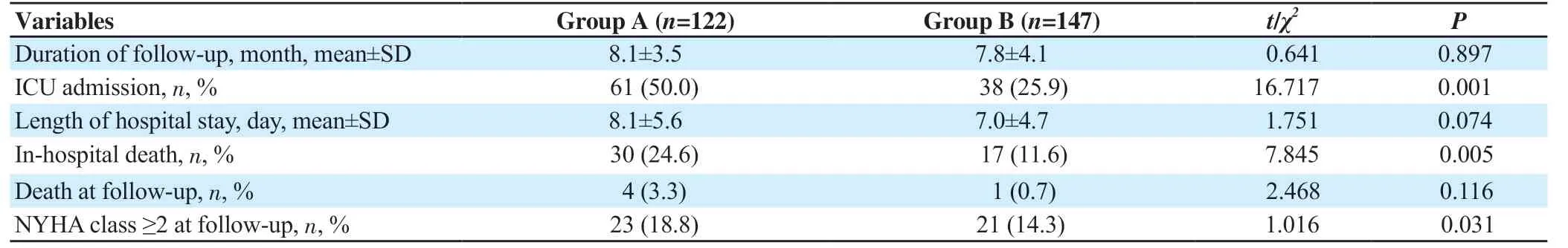
Table 2. Events and outcomes of COVID-19 patients during hospital stay and follow-up (n=269).
As illustrated in Table 3,in group A,patients had a 1.49-fold risk of in-hospital death as compared to the other group.Patients with underlying hypertension,diabetes,and established cardiovascular disease had a 1.55,1.62,and 1.63-fold risk of inhospital death,respectively in the adjusted model (adjusted for age and sex).We followed 217 patients for a mean follow-up period of 9.4 months.5 Patients had major cardiovascular events (2 cerebrovascular accidents,2 myocardial infarctions,and 1 pulmonary emboli).During follow-up,29 (13.4%) participants reported that their underlying diabetes or hypertension was out of control (9 and 8 patients,respectively),or experienced new-onset diabetes or hypertension (7 and 5 patients,respectively).About onethird of subjects (n=70,32.3%) were symptom-free after discharge,and half of the participants (n=110) reported at least one cardiac or non-cardiac symptom lasting for more than one month,which was defined as chronic symptoms.The most common chronic symptoms reported by the participants were cough (38.2%),dyspnea on exertion (29.0%),headache (24.0%),and fatigue (23.5%).Other less reported but important chronic symptoms were myalgia (20.7%),vertigo (15.7%),hair loss (15.7%),chest pain (13.4%),and loss of taste or smell (12.9%),the latter persisting for more than 6 months in two patients (Table 4).There was no significant difference between the two groups of patients in terms of cardiac and non-cardiac symptoms,except for chest pain during follow-up.Patients in group A were more likely to experience episodes of recurrent prolonged chest pains leading to outpatient cardiology visits in order to evaluate its significance during the follow-up period (20.7% vs.8.0%,P=0.017).
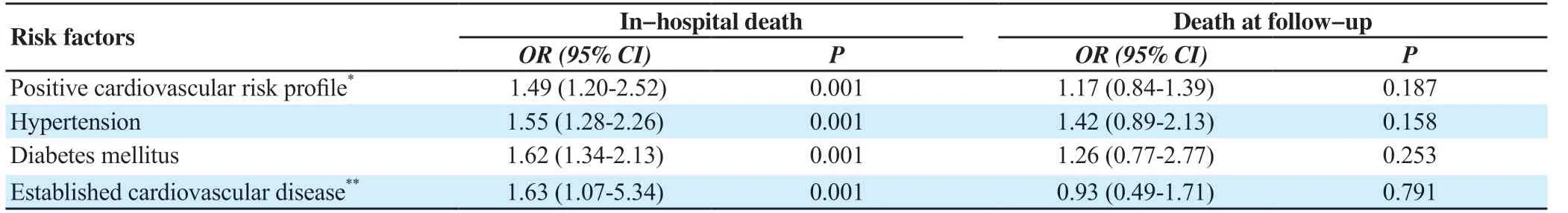
Table 3. Risk factors of mortality by cardiovascular diseases based on adjusted model.
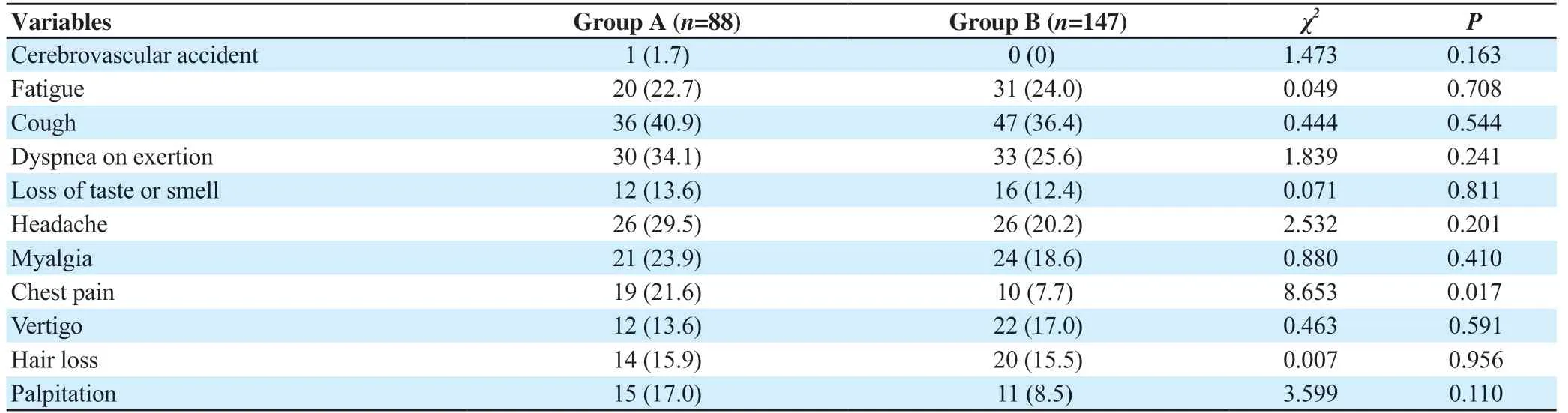
Table 4. Chronic symptoms reported by participants at follow-up (n,%).
4.Discussion
Older patients,and those with pre-existing medical situations (such as CVD,chronic respiratory disease,or diabetes) are reported to be at risk for severe disease from COVID-19[5,6,12-16].According to the present study,patients with a cardiovascular risk profile were more likely to be hospitalized in ICU,have a higher rate of inhospital mortality (OR:1.63,95% CI:1.07-5.34),and experience NYHA class ≥2 during follow-up.Multiple explanations exist for these findings.First,the median age of our patients with underlying cardiovascular disease or its risk factors was 61 years,in line with all other previous studies which showed that older age is crucial in increasing the disease complications.Moreover,the frailty of elderly patients with multi-comorbidities makes them more likely to have worse outcomes[17].A positive cardiovascular risk profile may contribute to increasing mortality in COVID-19 patients,at least in part,because of the consequent hemodynamic deterioration,or weakening of the patient’s immune systems.
In accordance with our observations,prior studies have found that during other viral infections,for instance,influenza epidemics,cardiovascular comorbidities were strongly related to increased mortality.For example,data from the severe H1N1 pandemic in 2009 indicated that elevated troponin and left ventricular dysfunction (ejection fraction <50%) were related to high mortality[18].In an earlier meta-analysis,Sabatino et al.reported that pre-existing cardiovascular comorbidities or risk factors have a significant role in increasing mortality[19].In multiple recent meta-analyses,CVD and its risk factors (hypertension and diabetes) were closely associated with worse outcomes in COVID-19 patients[20-22].
Our findings showed that hypertensive patients are at risk for inhospital death from COVID-19 (OR:1.55,95% CI:1.28-2.26).In line with this result,previous studies suggested that hypertension can serve as a risk factor for worse hospital outcomes in these patients[3,23-25].The exact mechanism of the interaction between hypertension and increased mortality in COVID-19 patients is not clear.However,the dysregulation of the inflammatory and renin-angiotensin system in hypertensive patients may lead to excessive cytokine release,vasoconstriction,cell injury,and worse outcomes[6,26,27].
Diabetes was the second most common comorbidity (after hypertension) observed in our patients,leading to a 1.62-fold risk of in-hospital mortality.In a cohort study of 7 337 COVID-19 patients,suffering from type-2 diabetes was associated with more complex hospitalization,and increased mortality[28].Silverio et al.showed that diabetic COVID-19-affected patients have a higher risk for in-hospital death independent of age,compared to those without diabetes[29].Besides the link between diabetes and atherosclerosis,iatrogenic poor glycemic control in COVID-19 patients may arise from various mechanisms:corticosteroid therapy commonly used in severe infection,hyperglycemia due to the septic status,inadequate glucose monitoring in patients with infection,lack of recommended follow-up and required medical contact on diabetes management,and discontinuation of medications such as angiotensin-converting enzyme inhibitors according to some hospital’s treatment protocols[30].
In our study,about 50% of patients reported that they had at least one cardiac or non-cardiac symptom lasting for more than one month.The most common chronic symptoms reported by participants at follow-up were cough,dyspnea on exertion,headache,and fatigue.In a survey of adults with positive outpatient test results for SARS-CoV-2,20% (1 in 5) reported that some symptoms were prolonged.These persistent symptoms included fatigue,cough,congestion,dyspnea on exertion,loss of taste or smell,headache,myalgia,gastrointestinal symptoms,chest pain,and confusion[31].According to our observations,patients with underlying CVD or its risk factors were more likely to experience episodes of recurrent chest pains leading to outpatient cardiology visits compared to the other group,which could warrant special attention to screening these subjects for probable cardiac complications (e.g.,pericarditis,myocarditis,acute coronary syndrome,pulmonary emboli,etc.) during follow-up.
Several limitations of this study can be addressed.First,our single-hospital experience may not be generalized to the broader community.Second,it is often hard to differentiate between complications caused by comorbidities and possible direct damage caused by COVID-19.However,we used a logistic regression model to overcome this limitation.Third and in particular,our study did not include echocardiographic data and laboratory markers of inflammation,as their application was not routine during the first years of COVID-19 appearance.In addition,analyzing the effects of different treatment methods used during hospitalization was out of the scope of this study,but all the protocols were guided by our infectious disease specialists to achieve more precise data collection.The study size may be small for analyzing different types of underlying cardiovascular comorbidities and future meta-analyses may overcome this limitation.
More attention should be paid to elderly adult patients with underlying CVD who are more susceptible to developing worse outcomes.The underlying CVD may have an independent role in causing death and a worse prognosis.Raising public awareness to reduce the burden of underlying comorbidities,as well as encouraging susceptible patients to comply with protection instructions against COVID-19,are recommended.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors' contributions
MB:conceptualization,methodology,supervision,writing,review and editing.MM:investigation,methodology,validation,data analysis,and data curation.NG:conceptualization,methodology,supervision.MH:methodology,investigation,original draft preparation.
 Journal of Acute Disease2024年1期
Journal of Acute Disease2024年1期
- Journal of Acute Disease的其它文章
- Correlation of neutrophil to lymphocyte ratio to severity of coronary artery disease and in-hospital clinical outcomes in patients with acute coronary syndrome:A prospective observational study
- A 10-year review and epidemiology of animal bite cases in Gerash city,south of Iran:A retrospective cross-sectional study
- Relationship between nutritional therapy and beneficial bacteria ratio in severe disease
- Clinical profile and risk factors of symptomatic and asymptomatic hypoglycemia in neonates admitted to NICU in a tertiary care center:A cross-sectional study
- Acute coalescent mastoiditis in a 16-month-old child due to Streptococcus pneumoniae infection
- Paradoxical systemic toxicity by inhaled paraquat poisoning:A case report
