Hepatocellular carcinoma recurrence: Predictors and management☆
Wl Abdelhmed ,Mohmed El-Ksss
a Endemic Medicine Department, Sohag University, Sohag, Egypt
b Endemic Medicine Department, Faculty of Medicine, Helwan University, Cairo, Egypt
Keywords: Hepatocellular carcinoma (HCC)Recurrence Ablation Liver resection Liver transplantation
ABSTRACT Hepatocellular carcinoma (HCC),the sixth most common cancer globally,is associated with high mortality rates and more than 830,000 annual deaths.Despite advances in the available management options including surgical resection and local ablative therapies,recurrence rates after the initial treatment exceed 50%,even among patients who have undergone curative-intent therapy.Moreover,postsurgical HCC recurrence occurs in about 70% of cases five years postoperatively.The management of recurrent HCC remains undefined.This review discusses different predictors for HCC recurrence after each treatment modality and different approaches available to stratify these patients.More specific guidelines for managing HCC recurrence and strict surveillance protocols for such recurrence after initial HCC management are needed.
1.Introduction
Hepatocellular carcinoma (HCC),the most prevalent malignant hepatic tumor,is one of the leading causes of cancer-related mortality worldwide.1Moreover,HCC is ranked as the sixth most commonly encountered cancer(906,000 new cases)and the thirdleading cause of cancer-related death globally (830,000 deaths) in 2020.2HCC alone represents about 90% of all primary hepatic malignancies and nearly 9% of all newly reported ones.3The background of liver cirrhosis is the most crucial risk factor for HCC,given that it is a chronic premalignant condition.4HCC occurs in 80%-90% of patients with underlying cirrhosis.5Among patients with cirrhosis who had hepatitis B virus(HBV)or hepatitis C virus(HCV)infection,the incidence of HCC was 88%or 93%,respectively.6The yearly and five-year cumulative incidence is 1%-4% and 5%-30%,respectively.6This variation could be explained by many factors such as the underlying etiology of sex,liver disease,associated comorbidities,and the tumor’s location.7HBV infection is the most important risk factor for HCC,accounting for almost 50% of reported cases.8Furthermore,the risk of HCC associated with HCV infection has decreased as patients achieve sustained virological response while taking antiviral drugs.9Metabolic dysfunctionassociated steatohepatitis is the fastest-growing HCC etiology,especially in the West.10Many current clinical staging systems,such as the Barcelona Clinic Liver Cancer (BCLC) staging system,are available for the stratification of HCC management according to tumor stages and the expected outcomes of various interventions.11,12Potentially curative interventions such as resection,local ablation,and liver transplantation (LT),are usually proposed to patients with early-stage HCC.12Microwave ablation(MWA),has emerged among other thermal ablative techniques that are currently in use,destroying tumors by direct hyperthermia injury similar to radiofrequency ablation (RFA).13Patients with intermediate stages of the disease are the primary candidates for transarterial chemoembolization (TACE),while those with advanced disease may benefit from various available systemic therapies.12Unfortunately,even after curative treatment,patients continue to experience recurrence;additionally,repeated hepatectomy,RFA,and TACE treatments impair liver function in many patients,leading to death from liver failure or tumors that are refractory to systemic therapy.14HCC is generally an aggressive disease,with a five-year survival rate of less than 20%and a recurrence rate of up to 88%.15,16The high recurrence rates after curative HCC treatment constitute the main reason for the poor prognosis.17Thus,the prevention of HCC recurrence following curative treatment could significantly improve the prognosis of the condition;however,research on recurrence prevention has been ineffective so far.18,19This review discusses HCC recurrence in different situations,the patient and tumor related factors predicting it,survival in those patients,and how to fill the gaps.
2.Predictors of HCC recurrence
Irrespective of its etiology and the treatment strategy employed,HCC can often recur.16Many patients will develop a second recurrence with a reported incidence of 50%-70%,even after managing their first relapse.20,21Moreover,some patients may experience a third or fourth relapse after prior curative-intent treatment.However,this is uncommon,as available data suggest that each successive curative-intent procedure predisposes patients to diminished long-term survival.22HCC recurrence could be associated with some HCC tumor-related risk factors,including tumor aggressiveness,multinodularity,large size (≥5 cm),macroscopic vascular or microscopic lymphovascular invasion,high preoperative alpha-fetoprotein (AFP) levels,as well as the patient-related risk factors such as the presence of cirrhosis in addition to advanced initial BCLC stages.16,23,24Recurrence has primarily been investigated postresection and LT.25-28Researchers have sought to develop a composite scoring tool to assess recurrence risk after ablation,and some investigators employ artificial intelligence.29,30Other factors,such as the time to recurrence,extrahepatic spread,size,and the number of recurrent nodules,are likely to be more beneficial in estimating the postrecurrence overall survival (OS)and disease-free survival.31,32Furthermore,intrahepatic metastasis poses a serious issue for tumors larger than 2 cm,as the tumor size is directly proportional to the risk of both microvascular invasion and intrahepatic metastases.14Table 1 summarizes the risk factors/predictors of HCC recurrence.
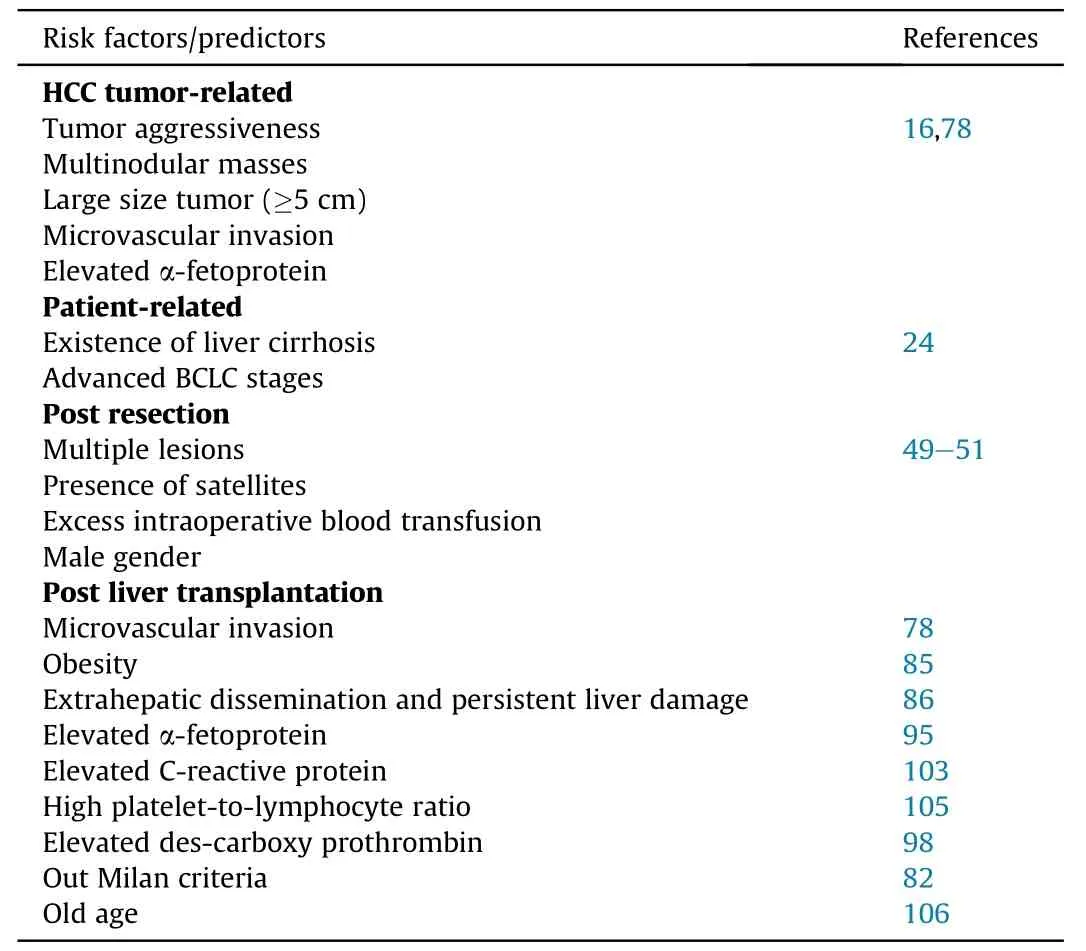
Table 1 Risk factors/predictors for HCC recurrence.
3.Early detection of HCC recurrence is a necessity
Close surveillance is mandatory since many patients develop HCC recurrence early following treatment.15Generally,it is advisable to do follow-up patients subsequent to HCC intervention at intervals of 3-4 months during the initial 1-3 years,every 6 months during years 3-5,and subsequently on a yearly basis for a minimum of 10 years.16Both primary tumor characteristics(i.e.riskof recurrence) and the underlying liver quality (i.e.risk ofde novodisease) determine the timing of surveillance.16Surveillance includes the utilization of contrast-enhanced multidetector computed tomography (MDCT) or magnetic resonance imaging(MRI) scanning in conjunction with AFP-level assessment.33The utilization of gadoxetic-enhanced MRI has been observed to exhibit greater sensitivity in detecting HCC recurrences measuring less than 2 cm,as well as demonstrating a higher level of accuracy when compared to both MDCT and conventional MRI.34Although AFP has a very low sensitivity,it is widely utilized as the primary serological marker for the detection of HCC recurrence.35However,desgamma-carboxy-prothrombin (DCP) has been reported to be superior to AFP in the detection of HCC recurrence and has yet to be incorporated into routine surveillance for HCC recurrence.35-37These inflammatory and angiogenic markers have also been evaluated among transplanted patients.38Moreover,the utilization of liquid biopsy,with the detection of circulating tumor DNA,can enhance the predictive performance of AFP.39Currently,there is no ideal dependable biomarker combination for the detection of early HCC recurrence with high accuracy.40
4.Staging of recurrent HCC
After diagnosis of HCC recurrence,staging should begin with the search for evidence of extrahepatic disease,which is present in 12%-27% of patients.16,41,42Since this is primarily considered a contraindication to surgical treatment,some researchers have suggested that even patients with isolated extrahepatic recurrence may still benefit from resection.43Still,no staging system is established for recurrent HCC;however,primary HCC staging algorithms,such as the BCLC classification,are often extrapolated and used to predict outcomes and guide decision-making.44Yaoet al.44recently used BCLC staging for recurrent HCC and demonstrated a different prognosis in terms of OS among individuals with variable recurrent HCC,validating the prognostic ability of BCLC staging.However,most patients who experienced recurrence received treatment different from the BCLC algorithm suggested in the primary HCC setting.44Existing staging systems,such as the BCLC and the Hong Kong Liver Cancer classifications,were not developed to assess the prognosis or make decisions in recurrent HCC.45Thus,these staging systems and treatment strategy algorithms should not be applied indiscriminately to patients with recurrence.45
5.Management of different scenarios of HCC recurrence
Herein,this review highlights the different patterns and scenarios of HCC recurrence after initial curative treatment strategies,risk factors,and management obstacles.
5.1. HCC recurrence after liver resection
Liver resection is currently one of the main radical interventions among HCC curative treatments.However,its recurrence rates are as high as 60%in the first five years following surgery,even in early smaller lesions.46The path of recurrence is still up for dispute.46A multicenter retrospective study reported a recurrence rate of 45.5%among 756 patients who underwent curative-intent hepatectomy.16In most cases,recurrence has been described to be intrahepatic,arising in the liver remnant rather than close to the resection margin;besides,it mostly occurred within the first two postoperative years.16In another study conducted by Xuet al.,23late recurrence (>2 years after the procedure) was also found to be predominantly intrahepatic(90.1%).Kimet al.47estimated that HCC recurrence peaked within the first year following hepatectomy and then gradually decreased until the fifth postoperative year,followed by stabilization of the recurrence risk until year 10.HCC relapse may be triggered by the precancerous background of the residual diseased liver.Since this is a “multicentricde-novooccurrence”,these tumors are always primitive.48According to the literature,AFP levels of more than 400 mg/L,lesion sizes above 5 cm,multiple lesions,the presence of satellites,microvascular invasion,and the need for intraoperative blood transfusion are pretreatment variables associated with the HCC recurrence risk.49-51Numerous oncological characteristics,including the tumor size,number of tumors,and microvascular invasion,have been associated with a higher risk of postoperative HCC recurrence.46,52Some scores,such as the albumin-bilirubin (ALBI) score,were strongly associated with recurrence after surgical resection.53Regarding the sex differences associated with HCC recurrence risk and mortality following curative resection,a retrospective Chinese study including 1435 HCC patients who underwent curative surgical resection (1228 males and 207 females) did not find any differences in the early recurrence rate(≤2 years following resection)between males and females.However,males had significantly higher rates of late recurrence (>2 years) and postoperative mortality than females.51
A better prognosis for HCC patients has been made possible by surgical techniques and surveillance improvements,however,the recurrence rates are as high as 60%in the first five years following surgery.46,54Laparoscopic surgery has been demonstrated to have better long-term outcomes than open surgery in Meta-analyses and substantial propensity score-matched trials.55,56Laparoscopic liver resection for HCC is always associated with fewer postoperative and oncological complications such as bleeding and liver decompensation.57,58Previous studies have demonstrated that the resection technique has no bearing on the likelihood of HCC recurrence or survival,whereas tumor features and biological behavior may be more important features.59-61A larger surgical margin may prevent early recurrence in patients with HCC;however,extremely wide resection margins may leave insufficient liver parenchyma and cause postresection liver failure.62,63The optimal resection margin for HCC is currently arbitrary and controversial.64,65Anatomical resection,first described by Makuuchiet al.66in 1985,is defined as the tumor resection together with the hepatic segment or subsegment,which includes tumor-bearing portal tributaries as well as a major branch of the portal vein and hepatic artery.Nonanatomic resection,which is a less extensive liver resection than anatomic resection,is best defined as the resection of a lesion regardless of the anatomical segment or section of the lobar anatomy.66,67Still,the benefit in terms of OS and locoregional rates of recurrence by anatomical resection for HCC remains unclear and requires more clinical trials to be ascertained.68After curative liver resection,no specific adjuvant therapy is currently recommended by clinical guidelines to prevent recurrence;however,a few studies have suggested prophylactic transarterial chemoembolization (TACE) and sorafenib.69-71Besides,adjuvant systemic chemotherapy significantly decreases HCC recurrence following curative hepatic resection.72
5.2. HCC recurrence post-LT
5.2.1.Criteria for transplanting HCC patients
In 1963,LT was initially introduced in clinical practice to treat unresectable liver lesions.The Milan criteria allow transplantation in HCC settings in the presence of one lesion measuring less than 5 cm or up to three lesions that each measure less than 3 cm in diameter,with no evidence of vascular invasion and extrahepatic metastasis.73The Milan criteria established the patient’s selection of LT (Fig.1).73LT offers patients a 75% four-year survival rate without extrahepatic spread and macrovascular invasion (MVI).73The early results of LT were unsatisfactory because of the poor survival of transplanted patients owing to the high primary tumor recurrence rates.74Approximately 8% of patients experienced HCC recurrence,making it the leading cause of mortality.73Subsequent studies revealed that 10%-16%of patients experienced post-LT HCC recurrence.75,76These findings demonstrated that HCC recurrence occurs even when the selection criteria for LT are employed,and it is probably caused by the spread of HCC from micrometastases and circulating cancer cells before or during the condition.76The Milan criteria for LT are associated with the sizes and numbers of HCC nodules,which are viewed as surrogate markers for MVI and/or poor tumor differentiation.77MVI and/or poor HCC differentiation are independent indicators of HCC recurrence.78Besides,patients with HCC benefit from LT by expanding the Milan criteria.79Some researchers have explored broadening the Milan criteria by considering the tumor(s)’morphologic characteristics,which were evaluated using radiologic techniques during the pre-LT period.80One of these studies demonstrated that extending the Milan criteria for LT to patients with solitary HCC lesions measuring<9 cm in diameter or those with at most three lesions (with the largest of them measuring 5 cm)and a total tumor size of <9 cm did not significantly affect the one-year and three-year OS or recurrence-free survival compared to the Milan criteria.81Another set of criteria “The University of California San Francisco criteria(UCSF)”,were developed based on a cohort study conducted in the United States (U.S.).82Per these criteria,80.7% of patients would experience a comparable five-year recurrence-free survival after LT,to what was seen when using the Milan criteria.82UCSF criteria allowed transplanting patients with a single lesion measuring less than 6.5 cm or two lesions measuring less than 4.5 cm each.There has been considerable discussion about the link between expanding the Milan criteria for LT and increased HCC recurrence.83Shahet al.84analyzed 155 patients who had confirmed post-LT HCC and met the Milan criteria,and they used pathological investigation to determine whether MVI was present.Of these patients with MVI,68% experienced HCC recurrence.Routine lesion biopsy is frequently not applied because of the tumor multinodularity or the possibility of cancer cell dissemination,despite the unquestionable diagnostic usefulness of pre-LT pathological assessments of tumor grading and MVI.
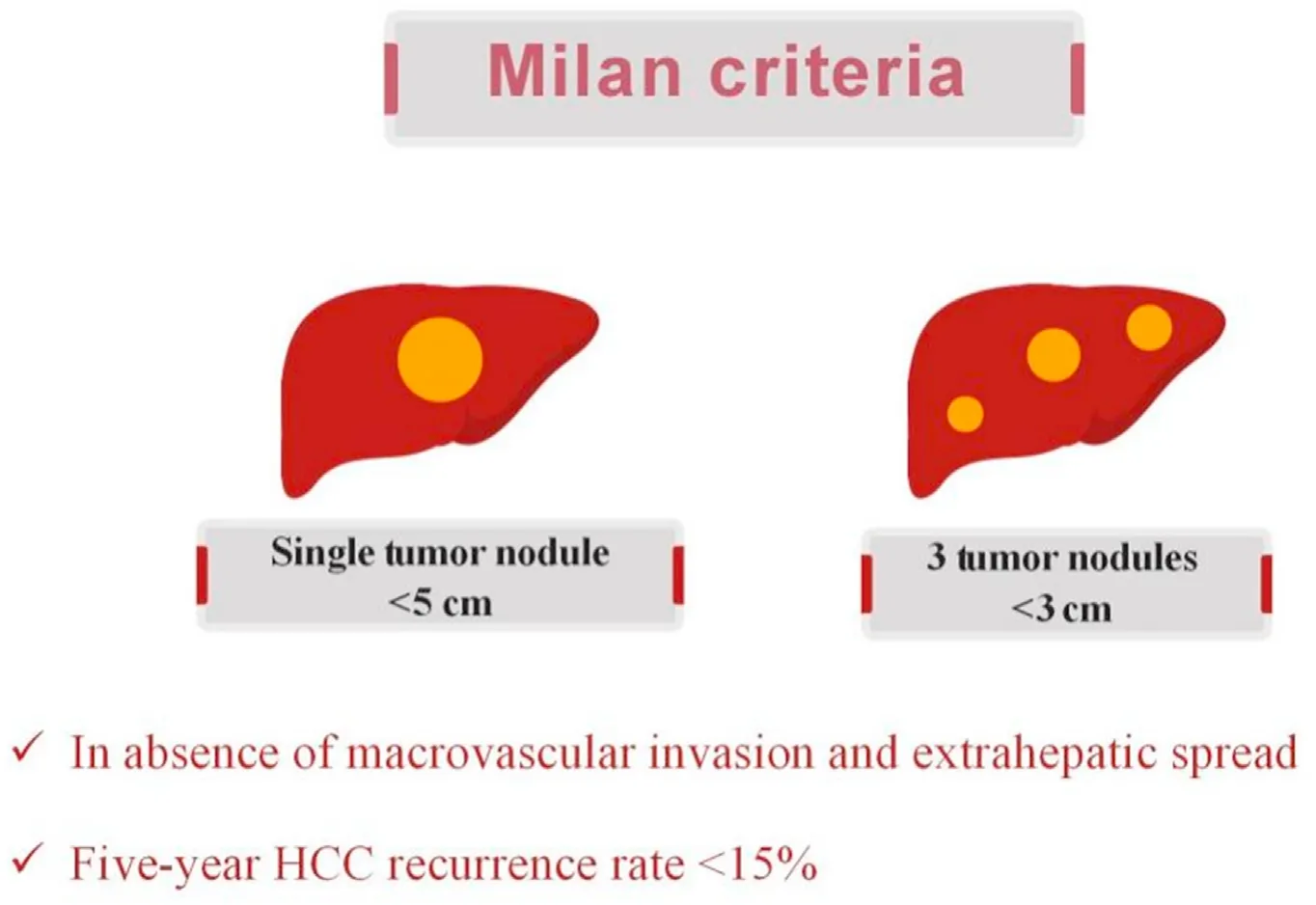
Fig.1.Milan criteria for liver transplantation as a treatment option for HCC.
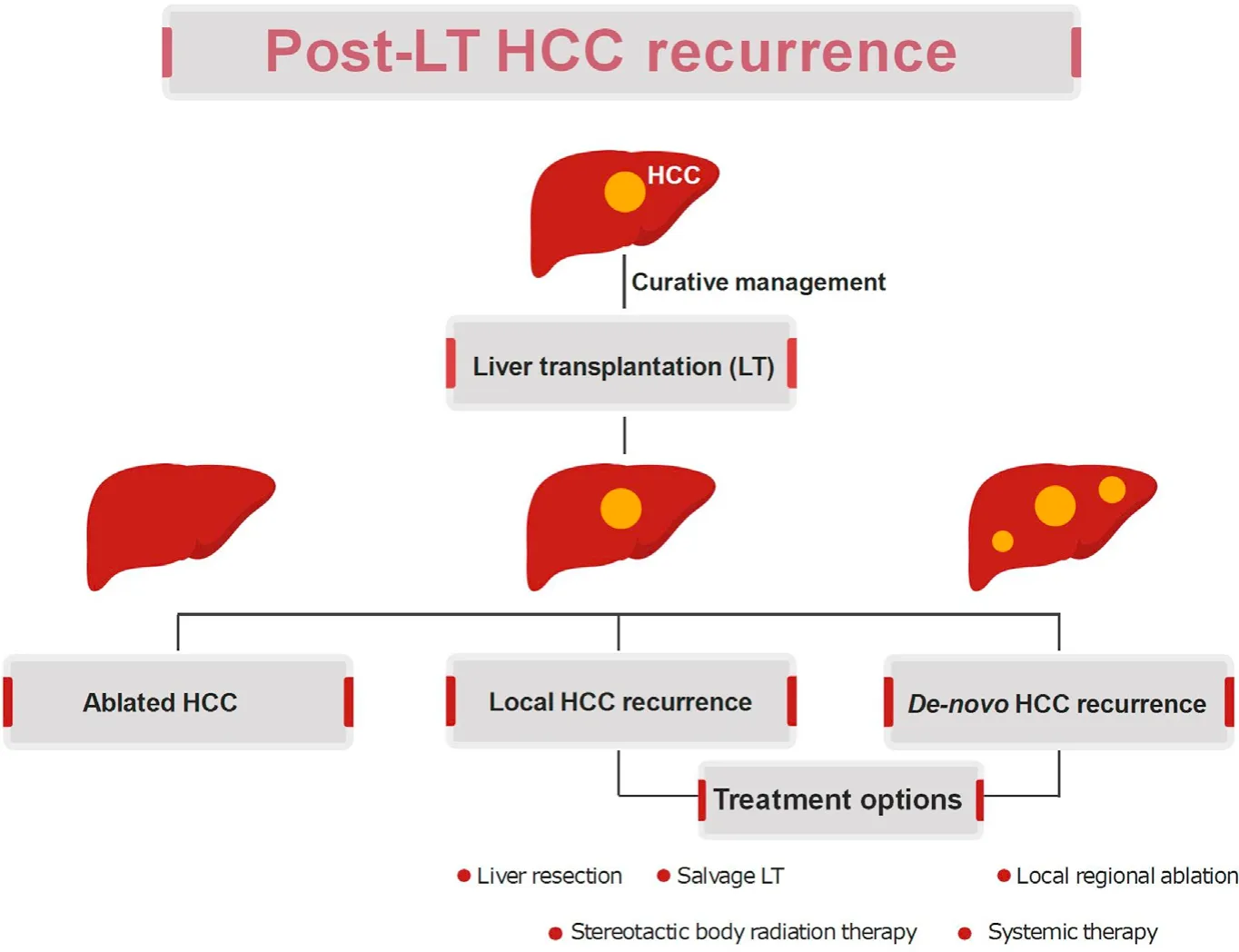
Fig.2.Patterns and treatment options for post-LT HCC recurrence.
5.2.2.Predictors of HCC recurrence post-transplantation
Some comorbidities also influence the risk of recurrence in HCC patients undergoing LT,as the obese patients show a significantly higher frequency of microvascular invasion,higher recurrence rates,and lower recurrence-free survival (RFS) than the normalweight patients.85The presence of occult extrahepatic dissemination and the persistence of the etiology of liver damage (e.g.,HBV infection or HBV/hepatitis D virus (HDV) coinfection) account for the residual risk of early and late HCC recurrence,respectively.86Effective and sustained tumor downstaging with locoregional,surgical,or systemic therapies from beyond to within the Milan criteria favorably impacts the overall and tumor-free survival in transplanted patients.87Also,pretransplant cytokine profiles(such as those of B-lymphocyte chemoattractant and interleukin (IL)-12p40) and the maximum tumor diameter can provide robust prognostic information in the setting of LT for HCC with excellent efficiency in recurrence prediction for HCC patients,and also stratify the prognosis beyond the Milan criteria or the AFP model.88
Combining positron emission tomography/computed tomography (CT) imaging with MRI predicted MVI with 78.6% sensitivity and 80.0%specificity.89The assessment of AFP serum levels before LT has been suggested to identify patients at high risk of HCC recurrence since the former is a good marker of tumor differentiation and vascular involvement.90Strong predictors of HCC recurrence have been proposed to include increasing AFP levels to>15 ng/mL,>50 ng/mL/month,or 0.1 ng/mL/day during the LT waiting period.91-93A multivariate analysis revealed that an AFP value at transplant of >25.5 ng/mL was strongly predictive of post-LT HCC recurrence.94However,there is no consensus on the applicable cut-off value for AFP to improve patient selection and the planning of proper HCC recurrence surveillance after LT.94AFP values between 16 ng/mL and 320 ng/mL seem to be associated with poor post-LT outcomes.95In a recent retrospective study of 3819 patients who underwent LT in downstaging groups,AFP<100 ng/mL was the only independent predictor of HCC recurrence.96Moreover,it has been demonstrated that extremely elevated pre-LT AFP levels (>1000 ng/mL) are associated with the worst post-LT survival rates,regardless of the tumor burden.97HCC severity,as evidenced by the presence of intrahepatic metastases,capsule infiltration,and portal vein invasion,is correlated with elevated blood DCP levels.98Lower-grade differentiation and more frequent MVI were observed in HCC,which expressed normal levels of AFP and elevated levels of DCP.99These factors have suggested that DCP better predicts post-LT HCC recurrence than AFP.100In the U.S.,a retrospective study in which AFP and DCP were combined to predict HCC recurrence found that serum levels of AFP(250 ng/mL)and DCP (7.5 ng/mL) were associated with a higher risk of recurrence.101C-reactive protein (CRP),another systemic inflammatory biomarker produced by hepatocytes,has been associated with HCC.102High serum CRP levels are strongly associated with a greater risk of HCC recurrence in patients outside the Milan criteria in a few Asian studies.103The neutrophil-to-lymphocyte ratio(NLR)and platelet-to-lymphocyte ratio (PLR) are two inflammatory markers involved in the determination of HCC prognosis in recent reports.104A considerable rise in the rate of post-LT HCC recurrence has been linked to high PLR.105
Regarding recipient age,studies have reported that elderly patients who underwent LT experienced lower survival rates and higher rates of HCC recurrence.106In general,HCC patients aged>65-70 years are not considered eligible for LT.107LT patients aged>70 years had worse survival rates and greater rates of HCC recurrence.85The most probable hypothesis is that advanced age is associated with immunosuppression,which hinders the development of neoplastic cell clones and would be more evident during prolonged immunosuppressive therapy.108Calcineurin inhibitor(CNI) therapy is associated with a higher tumor recurrence risk,specifically if there are high serum concentrations of these medications in the first few months following transplantation,according to other retrospective investigations.109Research has also shown a direct link between CNI direct dosages and a higher risk of posttransplant HCC recurrence.110Immunosuppressive regimens based on the mechanistic target of rapamycin (mTOR) inhibitors,sirolimus and everolimus,have been created to circumvent this obstacle.111The growth of human malignancies,including HCC,has been associated with mTOR dysregulation,which plays a critical role in the regulation of numerous fundamental cell functions.111-113The expression of mTOR is abnormally upregulated in a considerable portion of HCC mutations,and tumors with enhanced mTOR signaling have recently been identified as a subset of aggressive malignancies.4,114,115In vitroand animal models have demonstrated that mTOR inhibitors,unlike CNIs,suppress the growth of HCC.116The combination of sorafenib and anti-mTOR can manage post-LT HCC recurrence with the probability of severe adverse events.116Although this time frame varies,several studies have found that HCC recurrence peaks between two-year and three-year following LT,and after five-year,recurrence becomes extremely rare.117The time to recurrence is a significant prognostic factor since post-LT HCC recurrence has a detrimental effect on OS.117A worse prognosis is associated with early(within 12 months after LT) HCC recurrence.117Recurrence that occurs a year of LT is associated with a better prognosis and a five-year survival rate of about 50%.118These studies strongly recommend keeping stringent HCC recurrence surveillance systems for the first three years following LT,extending up to the fifth year.119In addition to AFP serum tests,most LT centers recommend performing total body contrast CT or MRI scans every six months for at least three years,extending to five years after LT.117The adverse effects of sorafenib may limit its use after LT,and its safety is a concern.120Figure 2 summarizes patterns and treatment options for post-LT HCC recurrence.
5.3. HCC recurrence after ablation therapies
5.3.1.RFA
Over the past ten years,RFA has been routinely used to treat HCC.121It provides a minimally invasive and potentially curative option for early HCC when resection is not feasible.121,122RFA is preferable to surgical resection in that it preserves more of the nearby hepatic tissues,requires fewer days of hospitalization,results in lower morbidity rates,and can be used on inoperable patients with liver cirrhosis.123,124However,early or late complications associated with mechanical or thermal injury during RFA have been documented during follow-up.125Aggressive tumor recurrence after RFA has recently attracted attention since it can decrease patients’ OS rates.126After ablation,frequent local tumor progression (LTP) is closely associated with tumor recurrence.127The previously reported five-year LTP rates vary from 3.2% to 27.0%,and following a mean follow-up period of 38 months,the incidence of HCC recurrence reached 63.3%.127,128
Per the findings of other studies,the rate of aggressive tumor recurrence following RFA for HCC is extremely low,falling between 0.8% and 10.0% and going as high as 15.0% in patients with periportal HCC locations.126,129There are currently some risk factors for aggressive HCC recurrence after RFA,which include larger tumor sizes,poorly defined tumor margins,elevated serum DCP levels,fast incremental upsurges in RF electrical power,periportal localizations of the lesions,the youthfulness of patients and increased expression levels of hypoxia-inducible factor-1 and epithelial cell adhesion molecule in HCC residue after unsuccessful RFA.126,129-133Insufficient ablative margins,hypervascular HCC,and an unfavorable site of HCC are additional factors.According to some previous reports,periportal placement may be a significant risk factor for LTP following RFA.134,135Rapid intrahepatic dissemination,aggressive recurrence,scattered and rapid intrahepatic recurrence,early diffuse recurrence,diffuse intrahepatic recurrence,rapid and aggressive tumor progression,and aggressive intersegmental recurrence(AIR)are a few terms used to describe aggressive tumor recurrence after RFA.126,129,130,132,136-138To prevent post-RFA aggressive tumor recurrence,especially in patients with periportal tumors,some modified ablation approaches such as the use of sinusoids,the no-touch multipolar ablation technique,more extended ablation times at lower power,and combined TACE/cryoablation with RFA were investigated.131,139-141However,as adjuvant therapy after ablation,sorafenib did not improve RFS.142
5.3.2.MWA
MWA is another modality of thermal local ablation for HCC,which depends on the creation of electromagnetic waves that cause dipole water molecules to continually move at a rate of billions of times per second with an oscillating electric field that produces heat.11Theoretically,MWA outperforms RFA in several ways,including a reduction in the “heat sink” phenomenon,reduced tissue charring during ablation,a more extensive ablation zone,and more profound,faster penetration with a brief ablation time.143-145Additionally,the updated MWA machines have a cutting-edge shaft with a cooling system to avoid temperature increments and prevent skin burning.146Large ablation zones can be created more efficiently by increasing the energy given to the target.146With the introduction of the new technology,large HCC lesions (up to 8 cm in size) might accomplish over 80% of complete ablation.147Recurrence can occur,which is a big problem even though more patients choose MVA with satisfactory complete ablation.148A total recurrence rate of 30.7% was recorded in one study (13.4% within the same lesion and 17.3% in new sites).149Newly detected lesions on CT that displayed enhancement in the arterial phase and washout in the delayed phase were considered tumor recurrence.150
Patients with a hepatic focal lesion (HFL) larger than 4 cm(37.9%) experienced recurrence at a much higher rate than those with an HFL of 4 cm(13.6%).149The substantial correlation between the tumor size and the relapse rate was acknowledged.151Patients with numerous hypervascular nodules experienced a significantly greater recurrence rate.149This is in line with the findings of Toshimoriet al.,152who noted that numerous nodules,hypervascular lesions,and HFL >2 cm had a significantly higher recurrence rate.
5.3.3.TACE
TACE is currently the recommended treatment method for patients with large or multinodular HCC and conserved liver function but no cancer-related clinical manifestations and signs of vascular invasion or extrahepatic spread.153,154According to the BCLC staging system,these patients are considered to have intermediatestage liver cancer.TACE can improve a patient’s probability of survival by maintaining their liver function and treating asymptomatic multinodular tumors without MVI or extrahepatic spread.155,156
Recent studies have demonstrated that in patients with multinodular HCC without vascular invasion or extrahepatic dissemination,the combination of TACE and sorafenib resulted in better clinical outcomes than TACE alone.156,157The most common TACE strategy,conventional TACE(cTACE),is the selective obstruction of tumor-feeding arteries via the injection of chemotherapeutic agents (doxorubicin or cisplatin) mixed with lipiodol that leads to ischemic necrosis of target tumors by cytotoxic and ischemic effects.158However,introducing the embolic drug-eluting bead(DEB)has offered a smart substitute for traditional techniques.158Some research reports have demonstrated that,compared to standard cTACE,DEB loaded with doxorubicin has a safe pharmacokinetic profile with decreased systemic exposure to the drug and much less hepatic damage.159,160Despite the theoretical advantages of DEBTACE,it is still controversial in clinical practice whether DEBTACE is superior to cTACE regarding OS and treatment response.161The effectiveness of TACE is constrained,and a quick return after this therapy can worsen the prognosis.162Increased vascular endothelial growth factor (VEGF) synthesis and the ensuing angiogenesis are characteristics of post-TACE tumor recurrence.163Additionally,TACE stimulates the countenance of other proangiogenic mediators(such as hypoxia-inducible factor 1)and boosts VEGF expression in the remaining surviving malignant tissue.163,164Although TACE causesin situnecrosis,it may also foster conditions that allow for(or even promote)angiogenesis.165
Previously,a Cochrane Meta-analysis questioned the validity of the evidence proving the advantages of TACE.166According to this Cochrane review,no proof exists that TACE improves participants’chances of surviving with unresectable HCC.166However,more recent data showed that the use of new approaches like degradable microspheres and efficient biomarkers for monitoring efficacy,will improve the outcomes of TACE,and may even turn it into a curative intervention.167
5.4. HCC recurrence after systemic therapy
Since there are defects in surveillance and diagnostic tools for HCC,it is typically detected at an advanced stage.168About 60%-70% of patients had primary advanced,incurable,recurring,or metastatic disease at the moment of diagnosis.169The median survival after diagnosis ranges from 6 months to 12 months when palliative care is administered at an advanced stage.170Systemic chemotherapy has been associated with low survival benefits,high rates of systemic toxicities,and adverse effects.171HCC is frequently described as a chemoresistant malignancy,irrespective of numerous suggested chemotherapy plans.172,173However,patients with advanced-stage HCC may benefit from systemic therapy.174Sorafenib,an oral tyrosine kinase inhibitor (TKI),targets angiogenesis and tumor proliferation pathways by inhibiting VEGFR,platelet-derived growth factor receptor β pathways,and Raf-MEKERK signaling.175Sorafenib adjuvant therapy seems to have the potential to be beneficial.176Sorafenib was found to be both safe and effective in a phase I trial including 14 patients,with a single reported death and four cases of recurrence observed after an average follow-up period of 32 months.176Dose reduction is necessary for more than half of sorafenib-treated patients with recurrent HCC.120,177After dosage reductions or treatment discontinuation,the disease progresses in many patients on sorafenib.178Additionally,sorafenib did not initially work for 27%of the patients in the Sorafenib HCC Assessment Randomized Protocol (SHARP)study.179Postsorafenib survival was substantially correlated with liver decompensation,performance status,tumor advancement,and/or extrahepatic tumor spread.180Lenvatinib,regorafenib,cabozantinib,and sorafenib are TKI medications that have increased patient survival in advanced HCC.181,182
Numerous studies assessing the function of immunotherapy in HCC have recently been conducted,and others are currently in progress.183Programmed cell death protein-1(PD-1)/programmed death-ligand 1 (PD-L1) or cytotoxic T lymphocyte-associated antigen 4(CTLA-4)are the targets of immune checkpoint inhibitors.183These medications activate the immune system’s antitumor response,enabling it to identify and eliminate cancer cells,T cells,dendritic cells (DC),and activated cytokine-induced killer (CIK)cell-based adoptive immunotherapies,as well as oncolytic virus and peptide vaccines for HCC,have all been shown to be safe and effective in clinical trials.183-188
PD-1 inhibitors,nivolumab and pembrolizumab,received the U.S.Food and Drug Administration’s(FDA)approval as second-line options for HCC treatment following sorafenib after the success of phase II clinical studies,CheckMate 040 and Keynote 224.189,190Sadly,pembrolizumab did not show a statistically significant advantage over placebo in progression-free survival (PFS) or OS according to the phase III study Keynote 240.191
Following the IMbrave150 trial’s successful conclusion,improved HCC management recently advanced substantially.192The combination of atezolizumab (an anti-PD-L1) and bevacizumab (an anti-VEGF monoclonal antibody) is superior to sorafenib in first-line therapy,more than ten years after sorafenib was approved.192Adjuvant adoptive cellular immunotherapies have been shown to enhance RFS and OS in patients with HCC following ablative therapy in numerous trials.186Cryoablation plus DC-CIK cell immunotherapy significantly increased OS for patients with metastatic HCC compared to either cryoablation alone (median:17.5 months) or the untreated group (median: 3 months).193To date,only a few studies could report definitively observed HCC recurrence patterns after systemic therapies due to high rates of morbidity and mortality among patients with advanced HCC besides high rates of adverse effects of drugs,be they novel or approved.
6.Prevention of HCC recurrence
The prevention of HCC recurrence is challenging;however,several studies have discussed a wide range of chemo-preventive options,such as:
-The long-term oral intake of branched-chain amino acids(BCAA) granules in patients who underwent RFA led to a reduction in the cumulative relapse rate and an improvement in the OS.194,195The OS and RFS improved with oral BCAA granule delivery,according to Nishikawaet al.’s194retrospective study of 256 patients with RFA and blood albumin levels of ≤3.5 g/dL.BCAA granule administration can also hasten the recovery of protein metabolism following hepatectomy.196According to Ichikawaet al.,197BCAA granules significantly prevented early recurrence following hepatectomy.Additionally,it has been demonstrated that the administration of BCAA granules before TACE prevented the decline in blood albumin levels three and six months following TACE and supported the maintenance of residual liver function in Child-Pugh A and B patients.198When sorafenib is utilized,BCAA granule delivery prevents the decline in serum albumin levels and prolongs survival.199
-Several Meta-analyses have reported the effectiveness of interferon (IFN) as an antiviral therapy for HBV and/or HCV-related HCC.200,201IFN may potentially prevent postoperative recurrence when used in conjunction with the Milan criteria,and the prolonged virological response was explicitly linked to this possibility.201
-Nucleic acid analogs are recommended for patients with HBVrelated chronic liver disease following HCC treatment to limit HCC recurrence and enhance prognosis.202
-A report on the impact of IFN following radical therapy for HCVinduced HCC found a trend in suppressing recurrence;however,the findings were not statistically significant.203After aggressive treatment for HCC,multiple studies have found that IFN reduced the rate of further recurrence after a second recurrence.204A multicenter prospective analysis negated the role of direct-acting antivirals(DAAs)inpromoting HCC recurrence,even though most studies reported a significant recurrence rate following elimination by DAAs.205The prevention of HCC’s arms is depicted in Fig.3.
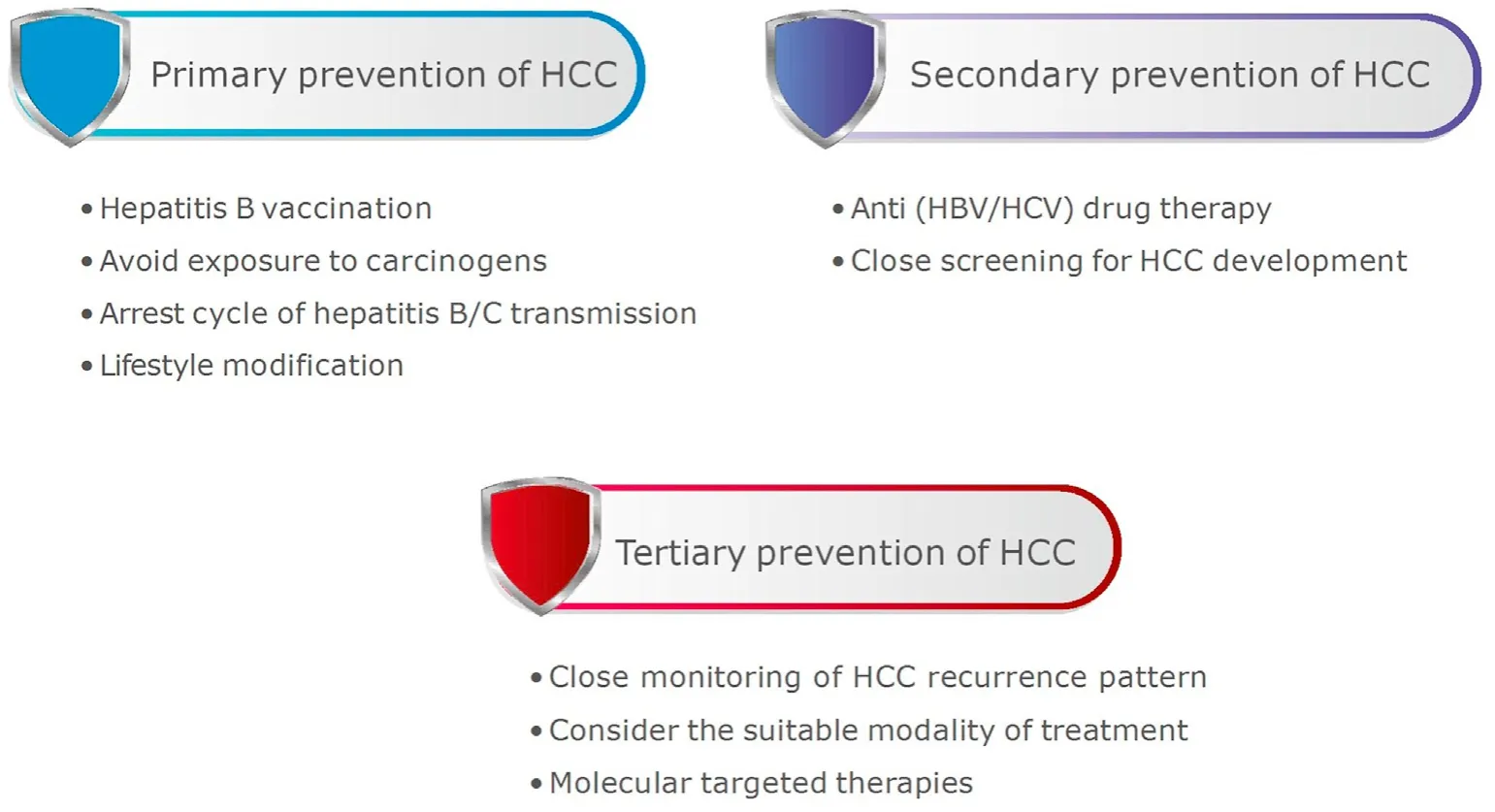
Fig.3.Arms of HCC prevention.
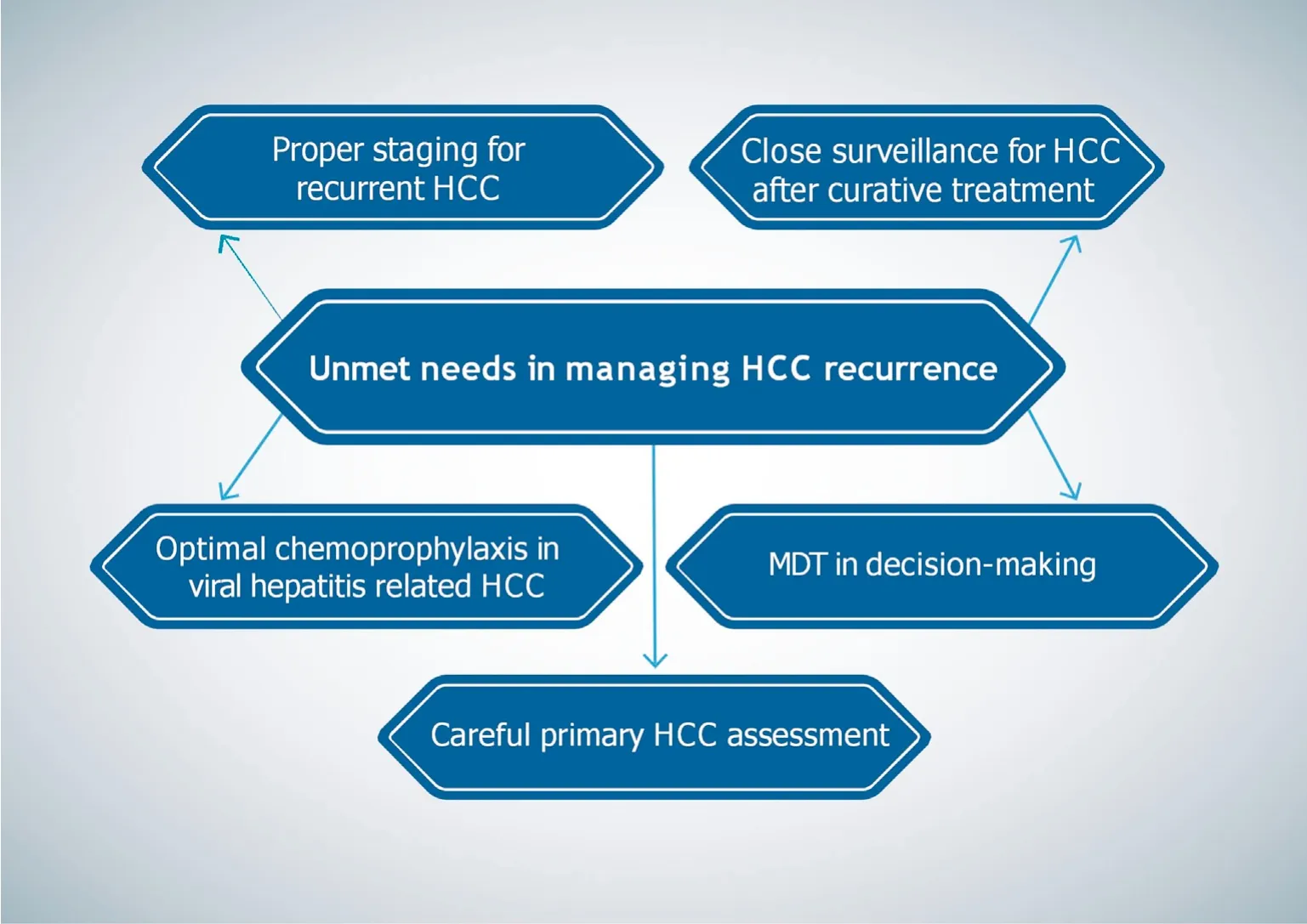
Fig.4.Unmet needs of the management of HCC recurrence.
-An RCT was conducted on patients receiving HCC radical curative treatment to see if sorafenib may stop the recurrence of the disease.206There were two groups in this study (the STORM trial): one comprising patients who received sorafenib at 800 mg/d and the other made up of patients who received a placebo;nevertheless,sorafenib had no discernible prolonging effect.18Due to the high rate of unfavorable side effects,the long-term oral administration of sorafenib proved impractical in the STORM study.18
-Peretinoin is an oral acyclic retinoid with a structure resembling that of vitamin A that works by binding to the retinoid nuclear receptor.207According to a small-scale RCT that examined the impact of peretinoin on the prevention of HCC recurrence following radical treatment,the drug was able to reduce the rate of a second recurrence (adjusted relative risk: 0.31;95%CI:0.12-0.78).208
-Additionally,deferoxamine (DFO) has been shown to have an anticancer impact in patients with HCC.209DFO was shown to decrease hepatic fibrosis and precancerous lesions in a liver cancer rat model.210
7.Conclusions:unmet needs in managing HCC recurrence
HCC recurrence is still a concern despite improvements in OS,which demands a careful reevaluation of the patient and disease condition before retreating.To manage HCC recurrence properly,appropriate staging is essential.Optimal chemoprophylaxis in viral hepatitis-induced HCC should be offered from the start.Close imaging surveillance is required after curative-intent treatment to detect possible recurrence early.The timing of surveillance should be determined based on primary tumor characteristics.The decision-making process for the management options at the recurrence time must exclude extrahepatic spread and select possible candidates for repeat therapies with a curative objective.Repeated liver resection or ablation may benefit those with stillpreserved liver function.Individualized and evidence-based decision-making is required to get the best results for individuals with recurrent HCC.Even though LT is the most effective therapy for treating HCC,it still has some limitations,the most notable of which is the possibility of tumor recurrence.To enhance patient outcomes,considerable effort still needs to be made,and progress is still needed.Careful patient selection and stratification are crucial points.Pretransplant prognostic models should be more validated.
There is currently no standard surveillance strategy for transplanted patients to detect post-LT HCC recurrence.Further research on adjuvant therapy after curative HCC treatment should be encouraged.Proper screening programs and HCC detection have to be optimized in different healthcare centers.Large-cohort studies are needed to investigate the benefits and risks of combining different HCC treatment modalities as a definitive solution to minimize recurrence.Patients with HCC should be evaluated adequately before liver resection to identify predictors of recurrence.Immunotherapy in HCC still requires more research to maximize its use,either as an additional therapeutic agent after curative treatment or as a sole therapy.Figure 4 illustrates the unmet needs of the management of HCC recurrence.
Authors’ contributions
Mohamed El-Kassas: Conceptualization,Writing-Reviewing and Editing;Walaa Abdelhamed: Data curation and original draft preparation.Both authors read and approved the final manuscript.
Declaration of competing interest
The authors declare that there is no conflicts of interest.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public,commercial,or not-for-profit sectors.
- Liver Research的其它文章
- Dietary pattern and hepatic lipid metabolism☆
- In-depth analysis of de novo lipogenesis in non-alcoholic fatty liver disease: Mechanism and pharmacological interventions☆
- The contributions of bacteria metabolites to the development of hepatic encephalopathy☆
- Autophagy modulates physiologic and adaptive response in the liver☆
- Unveiling the effect of estrogen receptors in alcoholic liver disease:A novel outlook☆
- Sequential ultrasound molecular imaging for noninvasive identification and assessment of non-alcoholic steatohepatitis in mouse models☆