Trends in colorectal cancer incidence according to an increase in the number of colonoscopy cases in Korea
Ga Hee Kim,Yeong Chan Lee,Tae Jun Kim,Sung Noh Hong,Dong Kyung Chang,Young-Ho Kim,Dong-Hoon Yang,Chang Mo Moon,Kyunga Kim,Hyun Gun Kim,Eun-Ran Kim
Abstract BACKGROUND The incidence of colorectal cancer (CRC) and preinvasive CRC (e.g.,early colon cancer and advanced adenoma) is gradually increasing in several countries.AIM To evaluate the trend in incidence of CRC and preinvasive CRC according to the increase in the number of colonoscopies performed in Korea.METHODS This retrospective cohort study enrolled Korean patients from 2002 to 2020 to evaluate the incidence of CRC and preinvasive CRC,and assess the numbers of diagnostic colonoscopies and colonoscopic polypectomies.Colonoscopy-related complications by age group were also determined.RESULTS The incidence of CRC showed a rapid increase,then decreased after 2012 in the 50-75 year-age group.During the study period,the rate of incidence of preinvasive CRC increased at a similar level in patients under 50 and 50-75 years of age.Since 2009,the increase has been rapid,showing a pattern similar to the increase in colonoscopies.The rate of colonoscopic polypectomy in patients aged under 50 was similar to the rate in patients over 75 years of age after 2007.The rate of complications after colonoscopy and related deaths within 3 mo was high for those over 75 years of age.CONCLUSION The diagnosis of preinvasive CRC increased with the increase in the number of colonoscopies performed.As the risk of colonoscopy-related hospitalization and death is high in the elderly,if early lesions at risk of developing CRC are diagnosed and treated under or at the age of 75,colonoscopy-related complications can be reduced for those aged 76 years or over.
Key Words: Colorectal cancer;Preinvasive colorectal cancer;Colorectal polypectomy;Colonoscopy
INTRODUCTION
Colorectal cancer (CRC) is the third most commonly diagnosed cancer with an estimated 1.8 million new cases in 2018,and is the second leading cause of cancer-related death in the world.In Korea,CRC showed the second highest incidence rate among all cancers in 2018,with an estimated 44.5 cases per 100000 persons per year[1,2].Following a rapid decline during the 2000s,the CRC incidence rate in men and women has remained generally stable.This decline has been greatly affected by screening colonoscopy and the removal of colorectal precancerous lesions[3].Most CRCs occur at the age of 50 to 70 years.Thus,several guidelines have recommended CRC screening colonoscopy for those over 50 years of age[4,5].However,over the last few decades,the incidence of CRC has increased in younger patients aged <50 years[6].In Korea,due to the low cost of colonoscopy and availability of many skilled colonoscopists,access to screening colonoscopy from a young age is different to that in Western countries[7].Several early CRCs,including precancerous lesions,have been detected by screening colonoscopy.Endoscopic resection procedures include polypectomy,endoscopic mucosal resection,and endoscopic submucosal dissection.Using these procedures,early diagnosis and treatment of early CRCs can be performed[8,9].In Korea,the volume of colonoscopies and colorectal polypectomies in the elderly aged 75 years or older is also increasing due to the CRC screening program initiated in 2004 and rapid population aging[10].In this context,we assessed national population-based data on CRC occurrence by age and gender.In particular,the purpose of this study was to evaluate the trend in incidence of CRC and preinvasive CRC according to age group and gender and to determine whether age adjustment for endoscopy during health examination would be necessary in the future.In addition,we attempted to confirm colonoscopy-related complications according to age and gender.
MATERIALS AND METHODS
Dataset
We used the National Health Insurance Service (NHIS) claims database to identify trends in CRCs and colorectal polypectomy in South Korea.We selected CRC patients and those who underwent colorectal polypectomy from the NHIS claims database that includes approximately 50 million persons,almost the entire population of South Korea.The database is deidentified with regard to gender,age,and medical history.The study population was followed up for 19 years from 2002 to 2020.We excluded patients who had data missing on gender,age,or imprecise data on death.The study protocol was approved by the Institutional Review Board of Samsung Medical Center (2019-08-140).
Definition of outcome of interest
We defined CRC patients as those who were diagnosed with CRC [International Classification of Diseases version 10 (ICD-10) code C18-C21].Preinvasive CRC patients were defined as those with ICD-10 codes D010,D011,and D012.Patients who underwent a colorectal polypectomy were defined as those with treatment codes of Q7701-03 and QX706.In addition,patients who underwent a colonoscopy without colorectal polypectomy were defined as those with the treatment code E7660.
Study design for trends in CRC and colorectal polypectomy
To identify trends in CRC and colorectal polypectomy,an incident case was defined as a new case without diagnostic history for the target disease right before 2 years,while a prevalent case was defined as a case with the target disease every year.We classified subjects into three age groups: <50 years,50-75 years,and ≥ 76 years.The number of diagnostic colonoscopies was calculated as the sum of cases of colonoscopy alone and cases of polypectomy,minus the number of cases counted as one if both colonoscopy and polypectomy were performed within 1 year.
Study design for identifying the associations between age, hospitalizations and deaths after colonoscopy
We analyzed whether patients who underwent colonoscopy from January 2002 to December 2020 were assigned a diagnostic code for colonoscopy-related complications.We determined whether patients undergoing colonoscopy were given diagnostic codes for gastrointestinal (GI)-related complications of ‘intestinal perforation’ [K63.1,(ICD-10)] and ‘intestinal bleeding’ [K92.0-92.2,(ICD-10)] and non-GI-related complications such as heart disease [I21 and I50.0,(ICD-10)] and brain disease [I60-64,(ICD-10)] that might contribute to mortality.We also assessed whether patients with these codes were hospitalized or died within 1 mo or 3 mo using trend analysis.
Statistical analysis
We measured rates of prevalence,hospitalization,and death in those with GI-and non-GI complications after colonoscopy within 1 mo or 3 mo between 2002 and 2020.Then,we performed trend analyses using Cochran-Armitage trend tests to investigate the associations between age and complications.Statistical significance was considered when thePvalue was less than 0.05.Data processing and statistical analyses were performed with SAS software version 9.4 (SAS Institute,Cary,NC,United States) and R software (version 4.0.3;R Foundation for Statistical Computing,Vienna,Austria).
RESULTS
Incidence of CRC and preinvasive CRC between 2004 and 2020
A total of 430696 patients were diagnosed with CRC between 2004 and 2020 (Table 1).During the study period,the incidence of CRC was higher in men than in women over all periods.In particular,the incidence of CRC among men aged 50-75 years increased significantly from 2004 to 2012.The increase in CRC has slowed since 2012 in both men and women (Figure 1A).Between 2004 and 2020,a total of 52069 patients were diagnosed with preinvasive CRC (Table 2).Similar to the incidence of CRC,the incidence of preinvasive CRC during all periods was also more common in men.Since 2009,the incidence of preinvasive CRC has shown a sharp rise in both men and women,especially in men,and in those aged 50-75 years (Figure 1B).We also calculated the rate of incidence of preinvasive CRC (the ratio of the incidence of preinvasive CRC to the sum of the incidence of CRC and preinvasive CRC).Although the incidence of CRC continued to increase while the rate of its increase decreased from 2012,during the study period the rate of incidence of preinvasive CRC increased in all age groups.The rate of preinvasive CRC increase in patients under 50 years of age was similar to that in patients aged 50-75 years (Supplementary Table 1,Figure 2).
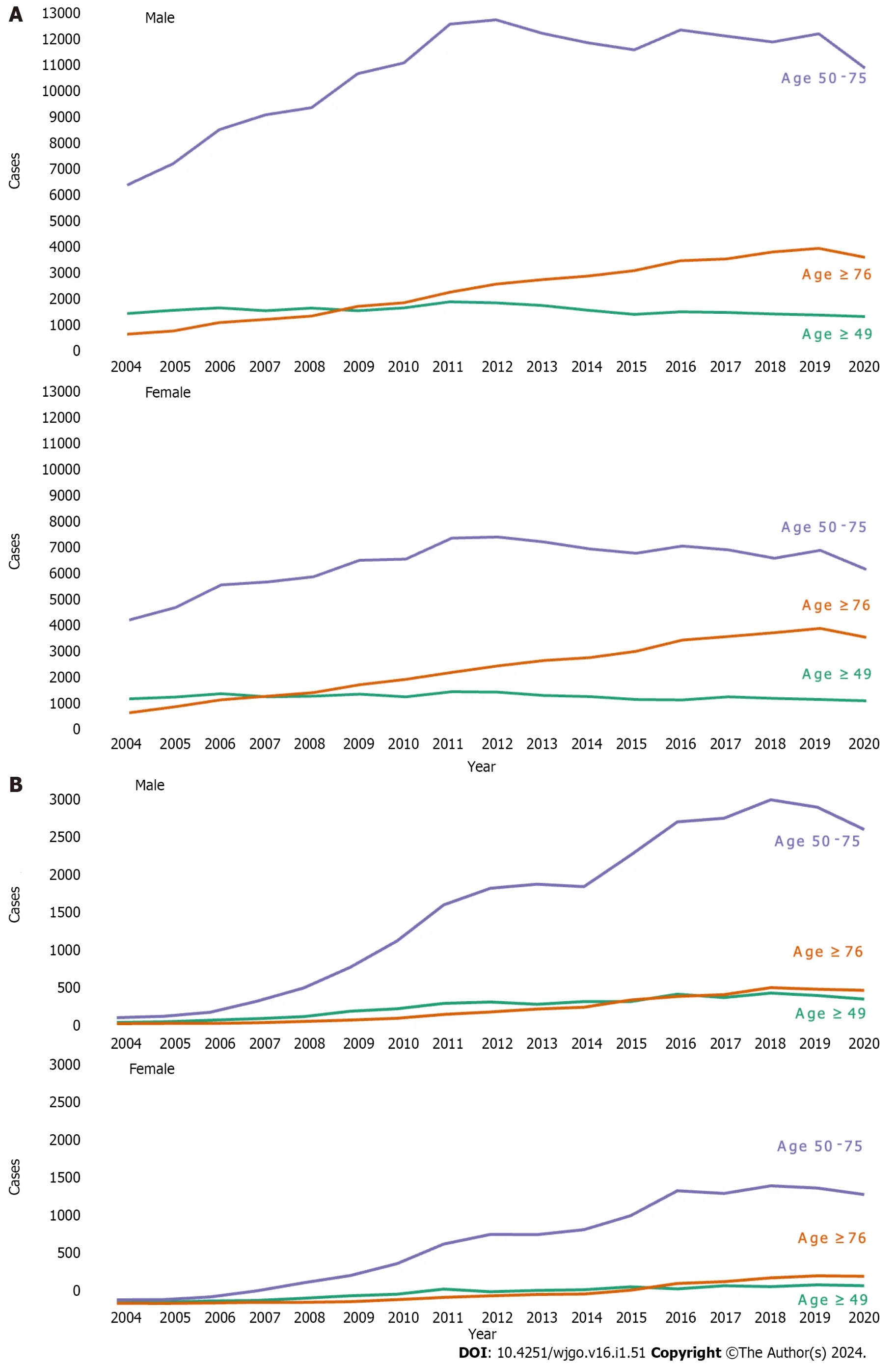
Figure 1 The incidence of colorectal cancer and preinvasive colorectal cancer by age and gender between 2004 and 2020. A: Colorectal cancer;B: Preinvasive colorectal cancer.

Figure 2 The proportion of preinvasive colorectal cancer among all colorectal cancers by age between 2004 and 2020.
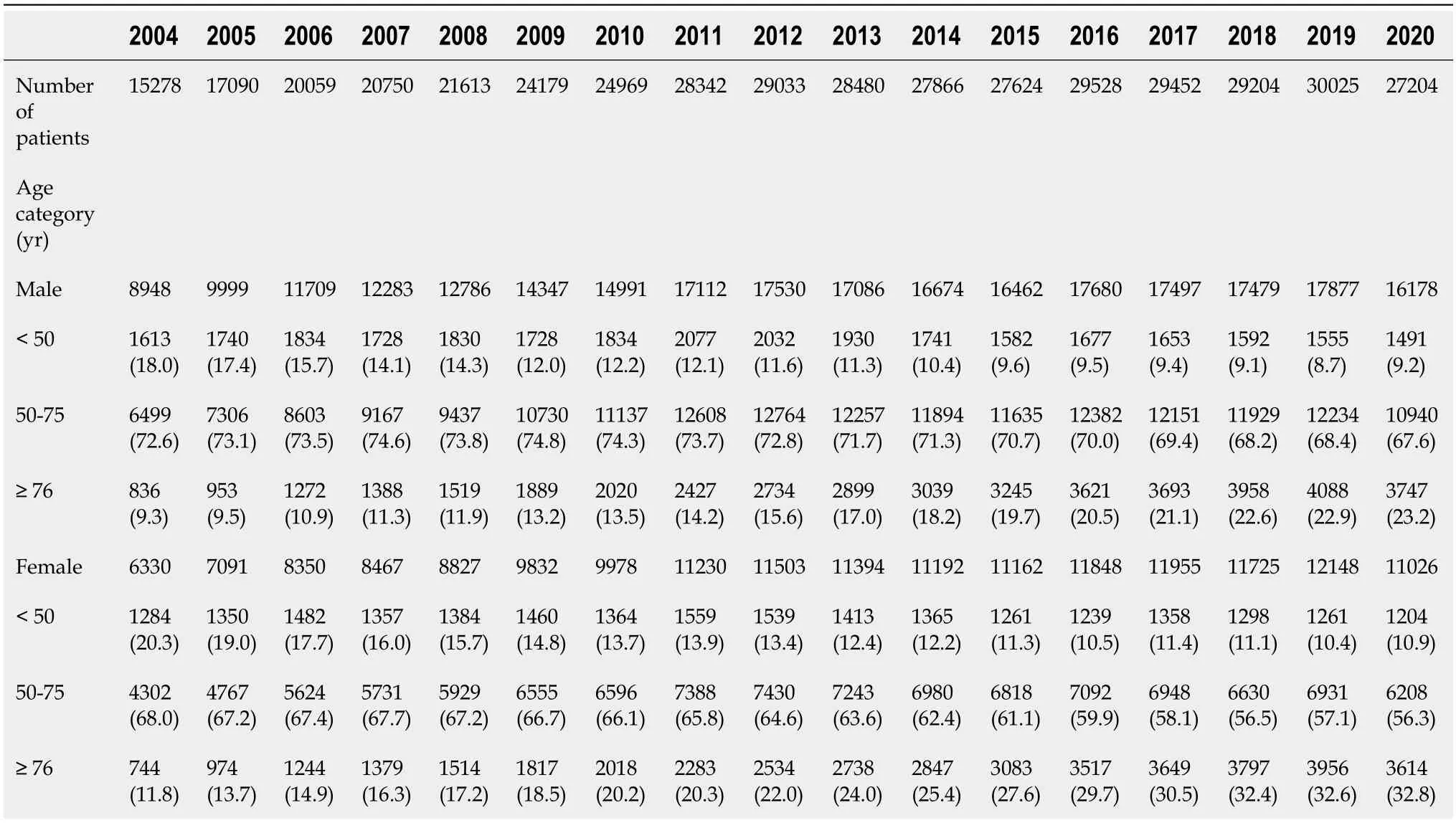
Table 1 The incidence of colorectal cancer by age and gender between 2004 and 2020,n (%)
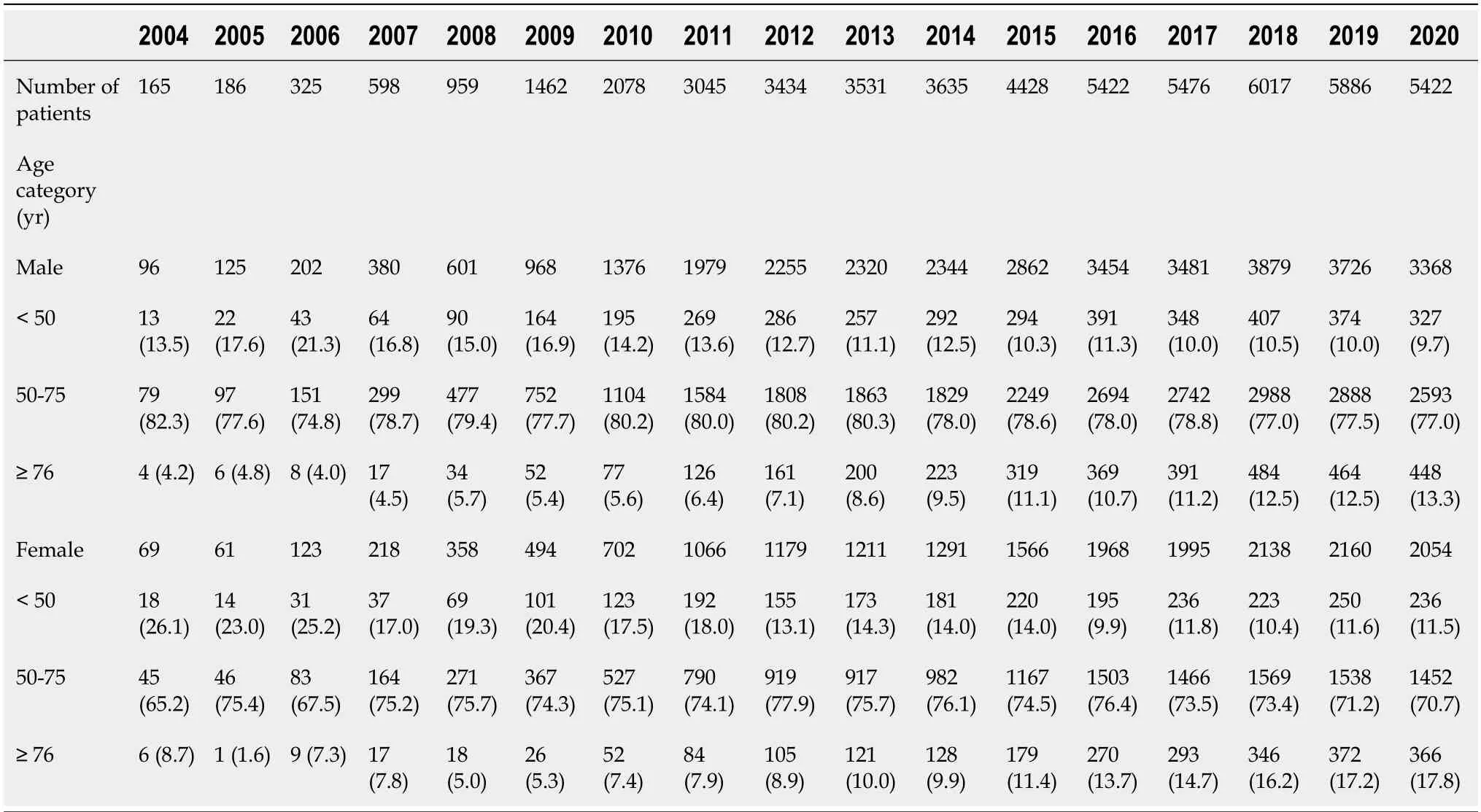
Table 2 The incidence of preinvasive colorectal cancer by age and gender between 2004 and 2020,n (%)
Trends in the number of colonoscopies between 2002 and 2020
In this study,we identified the total number of patients who underwent diagnostic colonoscopy (colonoscopy without polypectomy) and colonoscopic polypectomy,respectively,from 2002 to 2020 in the study database (Table 3).The number of patients who underwent diagnostic colonoscopy increased since 2002 in all age groups.The number of patients in 2020 had increased by approximately fifteen-fold compared to that in 2002.In particular,it showed a gradual increase after 2002.It then showed a sharp increase after 2010 in the 50-75 years age group.This pattern also appeared in the age group of under 50 years.However,the total number of patients who underwent diagnostic colonoscopy was lower than that in the 50-75 years age group,the age group that is subjected to screening colonoscopy.The pattern of change in the number of patients who underwent a colonoscopic polypectomy was similar to that of diagnostic colonoscopy (Table 3,Figure 3A).The number of patients who underwent a colonoscopic polypectomy gradually increased since 2002 in all age groups.Since 2010,it has shown a sharp increase among those under 75,especially in the 50-75 years age group.For those aged 76 years or older,colonoscopic polypectomies increased significantly in 2020,compared to 2002.The rate of colonoscopic polypectomies (the ratio of colonoscopic polypectomies to the sum of diagnostic colonoscopies and colonoscopic polypectomies) also steadily increased during the study period (Table 3,Figure 3B).The rate of colonoscopic polypectomies in 2020 increased by approximately two-fold compared to that in 2002.The increase in the rate of colonoscopic polypectomies in the under 50 age group showed a relatively steep increase,compared to other age groups.After 2018,the rate of colonoscopic polypectomies for patients under 50 years was slightly higher than those in the other two age groups.
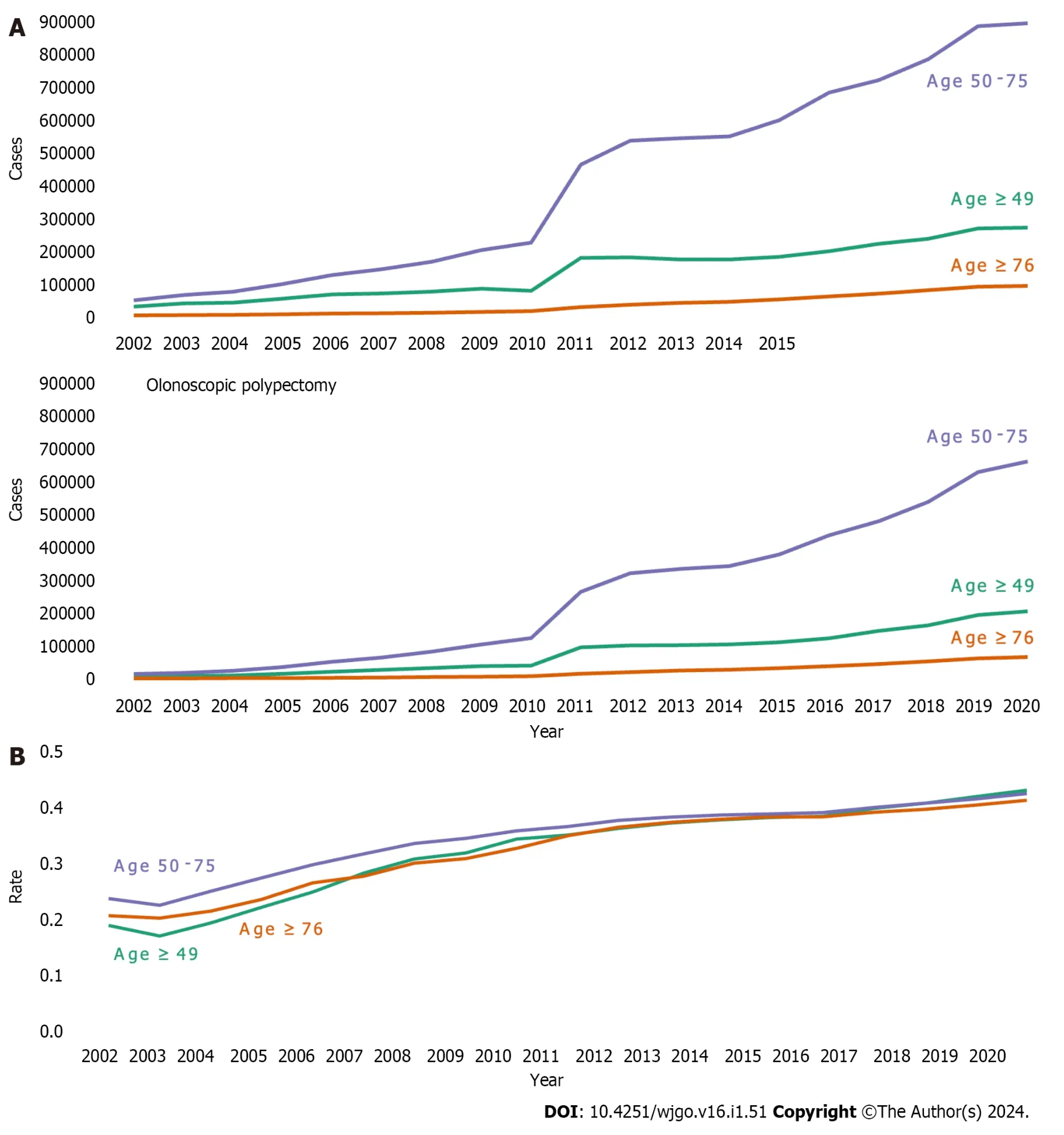
Figure 3 The total number of colonoscopies and colonoscopic polypectomies,and the proportion of colonoscopic polypectomies among the total number of colonoscopies and colonoscopic polypectomies by age,between 2002 and 2020. A: The total number of colonoscopies and colonoscopic polypectomies;B: The proportion of colonoscopic polypectomies among the total number of colonoscopies and colonoscopic polypectomies.

Table 3 The number of diagnostic colonoscopies (colonoscopy without polypectomy),colonoscopic polypectomies,and the proportion of colonoscopic polypectomies by age between 2002 and 2020
Hospitalizations and deaths after colonoscopy between 2002 and 2020
Among patients who underwent a colonoscopy,those who were additionally diagnosed with GI-and non-GI-related complications were classified by age group.We also determined whether patients were hospitalized or died within 1 mo and 3 mo (Supplementary Table 2).As age increased,the number of complications and related hospitalizations and deaths increased.In particular,the rate of complications after colonoscopy and related deaths within 3 mo were high for those aged 76 years or older.
DISCUSSION
Using a nationwide,population-based database,we analyzed changes in the incidence of CRC according to age and the incidence rate of preinvasive CRC with endoscopic resection in Korea over a 19-year period.We found that the rate of endoscopically resectable preinvasive CRC continued to increase over time,with the 50-75 years age group having the highest proportion for both men and women.In addition,the rate of incidence of preinvasive CRC increased in a similar pattern in patients under 50 and 50-75 years of age.The incidence of preinvasive CRC showed an increased pattern similar to the increase in the number of colonoscopies,showing a gradual increase from 2005 to 2009,followed by a sharp increase after 2010.Unlike the incidence of preinvasive CRC,which steadily increased during the 17-year observation period,the incidence of CRC showed a slight decrease in the under 50 and 50-75 years age groups around the middle of the observation period.This suggested that the decrease in the incidence of CRC in the under 76 years age group might be related to the diagnosis,treatment,and subsequent periodic follow-up colonoscopy of preinvasive CRC in the younger age group.The increase in the incidence of CRC in patients aged 76 years or older was associated with an increase in the number of colonoscopies.The CRC screening guideline published in Korea in 2015 recommends starting CRC screening from age 50[11].The total number of colonoscopies performed during the 19-year period showed a steady increase.In particular,it showed a sharp increase from 2010 to 2011.In addition to the explosive increase in colonoscopy performed for those in the 50-75 age group,there was a significant increase in the younger under 50 years age group.The new American Cancer Society guideline published in 2018 recommends extending the age of CRC screening colonoscopy to 45 years of age[12].The trend in Korea for the past 17 years from 2004 to 2020 has shown a steady increase in CRC and preinvasive CRC diagnosis due to the increase in the number of colonoscopies and colonoscopic polypectomies in all age groups.In particular,the rate of colonoscopic polypectomies increased in those under 50 years of age.The rate of preinvasive CRC diagnosis in those under the age of 50 increased similar to that in those aged 50-75 years,the age group recommended for CRC screening.Therefore,these findings provide real-world evidence that colonoscopic polypectomy,especially preinvasive CRC resection,affects the occurrence of CRC.Several studies and guidelines have discussed extending the age of CRC screening from 45 to 75 years of age[4,13].Previous studies have been conducted on how to determine the upper age limit for diagnostic colonoscopy in the elderly over 70 years of age[14-16].Most studies recommended that the start and end time of CRC screening colonoscopy should be determined through a personalized discussion in consideration of the patient’s underlying comorbidities and functional status as well as the patient’s preferences[16,17].In most countries,colonoscopy is mainly performed between the ages of 50 and 75[4,10,18].Similarly,when subjects were classified into three age groups in this study,it was found that colonoscopy was mainly performed between 50 and 75 years of age.In this study,the frequency of colonoscopies and colonoscopic polypectomies increased in all age groups from 2002 to 2020.In particular,the number of colonoscopies increased in the elderly aged 76 years or older.We analyzed whether patients who underwent a colonoscopy from January 2002 to December 2020 were assigned a diagnostic code for colonoscopy-related complications[19,20],and determined hospitalizations and deaths that occurred within 1 mo and 3 mo after colonoscopy.As expected,the rate of hospitalization and death after colonoscopy in the elderly was high.The rate of complications and deaths after colonoscopy within 3 mo was high for those aged 76 years or older.This trend shows that older age and their comorbidities could increase the risk of these complications.
Rapid population aging in Korea is considered a major factor in the increased number of colonoscopies and colorectal polypectomies performed in the elderly[21].We also found that the diagnosis of CRC and preinvasive CRC increased in the elderly aged 76 years or older with a high rate of complications after colonoscopy in these patients.Therefore,when endoscopists perform colonoscopy,they should consider each patient’s individual information,rather than determining an upper age limit for screening colonoscopy.
This study has several limitations.The study population was obtained from the NHIS database,a database for the reimbursement of medical claims.In this study,CRC and preinvasive CRC were identified through ICD codes and the distribution level was confirmed by gender and age.In Korea,statistics on cancer patients are periodically checked through the national cancer registration statistics project.Data quality issues might exist.However,when data were compared by year,there was no significant difference.The trend in CRC was confirmed to be similar.In this study,NHIS data were used for further analysis.In addition,we were unable to assess several potential confounding factors[22],such as clinical findings,laboratory data,lifestyle or personal health behaviors (including smoking and alcohol intake) and physiological characteristics (such as body mass index).However,we minimized selection bias and referral bias by using large-scale administrative data obtained for the majority of the Korean population.
CONCLUSION
Screening colonoscopy seems to have an important effect on the prevention of advanced CRC in the younger under 50 years age group as well as in the 50-75 year age group.Therefore,the role of colonoscopy as a screening test for CRC is very important even for those under the age of 50.As expected,the risk of colonoscopy-related hospitalization and death was high in the elderly.This suggested that if lesions at risk of developing CRC are diagnosed early and treated in the age group under 75 years of age,complications related to colonoscopy can be reduced in those over 75 years of age.In addition,before performing endoscopy for elderly patients,physicians should have sufficient consultation based on the patient’s personalized information and make a decision considering the risk and benefit.
ARTICLE HIGHLIGHTS
Research background
In Korea,colorectal cancer (CRC) showed the second highest incidence rate among all cancers in 2018.The volume of colonoscopy and colorectal polypectomy in Korea is also increasing due to the CRC screening program initiated in 2004 and rapid population aging.
Research motivation
We examined whether evaluating the trend in the incidence of CRC and preinvasive CRC by age group and gender would be helpful in determining the age group that is indicated for screening endoscopy in the future.
Research objectives
This study aimed to evaluate the trend in incidence of CRC and preinvasive CRC according to the increase in colonoscopies performed in Korea.
Research methods
Korean patients from 2002 to 2020 were identified to evaluate the incidence of CRC and preinvasive CRC and assess the number of diagnostic colonoscopies and colonoscopic polypectomies.Colonoscopy-related complications by age group were also determined.
Research results
Over the study period,the rate of incidence of preinvasive CRC increased at a similar level for patients under 50 and 50-75 years of age.Since 2009,the increase in the rate of incidence has been rapid,showing a pattern similar to the increase in the number of colonoscopies.
Research conclusions
The diagnosis of preinvasive CRC has increased with the increase in the number of colonoscopies performed.The role of screening colonoscopy for CRC has become very important even for those under the age of 50 years.
Research perspectives
As the risk of colonoscopy-related complications is high in the elderly,if early lesions at risk of developing CRC are diagnosed and treated in the 75 years or under age group,complications related to colonoscopy can be reduced for those over 75 years of age.
FOOTNOTES
Co-first authors:Ga Hee Kim and Yeong Chan Lee.
Author contributions:Kim TJ,Hong SN,Chang DK,Kim YH,Yang DH,Moon CM,Kim K,Kim HG,and Kim ER performed critical revision of the manuscript for important intellectual content;Kim GH and Lee YC acquired data from the National Health Insurance Service claims database and analyzed the data;Kim GH And Lee YC interpreted the data;Kim GH and Lee YC participated in the design of the study and performed the statistical analysis;the results shown in tables and figures were performed by Kim GH and Lee YC.The main text of the manuscript was written by Kim GH and Lee YC.Kim GH and Lee YC reviewed and edited the manuscript.Kim GH and Lee YC contributed equally to this work as co-first authors of this paper.Kim ER and Kim HG contributed the study concept and design.All authors have read and approved the final manuscript.
Institutional review board statement:The study was reviewed and approved for publication by our Institutional Reviewer.
Informed consent statement:In this retrospective cohort study,patients were not required to give informed consent to the study as the analysis used the National Health Insurance Service claims database which contains anonymous clinical data and is deidentified with regard to gender,age,and medical history.
Conflict-of-interest statement:All the Authors have no conflict of interest related to the manuscript.
Data sharing statement:No additional data are available.
STROBE statement:The authors have read the STROBE Statement-checklist of items,and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:South Korea
ORCID number:Ga Hee Kim 0000-0002-7214-9918;Yeong Chan Lee 0000-0002-2093-3161;Tae Jun Kim 0000-0001-8101-9034;Sung Noh Hong 0000-0002-4140-3717;Dong Kyung Chang 0000-0001-8925-4629;Dong-Hoon Yang 0000-0001-7756-2704;Kyunga Kim 0000-0002-0865-2236;Eun-Ran Kim 0000-0002-0495-2565.
S-Editor:Qu XL
L-Editor:Webster JR
P-Editor:Zhang XD
 World Journal of Gastrointestinal Oncology2024年1期
World Journal of Gastrointestinal Oncology2024年1期
- World Journal of Gastrointestinal Oncology的其它文章
- Comprehensive analysis of the role of ubiquitin-specific peptidases in colorectal cancer: A systematic review
- Colonoscopy plays an important role in detecting colorectal neoplasms in patients with gastric neoplasms
- Analysis of the potential biological value of pyruvate dehydrogenase E1 subunit β in human cancer
- Colorectal cancer’s burden attributable to a diet high in processed meat in the Belt and Road Initiative countries
- Emerging role of liquid biopsy in rat sarcoma virus mutated metastatic colorectal cancer: A case report
- Comprehensive evaluation of rare case: From diagnosis to treatment of a sigmoid Schwannoma: A case report
