Relationship between nutritional therapy and beneficial bacteria ratio in severe disease
Kento Nakayama,Hiroyuki Koami,Yuichiro Sakamoto
Advanced Emergency Care Center,Saga University Hospital,Saga 849-0851,Japan
ABSTRACT Objective: To evaluate relationship between changes in the beneficial bacteria in intensive care unit (ICU) patients and nutritional therapy type.Methods: Ten patients aged ≥18 years admitted to the ICU between January and December 2020,were included.Good enteral nutrition was defined as early achievement of target calorie intake through enteral feeding.The ratio of beneficial bacteria at the first and second bowel movements after each patient’s admission was calculated and the patients were classified into the increase or decrease group.Among all patients,five each were in the increase and decrease groups.We investigated patient background,changes in sequential organ failure assessment (SOFA) and acute physiology and chronic health evaluation (APACHE) Ⅱscores,nutritional doses or methods,and clinical outcomes.Results: No relationship was found between changes in the ratio of beneficial bacteria and changes in SOFA/APACHEⅡscores at the time of admission.The rate of good enteral nutrition was significantly higher in the increase group than in the decrease group (4/5 vs.0/5,P=0.01).Conclusions: An increase in beneficial bacteria may be significantly related to the early establishment of enteral nutrition.In the future,accumulating cases may make it possible to establish a new nutritional strategy for critically ill patients from an intestinal microbiota perspective.
KEYWORDS: Beneficial bacteria;Enteral nutrition;Parenteral nutrition;Intensive care unit;Good enteral nutrition;Severe disease;Nutritional therapy
Significance
In our study,no specific strategies for nutritional therapy have been established.However,we observed that good enteral nutrition was significantly higher in the increase group compared to the decrease group.In future accumulating more cases may make it possible to establish a new nutritional strategy for critically ill patients,specifically focusing on the perspective of intestinal microbiota.
1.Introduction
In recent years,the effects of gut microbiota changes have been studied in multiple organs[1-3].In intensive care unit (ICU) patients with systemic inflammatory response syndrome,it has been reported that levels of Bifidobacterium and Lactobacillus decrease in the intestinal flora,and this is associated with the prognosis[4].Although intestinal flora has been reported to be recovered by the combined use of pro-and prebiotics,no specific strategies for nutritional therapy have been established[5].Therefore,we examined the appropriate nutritional therapy by investigating the relationship between nutritional therapy in the ICU and changes in the ratio of beneficial bacteria.
2.Patients and methods
2.1.Study design
This retrospective study was conducted at our hospital between January and December 2020.
2.2.Inclusion and exclusion criteria
Patients aged ≥18 years,who were admitted to the emergency ICU of our hospital and were expected to be hospitalized for >1 week,were included in this study.The exclusion criteria for our study were (1) patients leaving ICU within one week;(2) difficult stool collection;and (3) stool storage method problems.
2.3.Ethical statement
This study was approved by the ethics committee of our hospital (approval number:2020-01-R-08).Written informed consent for participation in the study was obtained from all patients.Patient information was retrospectively extracted from the electronic medical records of our hospital.
2.4.Collection of stool specimens and analysis by terminal restriction fragment length polymorphism (T-RFLP) method
After admission to the hospital,stools from the first and second bowel movements were submitted to Techno Suruga Lab Co.,Ltd.,and the ratio of Bifidobacterium and Lactobacillus levels was investigated using T-RFLP flora analysis (MN method).T-RFLP analysis of microbial community structure in feces was performed by TechnoSuruga Laboratory Co.,Ltd.(Shizuoka,Japan).The amplification of the bacterial 16S rRNA gene (16S rDNA),restriction enzyme digestion,size-fractionation of fluorescentlabeled terminal restriction fragments (T-RFs),and the T-RFLP data analysis was performed as previously described by Nagashima et al.[6].The bacterial 16S rRNA was amplified using the Tks Gflex DNA polymerase (Takara,Japan) and 5’ FAM-labeled 516f and 1510r primers.The polymerase chain reaction product was digested using 5 U of FastDigest BseLⅠ (BslⅠ) (Thermo Fisher Scientific,USA).The resultant DNA fragments,namely,fluorescent-labeled terminal restriction fragments (T-RFs),were analyzed by ABI PRISM 3500xl Genetic Analyzer (Thermo Fisher Scientific),and their length and peak area were determined using the genotyping software GeneMapper (Applied Biosystems,USA).The T-RFs were divided into 29 operational taxonomic units (OTUs).The OTUs were quantified as the percentage of individual OTU per total OTU area,which was expressed as the percentage of the area under the curve.The bacteria were predicted for each classification unit,and the corresponding OTU was identified according to reference Human Fecal Microbiota T-RFLP profiling (https://www.tecsrg.co.jp/services/community-structure-analysis/intraintestinalenvironment/t-rflp-mn1/).A total of 20 specimens from 10 cases were investigated.
2.5.Collection and definition of other data
As a measure of early achievement of nutritional therapy,good enteral nutrition (EN) was defined as the cases in which ≥50% of the target calorie count was achieved within one week by only enteral nutrition,without the use of parenteral nutrition.Among the 10 cases from which stools were collected,the group in which the ratio of beneficial bacteria increased in the second test was defined as the increase group,and that in which the ratio decreased was defined as the decrease group.The extracted data included the patient’s sex and age,medical history,disease-causing hospitalization,sequential organ failure assessment (SOFA) score at admission,acute physiology and chronic health evaluation (APACHE)Ⅱscore,injury severity score,revised trauma score,probability of survival,and details of treatment,such as artificial respirator use,surgical intervention,blood purification therapy,transcatheter arterial embolization,blood transfusion,and antibiotic use.In addition to the above,hospitalization days,length of ICU stay,outcome,changes in the SOFA and APACHEⅡscores,fasting period,parenteral nutrition,frequency of diarrhea,nutritional administration method,and daily nutritional dose were recovered from the health records.
2.6.Statistical analysis
All statistical analyses were performed using JMP Pro Version 14 software package (SAS Inc.,USA).Fisher’s exact test was used for categorical data,and the Wilcoxon rank-sum test was used for continuous data.The normality and distribution of continuous variables were confirmed using the Shapiro-Wilk test.Normally distributed data are expressed as mean values with standard deviation,and non-normally distributed data are expressed as median values with interquartile ranges (IQR).In all analyses,statistical significance was set at P<0.05.
3.Results
3.1.Basic characteristics
In the increase group,the primary cause was trauma (n=3),burn (n=1),and post-cardiac arrest resuscitation (n=1).Meanwhile,in the decrease group,there were two cases of trauma and three cases of burns.The SOFA score at admission was 8±2 and 10±3 in the increase and decrease groups,respectively,whereas the APACHEⅡscore was 20±6 and 18±3 in the increase and decrease groups,respectively (Table 1).
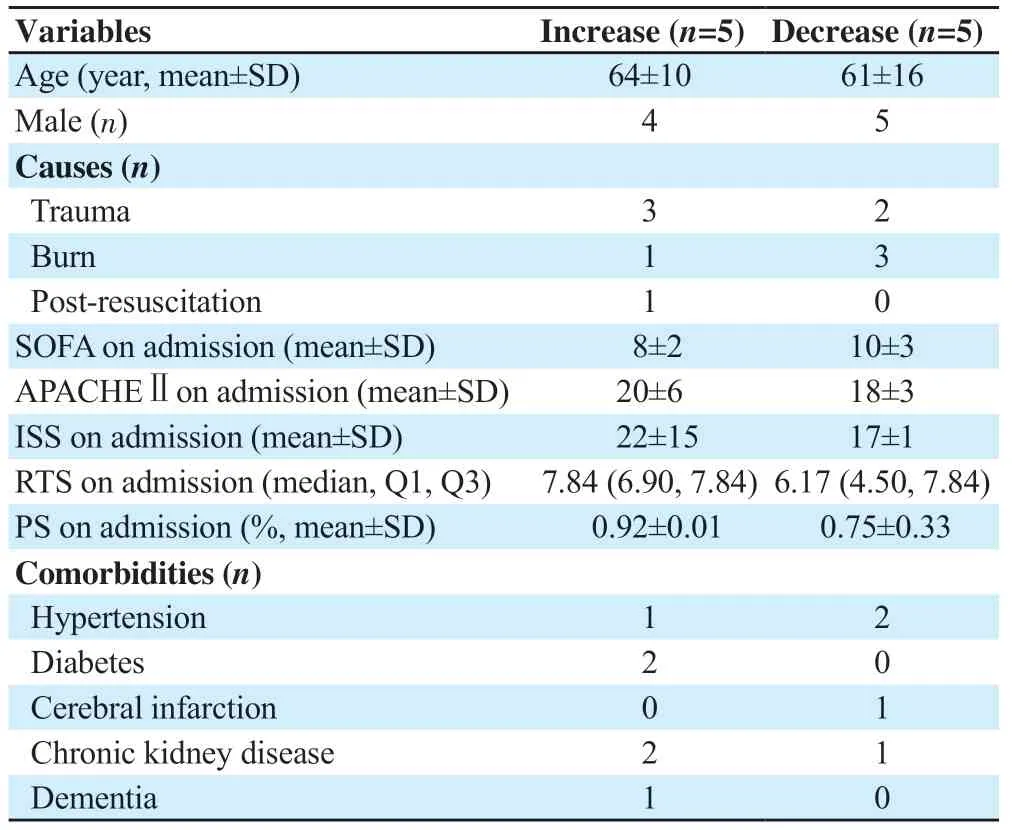
Table 1.Baseline characteristics.
3.2.Treatment and prognosis
Regarding treatment,five cases in the increase and decrease groups received mechanical ventilation (Table 2).Five cases in the decrease group and three cases in the increase group underwent mechanical operation.Four cases in the increase group and two cases in the decrease group received continuous renal replacement therapy.All patients in both groups received antibiotics.Only one case in the decrease group received carbapenem.The length of ICU stay was 30 (14,47) and 18 (18,34) days in the increase and decrease groups,respectively.One patient died in the increase group,and no deaths occurred in the decrease group.
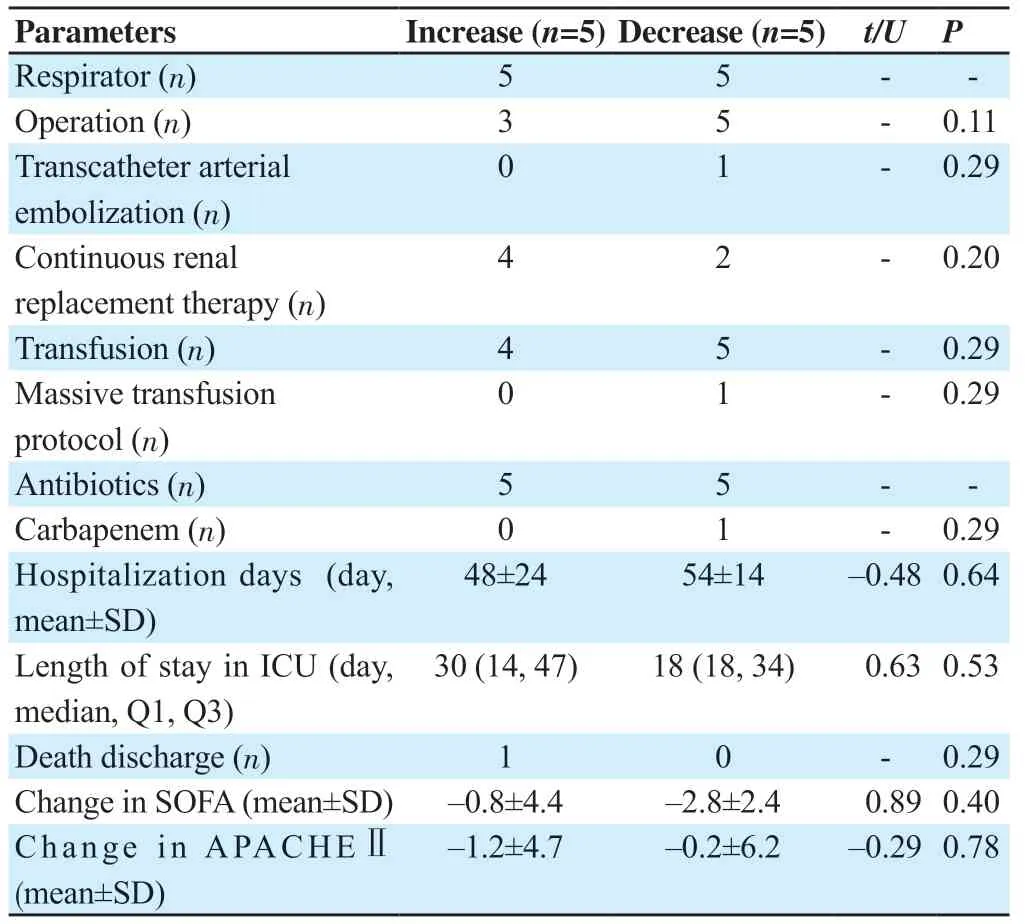
Table 2.Treatment and prognosis.
3.3.Changes in clinical severity scores
The change in the SOFA score at the time of stool collection was–0.8±4.4 and–2.8±2.4 in the increase and decrease groups,respectively (P>0.05).The change in the APACHEⅡscore at the time of stool collection was–1.2±4.7 and–0.2±6.2 in the increase and decrease groups,respectively (P>0.05).No significant difference was observed between the changes in the SOFA and APACHEⅡscores during hospitalization and the ratio of beneficial bacteria.
3.4.Nutrition therapy
The fasting period was 0.8 days (0,2) and 1.4 days (0,3.5) in the increase and decrease groups,respectively (Table 3).The number of patients using total parenteral nutrition was one (20%) and four (80%) in the increase and decrease groups,respectively.The daily caloric intake was 1 200 (580,1 539) and 1 328 (88,1 508) kcal in the increase and decrease groups,respectively.

Table 3.Nutritional therapy and bowel movement.
3.5.Percentage of good EN and good bacteria in hospitals
Good EN was achieved in four and zero cases in the increase and decrease groups,respectively (Table 3).There was a significant difference between both groups in achieving good EN (P=0.01).
4.Discussion
In the present study,we examined the changes in the ratio of beneficial bacteria and its association with nutritional therapy.Factors evaluating nutritional therapy,such as the SOFA/APACHE Ⅱscore at the time of hospital visit and its changes and the content of treatment after hospitalization,were not associated with increases or decreases in the ratio of beneficial bacteria.Ojima et al.reported that,in ICU patients,the proportion of actinobacteria decreased in the carbapenem group[7].In our study,only one patient used carbapenem.Carbapenem use was not associated with increases or decreases in the ratio of beneficial bacteria.Regarding nutritional therapy,there was no relationship between nutritional dose or fasting period and an increase or decrease in beneficial bacteria;however,the rate of good EN was significantly higher in the increase group.
Hayakawa et al.reported a significant decrease in obligate anaerobes and lactobacilli within 6 h of hospitalization in severe disease[8].In our study,it is thought that the ratio of beneficial bacteria had already decreased at the time of the first sampling and that subsequent changes in the ratio of beneficial bacteria may reflect the course of treatment rather than the severity at the time of admission.
Michalsen et al.reported that even if patients with rheumatoid arthritis or fibromyalgia fasted for eight days,no changes were observed in the intestinal flora[9].Although the background diseases were completely different,in our study,no significant difference was observed between the increase and decrease groups during the fasting period.This may be due to the extremely short fasting period in both groups (increase group:0.8 days,decrease group:1.4 days).
In our study,we defined good EN as ≥50% of the target caloric intake within one week without the use of total parenteral nutrition.There seems to be no objection to the fact that the smooth progress of enteral nutrition leads to an increase in the levels of beneficial bacteria.However,there have been cases in which levels of beneficial bacteria decreased despite adequate enteral nutrition.Parenteral nutrition was used in most cases.Chandra et al.reported that changes in intestinal flora may be related to the development of intestinal failure-related liver injury,which is a serious complication of total parenteral nutrition[10].In addition,Hodin et al.reported that total parenteral nutrition reduces the proportion of the Firmicutes phylum,which contains beneficial bacteria[11].Miyasaka et al.reported that administration of total parenteral nutrition in mice led to a move from a Firmicutes-dominant community to a Proteobacteriadominated community which are generally considered not beneficial bacteria[12].There have been no studies on the effect of parenteral nutrition combined with enteral nutrition on intestinal flora.Although the exact mechanism has not been elucidated,the use of parenteral nutrition may be involved in changes in the ratio of beneficial bacteria.Therefore,further investigation is necessary.
Our study had some limitations.The number of samples was very low.Additionally,the number of specimens collected per case was low.Moreover,the timing of sample collection was not uniform for each patient,and it did not necessarily accurately reflect the course of treatment.Background diseases were mixed,including severe trauma,severe burns,and post-cardiopulmonary resuscitation;therefore,the possibility that differences in background diseases affected changes in intestinal flora cannot be ruled out.
In this study,we focused on the ratio of beneficial bacteria;however,it is unclear whether the ratio of beneficial bacteria is a sensitive indicator that reflects the patient’s condition.In addition,it is necessary to consider whether it is appropriate to evaluate the patient’s condition based only on the increase in the ratio of beneficial bacteria,as a quantitative evaluation has not been performed.Accumulation of cases may reveal previously unknown adverse effects of parenteral nutrition.
We evaluated whether changes in beneficial bacteria in the ICU were associated with the type of nutritional therapy.To this end,we investigated the ratio of beneficial bacteria in stool specimens during the hospitalization of patients admitted to the ICU of our hospital.The rate of good EN,defined as enteral nutrition early target calorie achievement,was significantly higher in the group with an increase in the ratio of beneficial bacteria.Thus,an increase in beneficial bacteria may be significantly related to the early establishment of enteral nutrition.Nutritional management centered on enteral nutrition may be desirable from the viewpoint of the intestinal microflora.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors’ contributions
KN,HK,and YS contributed to the concept,design,definition of intellectual content,literature search,clinical studies,experimental studies,data acquisition,data analysis,statistical analysis,manuscript preparation,manuscript editing and manuscript review.All three authors are designated as guarantors.
 Journal of Acute Disease2024年1期
Journal of Acute Disease2024年1期
- Journal of Acute Disease的其它文章
- Cardiovascular risk factors affecting COVID-19 outcomes at a tertiary referral hospital in northwest Iran:A prospective cohort study
- Correlation of neutrophil to lymphocyte ratio to severity of coronary artery disease and in-hospital clinical outcomes in patients with acute coronary syndrome:A prospective observational study
- A 10-year review and epidemiology of animal bite cases in Gerash city,south of Iran:A retrospective cross-sectional study
- Clinical profile and risk factors of symptomatic and asymptomatic hypoglycemia in neonates admitted to NICU in a tertiary care center:A cross-sectional study
- Acute coalescent mastoiditis in a 16-month-old child due to Streptococcus pneumoniae infection
- Paradoxical systemic toxicity by inhaled paraquat poisoning:A case report
