Post-fontan circulation hepatocellular carcinoma: Open and laparoscopic hepatectomy
Krin KY Ho ,Wong Hoi She ,∗ ,Simon HY Tsng ,Kevin S Lo ,Tn To Cheung
a Department of Surgery, The University of Hong Kong, 102 Pok Fu Lam Road, Hong Kong, China
b Department of Anaesthesiology, Queen Mary Hospital, 102 Pok Fu Lam Road, Hong Kong, China
TotheEditor:
Fontan-associated liver disease shows increasing incidence as advances in pediatric cardiology have prolonged life expectancy in patients with single ventricle congenital heart defects [1].Their unique physiology and procedure-related sequelae present an increasingly relevant challenge in hepatic surgery.We hereby reported a series of patients suffering from hepatocellular carcinoma(HCC) who successfully underwent open and laparoscopic hepatectomy,and highlighted points on strategies to mitigate the surgical and anesthetic risks in this population.
The Fontan procedure is a palliative strategy for cardiac malformations with a single functional ventricle system.The congenital anomaly is characterised by systemic and pulmonary circulations being connected in series,causing mixing of deoxygenated and oxygenated blood in the single ventricle,and a pulmonary circulation maintained by passive flow through an elevated central venous pressure (CVP).The procedure has improved the life expectancy of such patients,with near normalization of arterial saturation and less fluid overload through connection of the systemic venous circulation directly to pulmonary arteries.
However,it is disadvantaged by an elevated CVP that gives rise to chronic congestive liver and associated complications of liver fibrosis and cirrhosis– Fontan-associated liver disease (FALD)–and ultimately HCC [2].Indeed,high CVP and severe atrioventricular valve regurgitation have been shown to be predictors of post-Fontan HCC in the long term [3].These patients are therefore of relevance with rising incidence of Fontan-associated HCC.A recent systematic review of 65 biopsy-proven HCC showed that HCC almost invariably develops ten years after Fontan procedure [4].
We present two patients both with history of Fontan procedure who successfully underwent open and laparoscopic hepatectomy respectively.Their demographics and clinical information were summarized in Table 1.
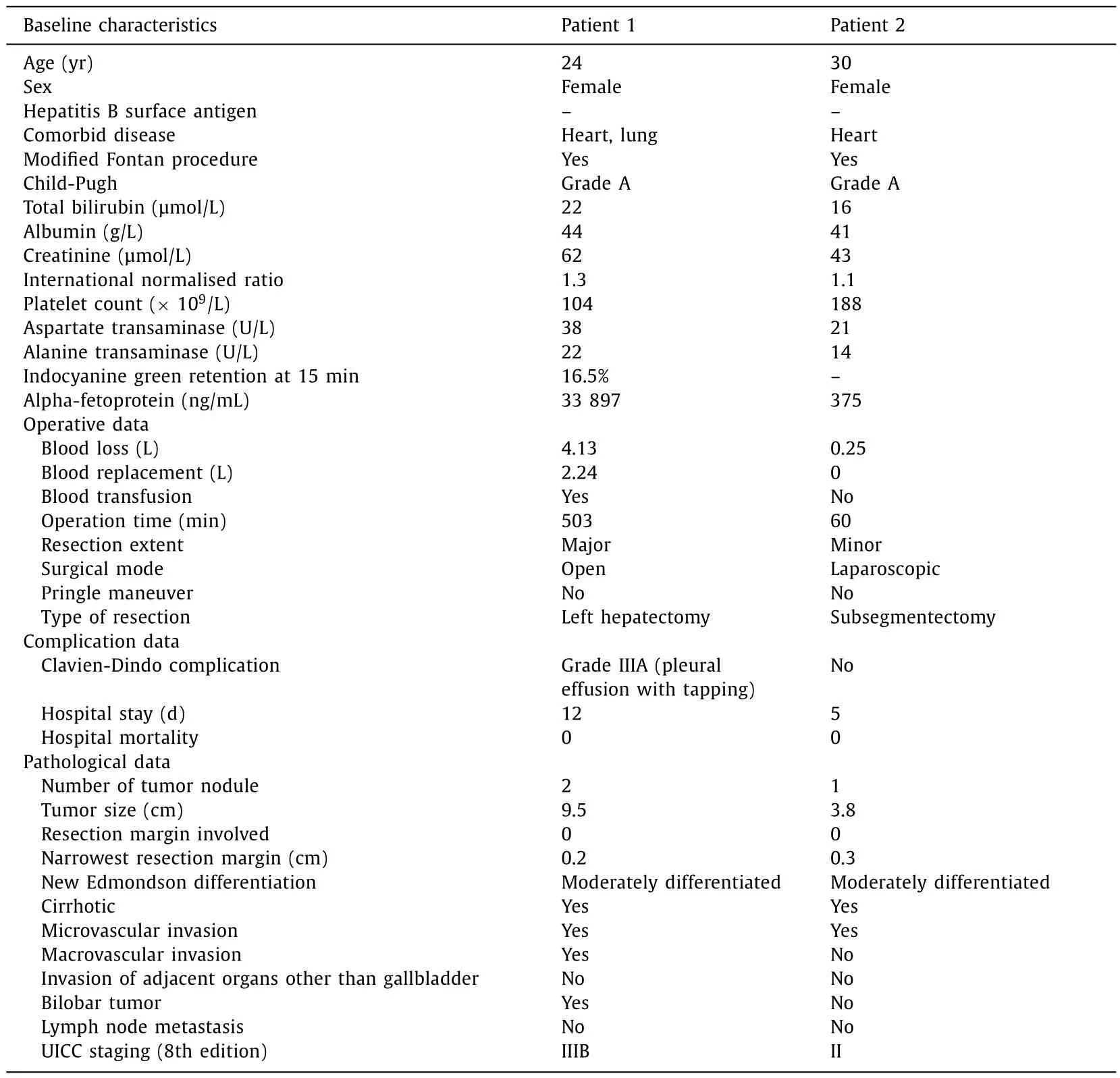
Table 1Summary of data regarding two patients with Fontan circulation who underwent open and laparoscopic hepatectomy.
The first patient was born with tricuspid atresia,pulmonary atresia and patent ductus arteriosus,and underwent modified Fontan procedure and patent ductus arteriosus ligation in her first year of life.At 24 years of age,she underwent open left hepatectomy post-Fontan for a lobulated HCC measuring 6.8×6.6×5.1 cm (Fig.1).Intraoperatively,very strong middle and right hepatic vein flow was encountered.Test clamping of inflow was first used,showing no fluctuation of blood pressure.We then proceeded with clamping of the inferior vena cava to mitigate bleeding.Total intraoperative blood loss was 4 liters with 2 liters of blood replacement.The procedure was otherwise uneventful,and pathological examination revealed 9.5 cm moderately differentiated HCC with resection margin clear by 2 mm.Postoperative period was complicated by right-sided pleural effusion requiring percutaneous drainage.She was otherwise well and discharged home on postoperative day 12.

Fig.1. Arterial (A) and portovenous (B) phase images of contrast computer tomography scan of a patient with Fontan circulation showing hepatocellular carcinoma measuring 6.8×6.6×5.1 cm.
She subsequently received additional postoperative transarterial chemoembolization (TACE) two months later in view of aggressive tumor behavior with lymphovascular invasion on pathology,multiple tumor thrombi in the large sized hilar vessels of the liver and in the hilar soft tissue,and a known carbon-11 avid segment V nodule noted on preoperative positron emission tomography scan.She had unfortunately succumbed since last follow-up due to disease progression but enjoyed survival of over 6 months postoperatively.
The other patient,a 30-year-old female patient,underwent successful laparoscopic wedge resection of segment II of the liver.She was born with complex cyanotic congenital heart disease with criss-cross atrioventricular valves,double outlet right ventricle,severe pulmonary stenosis,and hypoplastic pulmonary arteries.At the age of six she underwent modified Fontan procedure,with intra-atrial baffle repair,creation of atrial septal defect,truncation of main pulmonary artery,and pulmonary valve closure.Her condition was complicated by recurrent protein losing enteropathy,with transcatheter atrial septostomy performed at the age of twelve.Rising alpha-fetoprotein levels up to 150 ng/mL were further investigated with magnetic resonance imaging showing HCC 3.6×2.6×1.9 cm in segment II (Fig.2).Resection was performed by means of a laparoscopic procedure which was achieved with a low and stable pneumoperitoneum.Pathology confirmed a moderately differentiated 3.8×2.8×2.0 cm HCC with adequate resection margins.She enjoyed disease-free survival for 10 months postoperatively,unfortunately suffered a recurrence with multiple subcentimeter arterial-enhancing nodules in both left and right liver lobes,but continued to survive for 15 months postoperatively on TACE.
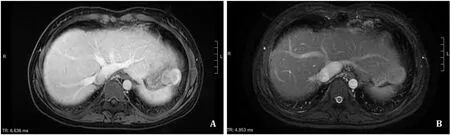
Fig.2. Contrast magnetic resonance images of a patient with Fontan circulation showing hepatocellular carcinoma measuring 3.6×2.6×1.9 cm in segment II.
Multidisciplinary preoperative assessment was performed for both patients including cardiac assessment with electrocardiogram,echocardiogram,cardiopulmonary exercise testing (CPET),24 h Holter monitoring,and cardiac catheterisation.CPET (adjusted for age and sex) demonstrated a reduction of VO2max to 59% and 75% of predicted,respectively.The remaining non-exercise-state investigations demonstrated no significant impairment in ventricular function,intracardiac thrombus,or outflow obstruction.Cardiac magnetic resonance imaging was also performed to demonstrate satisfactory ejection fraction and stroke volume,as well as a patent Fontan shunt.Pressures of the pulmonary artery,right atrium,superior and inferior vena cava,as well as hepatic venous pressures were also measured showing satisfactory results.
Intraoperatively,central venous catheters were inserted to allow monitoring of CVP,as well as placement of transoesophageal echocardiogram.For the first patient undergoing an open procedure,cell saver was also placed.
From a surgical point of view,the strategies used to counter challenges in the patient with Fontan-circulation are based on the principles of intravascular volume control,maintenance of low intra-abdominal and intra-thoracic pressures,and surgical techniques that avoid compromising cardiac preload.
The single ventricle system lacks active pumping of blood through the lungs,and instead,pulmonary blood flow depends on a gradient between CVP and atrial pressure.Any significant changes in CVP that arise from surgery including blood loss and hypovolemia,particularly due to back flow from hepatic veins,should be avoided to prevent disruption to this circulation.
For the open hepatectomy,Pringle maneuver has commonly been used during hepatectomy to reduce liver inflow,while total vascular exclusion of vena cava clamping has traditionally been a definitive and useful method of reducing blood loss.However,significant reductions in blood pressure may not be tolerable in these patients who are sensitive to changes in CVP and intravascular volume.Test clamping is a useful strategy to check hemodynamic changes [5],and significant changes with vena cava clamping can be avoided with hepatic vein clamping instead.The avoidance of hepatic inflow occlusion with the Pringle maneuver also preserves cardiac preload as far as possible and reduces intraoperative risk [6],given that the Fontan circulation is limited by impaired cardiac preload.Alternatively,the reverse Trendelenburg position may also be used to reduce CVP and blood loss from hepatic vein back flow without compromising the circulation stability.Lowering the CVP to<6 cmH2O has also been explored to provide an almost bloodless field [7,8];while there have been concerns of a comparatively higher risk of air embolism,a trial in domestic pigs demonstrated that embolism of small bubbles was unlikely to cause hemodynamic consequences and could be rapidly absorbed due to the high solubility of CO2in plasma [9]in the absence of a ventricular septal defect or atrial septal defect.Postoperatively,open hepatectomy is also associated with more pain compared to the laparoscopic approach.Consequences of suboptimal pain control and resultant postoperative atelectasis become amplified in the post-Fontan circulation,in which atelectasis and hypoxia increase the pulmonary vascular resistance [10].It is therefore especially important to take note of appropriate analgesic titration;a multidisciplinary approach with pain specialist colleagues is often beneficial.
For the laparoscopic hepatectomy,the pneumoperitoneum becomes a prudent focus for vascular and ventilatory control.On the one hand,a safe surgical field and dissection plane visualization demand adequate pneumoperitoneum,while excessive insufflation reduces venous return,and demands greater positive pressure ventilation to counteract and maintain intra-thoracic pressure against an elevated diaphragm.Carbon dioxide absorbed from the peritoneum also accumulates in the partial pressure of arterial carbon dioxide,which further increases pulmonary vascular resistance [10].Ultimately,a stable pneumoperitoneum at low pressures below CVP prevents compromising venous return and further reduction in cardiac output.As a precautionary measure,preparation for swift conversion to open hepatectomy would also mitigate these challenges.
From an anesthetic point of view,principles of management in the Fontan circulation are based on maintenance of preload,low pulmonary vascular resistance,avoidance of high intrathoracic pressure [11],avoidance of arrhythmias,avoidance of ventricular dysfunction,avoidance of worsening intra-cardiac right to left shunt and paradoxical air embolism,and minimizing the surgical stress response.Close control of intravascular volume to maintain preload and cardiac output can be aided through adequate volume replacement guided by transesophageal echocardiography(TEE).The benefits of adequate pulmonary perfusion must be balanced with the risks of hypervolemia and subsequent pathological right atrial distension and precipitation of arrhythmia [5].Judicious use of anesthetic agents that cause myocardial depression and venodilation such as sevoflurane,and pure alpha agonist vasopressors that increase systemic vascular resistance such as phenylephrine would be beneficial [5].Measures to reduce pulmonary vascular resistance include adequate minute volume and ventilation to avoid hypoxic vasoconstriction and hypercarbia.Positive endexpiratory pressure has also been administered concurrently with nitric oxide as a pulmonary dilator to maintain pulmonary blood flow and counter any increase in pulmonary vascular resistance due to pneumoperitoneum [10,11].However,excessively high intrathoracic pressures should be avoided to prevent reduction in venous return.Close anesthetic monitoring of cardiac output and central venous oxygenation can also mitigate the risks of reduced venous return and cardiac preload during reverse Trendelenburg positioning [10].
In summary,we highlighted the points regarding surgical challenges in open and laparoscopic hepatectomy in the post-Fontan population.Both approaches have allowed successful resection of HCC and we anticipate its demand to become increasingly important as the long-term survival of these patients continues to improve.
Acknowledgments
None.
CRediT authorship contribution statement
Karin KY Ho:Conceptualization,Data curation,Formal analysis,Investigation,Writing– original draft.Wong Hoi She:Conceptualization,Data curation,Investigation,Methodology,Supervision,Writing– review &editing.Simon HY Tsang:Supervision,Writing– review &editing.Kevin S Lo:Supervision,Writing– review &editing.Tan To Cheung:Project administration,Supervision,Writing– review &editing.
Funding
None.
Ethical approval
According to local guidelines,institutional ethical approval is not required for using anonymous data for research purposes.The patients had given their informed consent to the use and publication of their anonymous data for research purposes.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2024年1期
Hepatobiliary & Pancreatic Diseases International2024年1期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Pre-MASLD: Should it be defined separately?
- Comment on “Robotic surgery and liver transplantation: A single-center experience of 501 robotic donor hepatectomies”
- Pancreatic panniculitis as the first presentation of pancreatic ductal adenocarcinoma
- Benign stricture of bilioenteric anastomosis after Whipple with synthetic polypropylene suture
- A robust genomic-based prognostic model for the assessment of cancer stemness and survival for patients with hepatocellular carcinoma
- Endoscopic hemostasis using self-expandable metal stent combined with PuraStat ® for patient with high risk of post-endoscopic sphincterotomy bleeding (with video)
