Benign stricture of bilioenteric anastomosis after Whipple with synthetic polypropylene suture
A Michel Devne ,Christine MG Schmmel
a Department of Radiology, Prisma Health Upstate, Greenville, USA
b Department of Pathology, Prisma Health Upstate, Greenville, USA
TotheEditor:
Biliary stricture formation at the bilioenteric anastomosis is an infrequent complication (2%-3%) after pancreaticoduodenectomy;the average presentation is within 13-14 months (range from 1 month to 9 years) after surgery [1,2].While the etiology is unknown,development of biliary stricture has shown to be more likely if a bile leak occurs in the postoperative period [3,4]and with younger patients [5].Furthermore,while the incidence is thought to be the same in patients with benign and malignant diseases,patients with distal cholangiocarcinoma are at higher risk for stricture formation than other periampullary cancers or benign diseases [1].Interestingly,an evaluation of early biliary complications after pancreaticoduodenectomy revealed that 6/0 sutures were associated with biliary stricture;however,this was thought to be more a reflection of the technical difficulties and biliary injury from performing bilioenteric anastomosis on a small common bile duct [2].
Here we report a case of late presentation of a bilioenteric stricture at the site of the bilioenteric anastomosis in a patient 15 years post-pancreaticoduodenectomy,at which a non-absorbing Prolene suture was noted,suggesting a role in the development of the stricture.
A 66-year-old man presented to his primary physician with jaundice 15 years after a Whipple procedure for cholangiocarcinoma.Computed tomography (CT) examination (not shown)demonstrated intrahepatic biliary ductal dilatation with a soft tissue density abnormality in the portal hepatis measuring 4.7×2.5 cm adjacent to the pancreatic anastomosis.As a prior Whipple precluded endoscopic retrograde cholangiopancreatography (ERCP),a percutaneous transhepatic cholangiogram was performed,demonstrating biliary obstruction at the level of the hepatic hilum;an internal/external biliary drainage catheter was inserted.Within three weeks,the patient’s scleral icterus was improved and his urine and stool were of normal color.A percutaneous cholangiogram was performed,demonstrating an indeterminate,benign appearing,smooth,short segment stricture at the anastomosis (Fig.1).Cholangioscopy was performed with SpyGlass DiscoverTM(Boston Scientific,Marlborough,MA,USA),demonstrating no evidence of mass;ProleneTM(Ethicon,Cincinnati,OH,USA) suture was present within a benign-appearing stricture (Fig.2).Eight biopsy specimens of the stricture with SpyBite MaxTM(Boston Scientific) were obtained;the internal/external biliary drainage catheter was increased to 14 French.Cholangioplasty was completed at the bilioenteric anastomosis.Pathology received an aggregate of soft tissue (0.6×0.4×0.1 cm),which was identified as inflamed and artifactually distorted stroma with benign glandular epithelium with no diagnostic malignancy (Fig.3).Post-procedure,the drain was well-tolerated,and at three months,it was capped and removed;six months post-procedure,the patient was reported to be well without any stenting or drainage,with normal liver function tests and no clinical symptoms of biliary obstruction.

Fig.1. Cholangiogram from right ductal approach demonstrating improved bilioenteric anastomotic stricture (white arrow) after cholangioplasty.
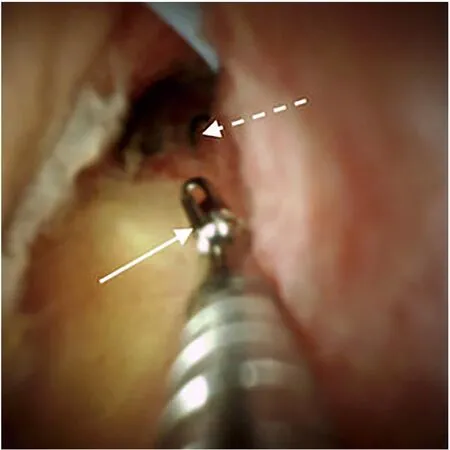
Fig.2. Cholangioscopy with SpyGlass DiscoverTM during biopsy of the stricture with SpyBite MaxTM (white arrow).Prolene suture was identified distal to the biopsy device (broken white arrow).
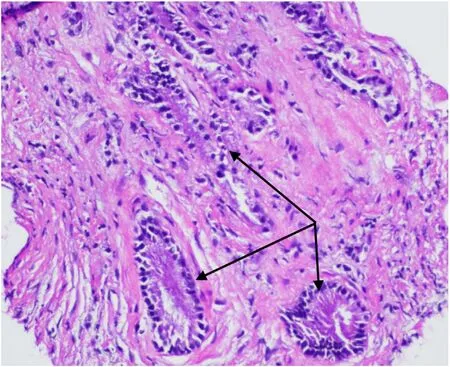
Fig.3. Histology of the stricture illustrating benign biliary epithelial glands (black arrows) surrounded by stroma (pink,hematoxylin and eosin staining) (original magnification×200).
Biliary stricture formation at the bilioenteric anastomosis post-Whipple is an infrequent complication that typically manifests within one year of surgery [1,2].Here we describe a symptomatic biliary stricture in a patient 15 years post-Whipple,the longest interval from Whipple to stricture reported to date,although a postoperative biliary stricture has been reported as late as 15.3 years after surgical repair of a laparoscopic cholecystectomy-related bile duct injury [6].The visualization capability of the SpyGlass Discover was able to identify the benign-appearing stricture and the propylene suture in the inflammatory stroma.This allowed for the removal of the suture along with multiple biopsies of the stricture,which were confirmed by pathology as benign glandular epithelium.
While there are reports exploring the etiology of these post-Whipple strictures,none mentions inflammatory reactions to sutures.
Propylene sutures,ProleneTM,are non-absorbable sterile surgical sutures,which,when present,may act as a foreign body leading to adhesion formation [7].While absolute causality of the suture causing the stricture cannot be shown,the literature suggests that foreign bodies can exacerbate the process of adhesion formation and even obstructions,an already well-known complication often requiring surgical intervention [8,9].In fact,the literature is replete with polypropylene mesh causing adhesions,prompting medical device companies to coat mesh with various substances to reduce the likelihood of adhesion formation [10–12].Currently,absorbable sutures are used to prevent bilioenteric anastomotic strictures.
In the case of our patient,no other pathology was noted to contribute to the stricture,suggesting a role for the suture in stricture formation.
The cholangiographic appearance of the stricture was indeterminate.However,we could better evaluate the stricture with cholangioscopy and perform a directed biopsy,providing a definitive benign diagnosis.This stricture was then treated percutaneously with serial balloon dilatation [13]avoiding the morbidity and mortality associated with a surgical anastomotic revision.
Acknowledgments
None.
CRediT authorship contribution statement
A Michael Devane:Conceptualization,Data curation,Writing–original draft.Christine MG Schammel:Writing– review &editing.
Funding
None.
Ethical approval
This study has obtained institutional review board approval from Health Sciences SC and the need for informed consent was waived.
Competing interest
A Michael Devane has been a paid speaker for Johnson and Johnson and is a consultant with Boston Scientific and Guerbet.Christine MG Schammel has no conflict of interest to declare.
 Hepatobiliary & Pancreatic Diseases International2024年1期
Hepatobiliary & Pancreatic Diseases International2024年1期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Pre-MASLD: Should it be defined separately?
- Comment on “Robotic surgery and liver transplantation: A single-center experience of 501 robotic donor hepatectomies”
- Pancreatic panniculitis as the first presentation of pancreatic ductal adenocarcinoma
- A robust genomic-based prognostic model for the assessment of cancer stemness and survival for patients with hepatocellular carcinoma
- Endoscopic hemostasis using self-expandable metal stent combined with PuraStat ® for patient with high risk of post-endoscopic sphincterotomy bleeding (with video)
- Post-fontan circulation hepatocellular carcinoma: Open and laparoscopic hepatectomy
