Effect of estrogen pretreatment in GnRH antagonist protocol-Metaanalysis
WU Ting-ting, JIANG Xin-xing, MA Yan-lin
1.Hainan Provincial Key Laboratory for Human Reproductive Medicine and Genetic Research, the First Affiliated Hospital of Hainan Medical University, Hainan Medical University, Haikou 570000, China
2.Department of Reproductive Medicine, the First Affiliated Hospital of Hainan Medical University, Hainan Medical University, Haikou 570000,China
3.Hainan Provincial Clinical Research Center for Thalassemia, the First Affiliated Hospital of Hainan Medical University, Hainan Medical University, Haikou 570000, China
4.Key Laboratory of Tropical Translational Medicine of Ministry of Education, Hainan Medical University, Haikou 570000, China
5.Haikou Key Laboratory for Preservation of Human Genetic Resource, the First Affiliated Hospital of Hainan Medical University, Hainan Medical University, Haikou 570000, China
Keywords:
ABSTRACT Objective: To evaluate the effect of estrogen pre-treatment in patients with different ovarian response in antagonist protocol.Methods: Randomized controlled trials (RCTs)and retrospective studies about the effect of estrogen pre-treatment in antagonist prorocol were searched in PubMed, Web of Science, China National Knowledge Infrastructure,Wanfang Database.R software was used for meta-analysis.Results: Seven RCTs and two retrospective studies were included.In order to explore the source of heterogeneity, subgroup analysis was used, which was mainly conducted according to the ovarian response of the included population, which were divided into low responders, non-low responders and mixed responders.In the study about gonadotropin hormone (Gn) days, patients were divided into wash-out subgroup and non-wash-out subgroup according to drug use-pattern.Meta-results showed that the number of Gn days increased significantly in the non-wash-out subgroup(WMD=1.07, 95%CI[0.83; 1.31], I2= 66%).The number of Gn days in the wash-out subgroup were not affected (WMD = -0.12, 95%CI [-0.45; 0.21], I2 = 0%).In the low-response subgroup,the number of oocytes retrieved (WMD = 0.46, 95% CI [-0.23;1.16], I2 = 81%) , the fresh cycle clinical pregnancy rate (RR = 0.77, 95%CI [0.55; 1.06], I2 = 73%) and the cycle cancellation rate (RR = 0.80, 95%CI [0.40; 1.61] , I2 =83%) were not significantly changed with estrogen pre-treatment.In the non-low-response subgroup, the number of oocytes obtained (WMD =0.21, 95%CI [-0.69; 1.11], I2=2%), fresh cycle clinical pregnancy rate (RR=0.94, 95% CI [0.77;1.14], I2=41%), live birth rate (RR=0.82, 95% CI [0.62; 1.08], I2=0%) and cycle cancellation rate (RR=0.89, 95%CI [0.54; 1.47], I2=2%) were not significantly changed with estrogen pretreatment.Conclusions: Estrogen pre-treatment (with non-wash-out period) in antagonist protocol increases Gn days , dose not improve IVF outcomes in non-low responders and low responders.
1.Introduction
Assisted reproductive technology (ART) is an important means to solve the problem of Infertile couple.Controlled ovarian hyperstimulation (COH) is a major method for appropriate quantity and quality of oocytes, which is a key step to ensure ART efficiency.A satisfactory COH protocol should have the following characteristics: effective follicle recruitment, patient-friendly, strong controllability, and low incidence of side-effect.
Antagonist protocol has been applied in clinical history for more than 20 years, is one of the mainstream protocol of ART.It has the advantages of short days for using Gn, high cost effective, friendly patient experience, low incidence of ovarian hyperstimulation syndrome (OHSS)[1]and suitable for different responders.There are high quality meta analysis showing no significant difference in live birth rate with the antagonist protocol compared to the gonadotropinreleasing hormone agonist (GnRH-a) protocol[2].As well known,during the phase of antral follicles recruitment , the synchrony of antral follicles has an important influence on the rate of follicle output and the number of eggs obtained.
Because antagonist protocol does not use GnRH-a, the promotion time window for Gn is usually limited to cycle day1 to day 3 or even shorter.This results in poor follicular synchronization and leading to the reduction of ovulation number and even the cancellation of cycle which significantly reduces the successful efficiency and flexibility of the antagonist protocol.A certain number of eggs is exactly the basis of improving the live birth rate, especially in the people with reduced ovarian function and low response, the reduced number of oocytes or the increased cancellation rate due will have a negative impact on the cumulative live birth rate.Renato Fanchin firstly proposed that in the late luteal using estrogen to inhibit the rise of endogenous FSH would promote antral follicle synchrony[3].The idea is based on the following endocrine mechanisms: the recruitment of antral follicles often occurs in the late corpus luteum of the previous menstrual cycle[4], which the luteal function will decreased in this phase if not pregnant.The gradual degeneration of the corpus luteum decreases the estrogen and progesterone, that negative feedback drives the pituitary (f ollicle stimulating hormone,FSH) increase secreting FSH, resulting in some follicles with low FSH threshold at this stage may begin to recruit growth making follicles asynchronous.The use of estrogen in the late luteum can reduce the level of pituitary negative feedback secretion FSH, which can inhibit the early recruitment of follicles.In the past 20 years,many scholars have been exploring the effectiveness of this theory,and we hope to further improve the effectiveness of antagonist protocol.A meta-analysis published in 2017 suggested that the effect of estrogen pretreatment in the antagonist protocol is not clear[5], which the number of included studies was limited.In the past five years, some relevant RCT or retrospective studies results were published.Our study can comprehensively summarize the current relevant research data, and explore the effect of estrogen pretreatment in different responders using antagonist protocol, so as to provide a basis for clinical application.
2.Materials and methods
2.1 Study type and search strategy
Randomized controlled trials and case-control studies about the effect of estrogen pre-treatment in antagonist protocol were included.The PubMed,Web of Science, China National Knowledge Infrastructure, Wanfang Database were searched studies that were published between January 1990 and February 2023 with the following keywords combined: ‘GnRH antagonist', ‘pre-treatment',‘estrogen', ‘estradiol', ‘in vitro fertilization', ‘IVF', ‘ICSI'.
2.2 Eligibility and exclusion criteria
The following criteria were used to select eligible studies: 1,randomized controlled trials or case-control studies focused on the effects of a GnRH antagonist protocol with or without estrogen pre-treatment; 2, Studies with different ovarian responses: high responders, low responders and normal responders; 3, The baseline characteristics of the control group and the experimental group were generally consistent, with complete data analysis, including Gn days , Number of oocytes, clinical pregnancy rate, live birth rate, cancellation rate.The following criteria were used to exclude unqualified studies: 1.Studies did not have the control group; 2,Studies that pre-treatment combined with other drugs; 3.Studies with non-antagonist protocol; 4,Studies that had the incorrect data, raw data cannot be accessible and were less than 7 of the study quality score; 5, Case reports, and review articles were excluded.
2.3 Quality assessment
The Cochrane risk-of-bias tool were used to evaluated the quality of RCT published by Higgins JPT[5], which includes six domains:1, adequate sequence generation; 2, allocation concealment; 3,blinding; 4, incomplete outcome data addressed; 5, free of selective reporting; 6, other issues.
The study quality assessment was A if each evaluation was “low risk”, otherwise was B.The case-controlstudy was evaluated by using the Newcastle-Ottawa scale.Those who met the evaluation entry received “*” got 1 point , and the cumulative score was the study quality score.All data were extracted independently by two researchers and discussed if there was any controversy.
2.4 Statistical analysis
R software was used to conduct all the analyses in this study.Counting data were expressed by risk ratio (RR), and the measurement data were expressed by weighted mean difference(WMD) with 95% confidence interval (CI).The inspection level α is set to 0.05.Cochrane's I2statistics was used to estimate the heterogeneity between the studies.Random effect model analysis was chosen when I2value was more than 50%, otherwis fixed effect model was chosen.In order to further explore the source of heterogeneity, subgroup analysis were used, mainly according to the ovarian respondse( divided into low responders, non-low responders and mixed responders), and the drug use patternsdivided into washout group (stop estrogen pre-treatment 5~6 d to start Gn) and nonwash-out group (estrogen pre-treatment for the day before Gn start)for analysis.The stability of the results was verified by calculating the effect size after excluding each study separately.
3.Results
3.1 Study characteristics
According to the above search strategy, the literature was searched,and a total of 58 subject-related documents were preliminarily selected by reading the full text.Literature screening was based on the criteria in the study method, and a total of 11 articles were eligible, including 7 RCT studies[3, 7-12], 4 retrospective studies[12-15].There were two retrospective studies excluded because of error data and low quality scores[13, 15].Nine studies were included for analysis, all RCT studies were assessed as B, and all retrospective study quality score was 8.The nine studies were characterized as follows:1, publication was between 2003 and 2022; 2, including 1 037 participants in the treatment group and 1 058 participants in the control group; 3, There was a study result which is included the low responders and non-low responders[14]; 4, There was a study that focused on the low responders who were younger than 35 years old[16]; 5, All studies were pre-treated with oral 17β-estradiol or estradiol valerate 4mg for 6-15 days, with a wash-out period(5-6 days ) after estrogen use only in two RCT studies[7, 10], and the rest studies' pre-treatments were used until the day before the Gn start day.There was a RCT study used menotrophin[17], and the remaining eight studies all used recombinant FSH for ovulation induction, with a starting dose of 300 IU for low responders and 150~300 IU for non-low responders, using a flexible or fixed antagonist protocol; 6,All nine studies were fresh cycles, with fresh embryos transfered on 2~5 d.
3.2 Meta~analysis results
3.2.1 Gn Days
Eight articles reported Gn days with the WMD was 0.80( 95%CI[0.43; 1.17], I2= 89% ).There was significant increase in Gn days in the pre-treatment group compared with the control group.The results of the subgroup analysis showed the non-wash-out subgroup WMD was 1.07( 95%CI [0.83; 1.31], I2=66%) ; the wash-out subgroup WMD was -0.12( 95%CI [-0.45; 0.21], I2= 0% ).It suggested that the Gn days of treatment group were significantly more than those in the control group in the non-wash-out subgroup, no statistically significant difference between the treatment group and the control group in the wash-out subgroup (Figure 1).
3.2.2 The number of oocytes and the fresh cycle clinical pregnancy rate
Seven articles reported the number of oocytes with the WMD was 0.38 ( 95%CI [-0.14; 0.89], I2= 56%), which suggested that was not significantly different in the number of oocytes.We further performed a subgroup analysis according to the ovarian response,which showed the WMD in low responder was 0.46 ( 95%CI [-0.23;1.16], I2=81%) ; the WMD in the non-low responders was 0.21 (95%CI [-0.69; 1.11], I2=22% ), suggesting that was not significantly different in the number of oocytes (Figure 2).
Eight articles reported fresh cycle clinical pregnancy rate /initiation cycle, showing RR was 0.91 ( 95%CI [0.77; 1.06], I2=45% ), suggesting that was not significantly different in the clinical pregnancy rate / initiation period..No significant difference was detected for the subgroup, RR in the low responders was 0.77 (95%CI [0.55; 1.06], I2=73% ); RR in the non-low responders was 0.94 ( 95%CI [0.77; 1.14], I2=41% ); RR in the mixed responders (1 RCT) was 1.33 ( 95%CI [0.70; 2.54] )(Figure 3).
3.2.3 Fresh cycle live birth rate and cycle cancellation rate
Three articles reported the fresh cycle live birth rate / start cycle.No significant difference was detected for the non-low responders, RR was 0.82(95%CI [0.62; 1.08], I2= 0%) (Figure 4).Cycle cancellation rate was reported in seven articles, and the results showed that RR was 0.86(95%CI [0.58; 1.28], I2=28% ), suggesting no significant difference.No significant difference was detected for the Subgroup,RR for the low responders was 0.80 (95%CI [0.40; 1.61], I2=83%);RR for non-low responders was 0.89 (95%CI [0.54; 1.47], I2=2%);the RR for the mixed responders (1 RCT) was 0.91(95%CI [0.19;4.29]) (Figure 5).
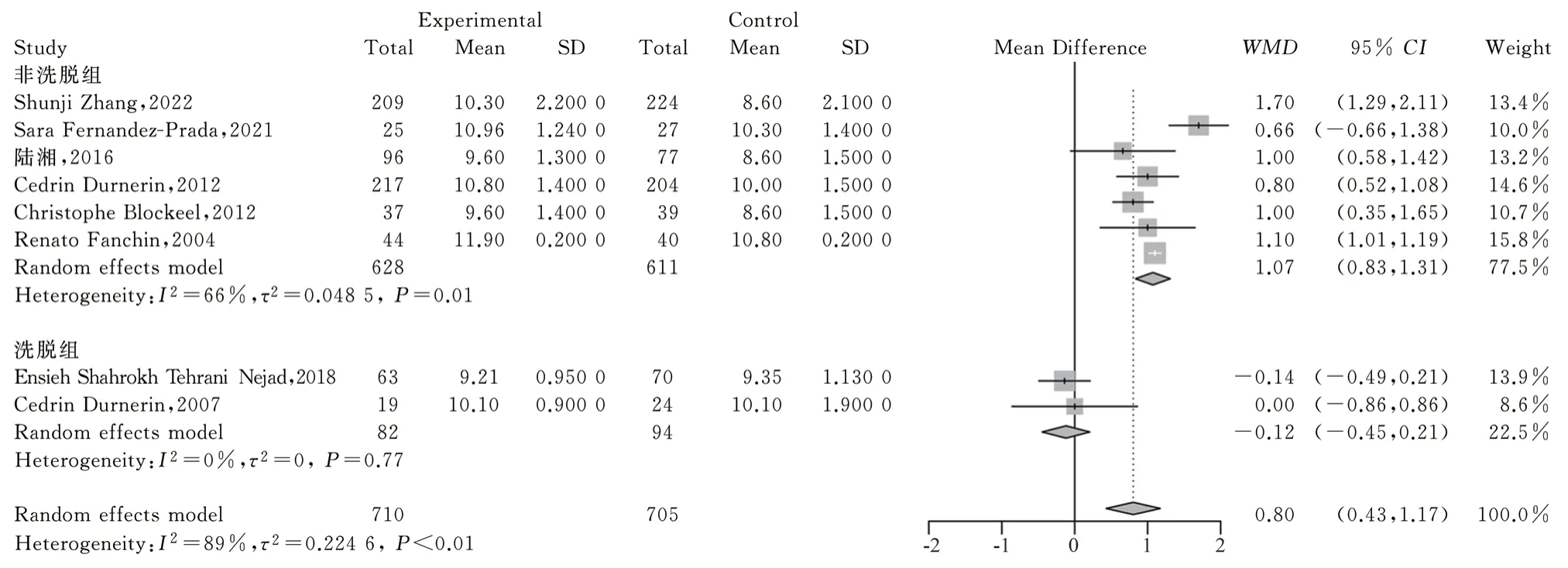
Fig 1 Forest plot for different drug use pattern in Gn days
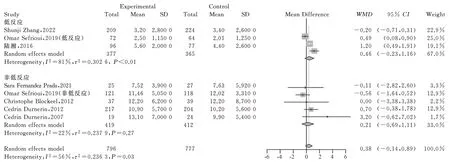
Fig 2 Forest plot for different responders in number of the oocytes
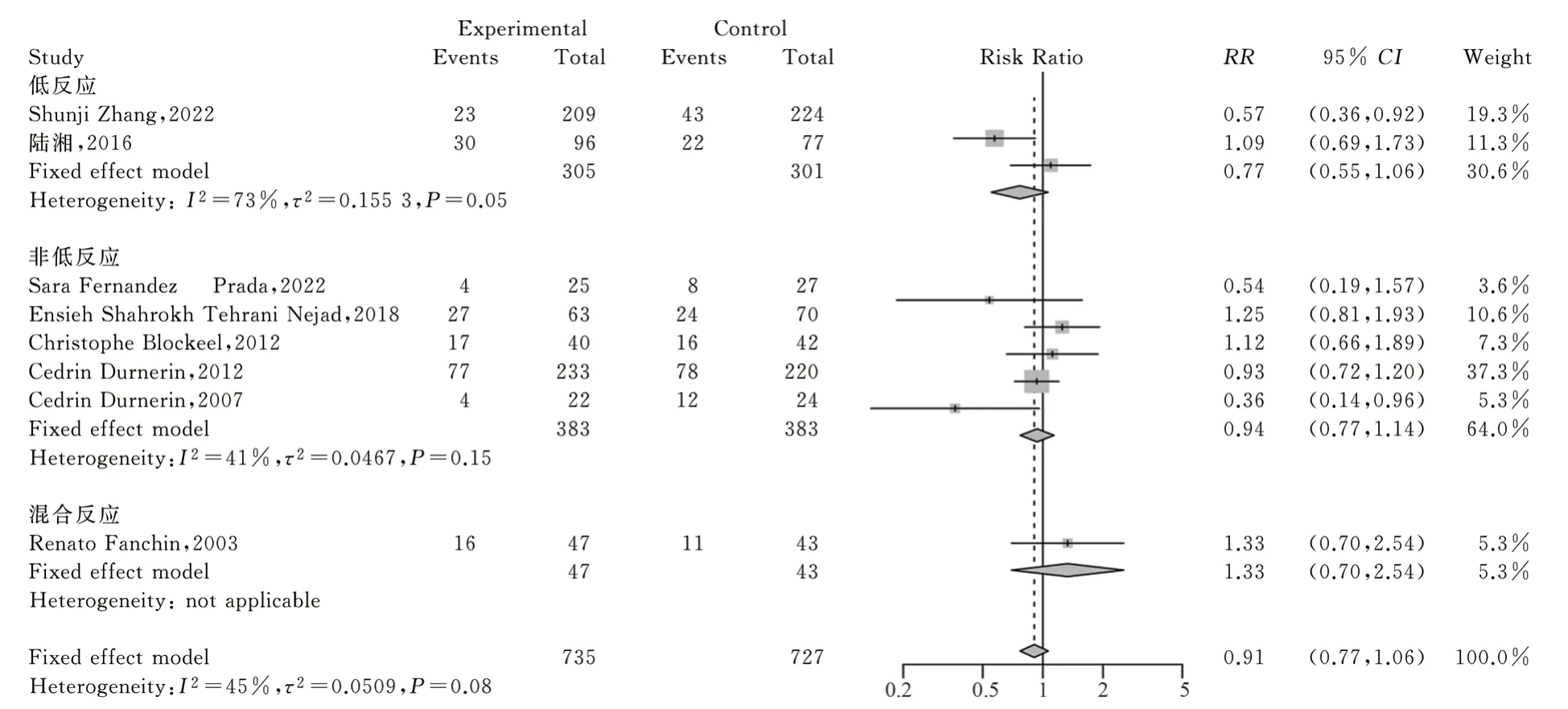
Fig 3 Forest plot for different responders in the fresh-cycle clinical pregnancy rates
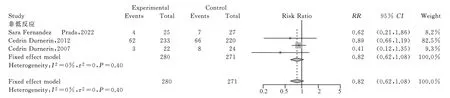
Fig 4 Forest plot for different responders in the fresh cycle live births
3.3 Sensitivity analysis results
In the sensitivity analysis for all above results, there were 2 abnormal results ( Table 1).When the effect value of Shunji Zhang was excluded, the and the overall WMD was 0.55 ( 95%CI [0.02;1.08]), which was statistically significant, indicating poor stability of these indicators.The results of the remaining group sensitivity analysis were similar to the original results, suggesting good stability.After removing the Shunji Zhangs' article, positive result in the number of oocyte was detected ((WMD was 0.78 (95%CI [0.10;1.47] )for the low responder) and WMD was 0.55 ( 95%CI[0.02;1.08]) for the totle group), the rest results was similar to previous result (Table 1).
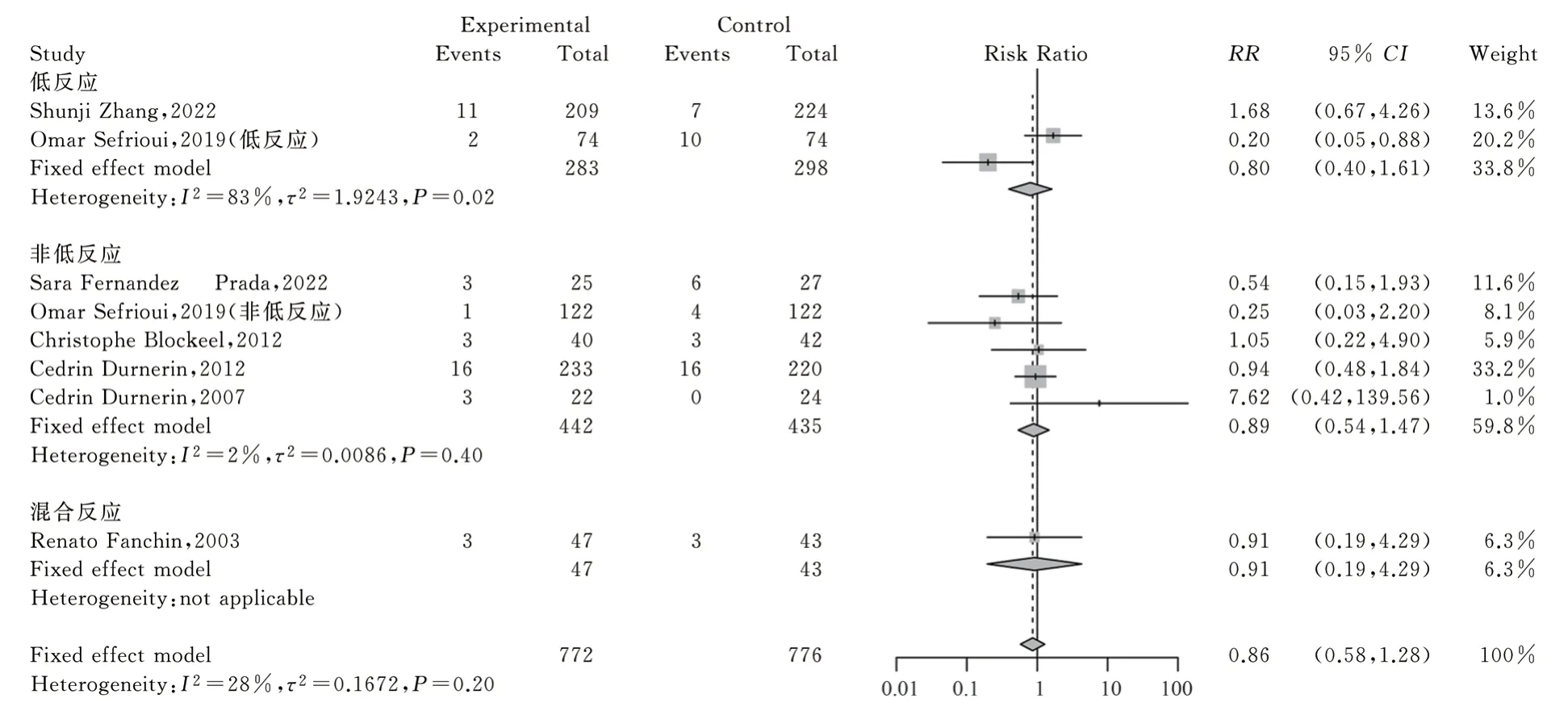
Fig 5 Forest plot for different responders in the cycle cancellation rates
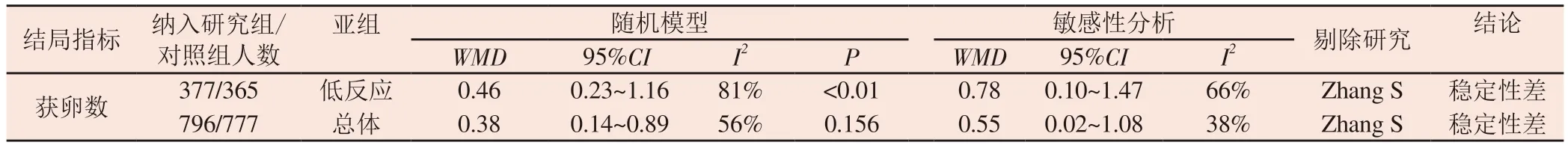
Tab 1 List of sensitivity analysis
4.Discussion
Antagonists were first used in 1999 to prevent the early luteinizing hormone (LH) peaks in superovulation.It was different from GnRH-a, which is reversible and dose-dependent by inhibiting GnRH release through competitively GnRH receptors.With several generations improvement of antagonist and increasing clinical experience, antagonist protocol can not only obtain the ideal and stable cumulative live birth rate, but also had the advantages of no flare-up effect, short treatment cycle, friendly patient experience and low risk of OHSS, which has gradually become the mainstream protocol in IVF.The results of Meta-analysis showed that there was no significant difference in the live birth rate and abortion rate and the incidence of OHSS was significantly reduced between the antagonist protocol and GnRH-a protocol[2].However, the deficiency was the insufficient flexibility and the number of oocytes which may be slightly reduced compared to the agonist protocol[18, 19].The reason may be asynchronous of the antral follicles and low ovarian responsed.In IVF patients with less than 15 oocytes retrieved, there was a strong positive correlation of live birth rate and the number of oocytes retrieved[20].Reducing the cycle cancellation rate could help to further improve the efficacy and cost-effectiveness of IVF therapy.Therefore, many scholars expected to optimize the synchronicity of follicles and improve the outcome of IVF, and constantly explore the methods such as: using oral contraceptives, progesterone or estrogen pretreatment in luteal phase , antagonist or estrogen in early follicular phase, etc., but no consensus has been reached so far.Follicular recruitment is caused by a FSH transient rise during the luteal-follicular transition (LFT), and the decline in late luteal of estrogen levels was signal of FSH rise[4].The study showed that the use of physiological doses of estrogen in the luteal phase effectively reduced the level of FSH on the Gn beginning day, estrogen pretreatment reduced the follicle growth rate and differential level of antral follicle size in the Gn beginning day[2].This suggested that the IVF outcome may be optimized by pretreatment with estrogen.Some doctors have used this method to found that it could effectively avoid weekend oocytes retrieval and increase the flexibility of antagonist protocol[9, 21].The meta analysis showed increased days of stimulation, number of oocytes retrieval and mature oocytes in estrogen pre-treatment protocol in low responders[22].However,this study included a small sample of comparing short protocol and antagonist protocol that were mainly retrospective analysis.In 2017,the meta-analysis by Sisi Yi showed that estrogen pre-treatment in the antagonist protocol could increase the Gn days, total Gn doses and the number of oocytes in normal responders, and did not increase the clinical pregnancy rate, live birth rate[23], However, this meta-analysis included few studies and lacked exploration of the role in other ovarian response patients.These data seem to suggest the possibility of benefit of estrogen pre-treatment in antagonist protocol.The application of estrogen pre-treatment is common, so more comprehensive evidence is needed to justify the pre-treatment effectiveness.
The results of this study showed a significant increase for Gn days in the non-wash-out subgroup , but no significant difference in the wash-out protocol study.This suggests that there is an interaction effect between wash-out pattern and Gn days after estrogen pretreatment, and the non-wash-out pattern can increase the cost of ovulation induction in patients.The mechanism may be that washout for 5~6 d after estrogen pre-treatment can restore pituitary fuction, so there was significant difference in Gn days.Since the increase for the number of oocytes may improve the rate of live birth in the low responders, and ovarian reactivity is an important factor of the number of the oocytes , the subgroup analysis of different ovarian responders could further explore its effectiveness.Our results showed that estrogen pre-treatment did not affect the number of oocytes , fresh cycle clinical pregnancy rate, fresh cycle live birth rate and cycle cancellation rate in both low responders and non-low responders.There was only 1 RCT study in the mixed responders[25].There was no significant difference in the clinical pregnancy rate and cycle cancellation rate.The source of heterogeneity cannot be fully explained by the analysis of medication pattern and ovarian reactivity subgroup.In this study, the non-low responders subgroup had low heterogeneity, what was mainly RCT and reliable; the low responders subgroup had high heterogeneity, which was related to the different study types, age characteristics of the included population.The sensitivity analysis results for the number of oocytes in low responders subgroup and overall group showed poor stability of the results, which may be affected by potential bias factors.The current study has few data about live birth rate, abortion rate, and lacks cumulative live birth rate and so on.
In conclusion, the estrogen pre-treatment in the antagonist protocol(non-wash-out) would increase Gn days and not improve the IVF outcome of non-low responders.The pre-treatment would increase the treatment burden of patients.There seems to be no benefit in antagonist protocol for low responders, but high-quality prospective randomized controlled studies in this aspect are limited, and more rigorous and large-scale studies are needed.The antagonist protocol application of estrogen pre-treatment need thinking: there was no benefit based on the current data if we used estrogen for pretreatment generically; the current quality of RCT research mainly focus on the low responders; we expect to improve poor prognosis patients’IVF outcome , such as Patients with ovarian insufficiency,suboptimal responders and low responders; we need more high quality research answer in the future.The estrogen pre-treatment in the antagonist protocol should be cautiously applied.
 Journal of Hainan Medical College2023年17期
Journal of Hainan Medical College2023年17期
- Journal of Hainan Medical College的其它文章
- Research progress on the regulation mechanism of non-coding RNA on ankylosing spondylitis
- Anesthetic effect of phenobarbital sodium on female BALB/c mice
- Research progress of TCM regulation of Cajal interstitial cells in the treatment of functional Gastrointestinal diseases
- Abnormal expression and significance of circ-CBLB/miR-486-5p in patients with rheumatoid arthritis of spleen deficiency and dampness excess type
- Inhibitory effect of thymoquinone on neuroinflammation in Parkinson's disease model by regulating NLRP3 inflammatory bodies
- Effect of Astragalus-hawthorn on ovarian reproductive function and inflammatory mechanism of action in rats with polycystic ovary syndrome
