Inspired by novel radiopharmaceuticals: Rush hour of nuclear medicine
Yang Liu ,Ya-nan Ren ,Yan Cui ,Song Liu ,Zhi Yang ,Hua Zhu ,Nan Li
1Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing),NMPA Key Laboratory for Research and Evaluation of Radiopharmaceuticals (National Medical Products Administration),Department of Nuclear Medicine,Peking University Cancer Hospital &Institute,Beijing 100142,China;2State Key Laboratory of Holistic Integrative Management of Gastrointestinal Cancers,Beijing Key Laboratory of Carcinogenesis and Translational Research,NMPA Key Laboratory for Research and Evaluation of Radiopharmaceuticals (National Medical Products Administration),Department of Nuclear Medicine,Peking University Cancer Hospital &Institute,Beijing 100142,China
Abstract Nuclear medicine plays an irreplaceable role in the diagnosis and treatment of tumors.Radiopharmaceuticals are important components of nuclear medicine.Among the radiopharmaceuticals approved by the Food and Drug Administration (FDA),radio-tracers targeting prostate-specific membrane antigen (PSMA) and somatostatin receptor (SSTR) have held essential positions in the diagnosis and treatment of prostate cancers and neuroendocrine neoplasms,respectively.In recent years,FDA-approved serials of immune-therapy and targeted therapy drugs targeting programmed death 1 (PD-1)/programmed death ligand 1 (PD-L1),human epidermal growth factor receptor 2 (HER2),and nectin cell adhesion molecule 4 (Nectin 4).How to screen patients suitable for these treatments and monitor the therapy? Nuclear medicine with specific radiopharmaceuticals can visualize the expression level of those targets in systemic lesions and evaluate the efficacy of treatment.In addition to radiopharmaceuticals,imaging equipment is also a key step for nuclear medicine.Advanced equipment including total-body positron emission tomography/computed tomography (PET/CT) and positron emission tomography/magnetic resonance imaging (PET/MRI) has been developed,which contribute to the diagnosis and treatment of tumors,as well as the development of new radiopharmaceuticals.Here,we conclude most recently advances of radiopharmaceuticals in nuclear medicine,and they substantially increase the “arsenal” of clinicians for tumor therapy.
Keywords: Nuclear medicine;radiopharmaceuticals;neoplasms
Introduction
Nuclear medicine plays an irreplaceable role in the diagnosis and treatment of tumors.With the emergence of immunotherapy and targeted therapy,nuclear medicine plays a greater role in the diagnosis and treatment of tumors.Knowing the expression of biomarkers throughout the body is crucial for clinical treatment.However,conventional clinical methods such as immunohistochemistry (IHC) and fluorescencein situhybridization(FISH) to analyze the expression level of biomarkers in tumor tissues have poor reproducibility because they are unable to obtain the expression of biomarkers throughout the body.Meanwhile,they are invasive.Radiopharmaceuticals represented by18F-fluorodeoxyglucose (18FFDG),as the important components of nuclear medicine,have played a center role in many kinds of diseases,especially in tumors.However,18F-FDG reflects the glucose metabolism of the lesions and is not a tumorspecific imaging agent.Researchers have been committed to finding ideal targets and developing new radiopharmaceuticals (Figure 1). And radiopharmaceuticals targeting special tumor biomarkers have been gradually developed.Compared to18F-FDG,they are specific and can visualize the biomarker expression by imaging,which is helpful to diagnose specifically,detect lesions (including primary lesions and metastases)systemically,screen suitable patients for these treatments precisely,non-invasively as well.Many of them have been approved by the Food and Drug Administration (FDA) or have entered the clinical research stage.Radiopharmaceuticals targeting prostate-specific membrane antigen(PSMA) or somatostatin receptor (SSTR) have played an important role in the diagnosis and treatment of prostate cancer and neuroendocrine tumors.
In addition to radiopharmaceuticals,the nuclear medicine equipment also plays a positive role in the diagnosis and treatment of tumors.The novel nuclear medicine equipment includes total-body positron emission tomography/computed tomography (PET/CT) and positron emission tomography/magnetic resonance imaging (PET/MRI).Compared to conventional PET/CT,total-body PET/CT can reduce patient and staff doses (2),shorten acquisition time (3),optimize image quality,reduce radiopharmaceutical costs,and increase patient throughput(4).In addition,it can observe the distribution and metabolism of radiopharmaceuticals in the body in realtime and dynamically,which is very helpful for pharmacokinetic research.The soft tissue resolution of PET/MRI is better than conventional PET/CT,so it can better display the morphology of lesions and their relationship with adjacent tissues.
As easily can be found in the new advances,the rush hour of nuclear medicine is coming.
Concept of nuclear medicine and radiopharmaceuticals
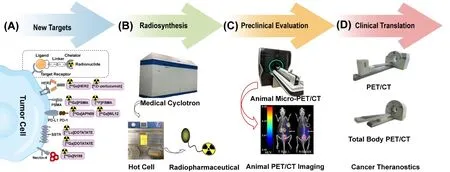
Figure 1 Radiopharmaceuticals: process from bench to bedside.(A) Radiopharmaceuticals are consisted of four parts including radionuclide,chelator,linker and ligand which could specially bind to cell surface receptors or targets such as PSMA,HER2,PD-1/PD-L1,SSTR and Nectin-4;(B) Preparation of radiopharmaceuticals includes production of nuclides,radiolabeling,and quality control.Animal PET/CT imaging demonstrated high accumulation in tumor region (1);(C) A series of preclinical evaluations are performed to screen out the optimal probes;(D) Optimal probe for clinical translation.Nuclear medicine equipment such as total-body PET/CT is applied to perform whole-body dynamic imaging with quite low doses to achieve visual diagnosis and treatment.PSMA,prostate-specific membrane antigen;HER2,human epidermal growth factor receptor 2;PD-1,programmed death 1;PD-L1,programmed death ligand 1;SSTR,somatostatin receptor;Nectin 4,nectin cell adhesion molecule 4;PET/CT,positron emission tomography/computed tomography.
In 1898,Pierre Curie and Marie Curie discovered the radioactive element radium (mainly226Ra) and polonium,pioneered the theory of radioactivity,and invented the radioisotope226Ra separation technique,which releases α rays that kill cells and bacteria.In 1905,Marie Curie performed the first radioisotope insertion therapy using a radium needle.Since then,humans began to study the application of radioactive elements in medical treatment.Nuclear medicine is a discipline using nuclear technology,mainly using radionuclides or nuclear radiation,to diagnose,treat and research diseases.It includes not only imaging diagnosis,functional determination,in vitroanalysis and nuclide therapy,but also various tracer experiments in the field of basic medical research.
Radiopharmaceuticals are a class of special drugs containing radionuclides for medical diagnosis and treatment.It can be simple radionuclide inorganic compounds,such as99mTcO4-,201TlCl,Na131I,etc,while most clinical radiopharmaceuticals are composed of radionuclides and non-radioactive labeled substances.Nonradioactive labeled parts include chemical compounds,biochemical agents (peptides,hormones,etc.),biological products (monoclonal antibodies,etc.),blood components(red blood cells,white blood cells) and antibiotics.
Generally,radiopharmaceuticals mainly consist of four parts: radionuclides,chelators,linkers,and ligands which can specifically bind to cell surface receptors or targets,such as PSMA,SSTR,human epidermal growth factor receptor 2 (HER2),programmed death 1 (PD-1)/programmed death ligand 1(PD-L1),and nectin cell adhesion molecule 4 (Nectin-4).The characteristics are as follows: 1) Radioactivity.Radiopharmaceuticals mainly use the particles or rays released by their radionuclides to achieve the purpose of diagnosis and treatment;2)Instability.Radionuclides in radiopharmaceuticals spontaneously decay into another nuclide or nuclear state,and not only does the amount of radioactivity but also their intrinsic mass change over time.Therefore,the concept of“recording time” should be emphasized during the whole process,from production,preparation,and quality control to clinical use;3) Radiation self-decomposition.The physical,chemical and biological effects of the particles or rays emitted by the decay of radionuclides directly affect the radiopharmaceutical itself,causing the change of the structure of the compound or the loss of biological activity,which can lead to the change of the biological behavior of the radiopharmaceuticalin vivo;and 4) Low dose.The dose of radiopharmaceuticals introduced into the body is mostly at the level of milligrams and micrograms,and thus usually using radioactive activity as a unit of measurement.
Functional imaging,molecular imaging and imaging probe
Functional imaging
Functional imaging is a way to demonstrate the functional changes of tissues and organs by imaging,primarily including MRI (diffusion imaging,perfusion imaging,brain functional localization imaging),CT (perfusion imaging),PET/CT (perfusion imaging,mainly used18F,11C,13N,15O and other labeled compounds for brain and myocardial blood perfusion imaging),single photon emission computed tomography (SPECT) (mainly includes regional cerebral blood flow and myocardial perfusion imaging).But it is insufficient for prediction of tumor markers.Thus,it remains unclear how to evaluate the efficacy of targeted therapies and optimize the therapeutic strategy.Therefore,novel imaging modality and biomarkers are being developed to better evaluate targeted therapy’s effects.
Molecular imaging
Molecular imaging is a non-invasive medical imaging method that enables visualization,characterization,and measurement of biological processes at the molecular and cellular levels in humans or other organisms.Compared to conventional imaging modalities,which mainly image the structural differences of tissues or organs,molecular imaging can demonstrate the physiological and biochemical activities of normal and diseased tissue cells in active state.The essence of molecular imaging is a technology based on functional imaging,which is used for diagnosis of diseaserelated molecular changes,drug development and treatment monitoring. Molecular imaging accelerates tumor detection,surgical guidance,targeted drug delivery,image-guided therapy,and efficacy evaluation.
Molecular imaging technologies mainly comprise nuclear medicine molecular imaging technology,magnetic resonance molecular imaging technology,optical imaging technology and ultrasonic imaging technology.However,because CT and MRI contrast agents are mostly nonspecific,and nuclear medicine imaging molecules are based on molecular tracers,they have unique advantages and convenient conditions in molecular imaging.PET imaging can visualize the expression of therapeutic targets of whole body with specific targeted molecular probes,such as various68Ga and18F-labeled PSMA ligands.The presence and degree of target protein expression were related to treatment response.Therefore,PET imaging probes have been introduced as predictive biomarkers (5).For example,measuring SSTR in patients with neuroendocrine tumors with68Ga-DOTATATE/TOC/NOC can predict peptide receptor radionuclide therapy response.PSMA-targeted PET imaging can not only help to differentiate the primary and metastatic prostate cancer,but also improve the detection rate of lymph nodes and bone metastases,especially at low prostate-specific antigen levels.
Nuclear medicine imaging probe
Tumor-specific imaging probes have been used to evaluate the efficacy of targeted cancer therapies.Tumor-specific imaging probes specifically bind carrier molecules labeled with positron emitters (for PET imaging),single photon emitters (for SPECT imaging),or fluorophores (for fluorescence imaging) to a specific tumor target.Carrier molecules can be monoclonal antibodies,monoclonal antibody fragments,adhesion molecules,small peptides,or small molecules that specifically target certain cell surface markers that are overexpressed in tumors.In addition,carrier molecules can also be small molecules that detect the acidic microenvironment of tumors.Therefore,the development and maturity of nuclear medicine imaging largely depend on the search for ideal targets and the design of ideal molecules as radiolabeled probes.In general,the ideal radiopharmaceuticals should have the following properties: high target-to-nontarget ratio after the drug enters the body,fast clearance in the blood,appropriate ray type,half-life and energy,suitable for SPECT and PET imaging,long retention time of the probes in the diseased tissue,convenient drug source,low price,and non-toxic.Moreover,in the synthesis of radiopharmaceuticals,the probes should be avoided to be destroyed and decomposed in the body (6).
Radiopharmaceuticals promote precise diagnosis and treatment of tumors
The discovery of various biomarkers has enabled the application of radiopharmaceuticals in clinical diagnosis and therapy to flourish.Encouraged by this,more and more radiopharmaceuticals have been approved by the FDA.With the popularity of SPECT and PET,the diagnostic research and development of radiopharmaceuticals represented by99mTc,18F and68Ga has developed rapidly in recent years,and has been developed for the diagnosis of various cancers,cardiovascular and cerebrovascular diseases,kidney function and nervous system diseases. Representative radiopharmaceuticals including68Ga-PSMA-11 and68Ga-DOTATATE are approved for the diagnosis of prostate cancers and neuroendocrine neoplasms (NENs),respectively.In recent years,with the great success of the FDA-approved177Lu-DOTATATE for the treatment of NENs and177Lu-PSMA-617 for the treatment of metastatic castrationresistant prostate cancer (mCRPC) in clinical applications,targeted radionuclide therapy has received extensive attention.In addition,radiopharmaceuticals targeting some therapeutic targets can visualize the expression level of corresponding targets in systemic lesions (including primary lesions and metastases) and can evaluate treatment efficacy.
In this section,we will describe the clinical translational research on PSMA,SSTR2,PD1/PD-L1 and HER2,which have been highly studied in recent years.In addition,we will also introduce the clinical translation of Nectin-4,a target that has been less studied in the field of nuclear medicine,in order to provide some thoughts on the research of new targets in the field of radiopharmaceuticals.
Radiopharmaceuticals targeting PSMA
PSMA is a type II transmembrane glycoprotein that exists on the cell surface.The expression level of PSMA is significantly upregulated in the membranes of almost all prostate cancer cells.68Ga-PSMA PET/CT can identify and locate tumors at the molecular level due to the specific binding of PSMA ligands,and detect tumors at early stages by imaging tiny lesions of 4 mm (7).FDA-approved radiopharmaceuticals targeting PSMA include68Ga-PSMA-11,18F-DCFPyL,and177Lu-PSMA-617 (Table 1).The VISION trial of the phase III study of177Lu-PSMA-617 in patients with mCRPC (8) facilitated the approval of177Lu-PSMA-617.PSMA PET is helpful for primary tumor staging,biochemical recurrence detection,restaging,efficacy evaluation,and treatment management (7).
PSMA-targeted imaging
Several studies indicated that PSMA PET imaging agents are diagnostically superior to other imaging examinations.Liuet al.(9) found that68Ga-PSMA-617 PET demonstrates a high detection rate of 75% (30/40) for primary prostate cancer,and even higher sensitivity and specificity.A meta-analysis (10) including 5 studies and 497 patients with prostate cancer showed that the sensitivityand specificity of PSMA PET/MRI to diagnose the primary lesion of prostate cancer were 91% and 64%,respectively,which is better than that of PSMA PET and MRI alone.

Table 1 FDA-approved radiopharmaceuticals targeting PSMA/SSTR for imaging/therapy
PSMA imaging is also valuable in pre-biopsy localization.PSMA PET scan before biopsy helps to avoid false negative pathological diagnoses when determining the puncture position,especially for small lesions (11).
The staging ability of PSMA PET/CT or PET/MRI is superior to the conventional imaging.The National Comprehensive Cancer Network (NCCN) guidelines(https://jnccn.org/view/journals/jnccn/21/10/articlep1067.xml) indicate that18F-pilufolastat PSMA or68Ga-PSMA-11 PET/CT or PET/MRI can be considered as an alternative to standard imaging of bone and soft tissues for initial staging,the detection of biochemically recurrent disease,and as workup for progression.A prospective,randomized and multi-center study (12) using PSMA PETCT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy found that the accuracy,sensitivity,and specificity of68Ga-PSMA-11 PET/CT in assessing pelvic lymph node metastasis were higher than those of the conventional imaging examinations.
PSMA PET shows great clinical application prospects in detecting lesions in biochemical recurrence (BCR) patients,and can still achieve high sensitivity even if prostatespecific antigen (PSA) is very low (<0.2 ng/mL).It is difficult for conventional imaging examinations to diagnose BCR.When PSA is less than 2.0 ng/mL,the sensitivity of the whole-body bone scan is low,with only 9.4%.The detection ability of CT for BCR is only 11%-14%,while PSMA PET/CT or PSMA PET/MRI has high diagnostic accuracy due to their high specificity (13).A meta-analysis(14) that included 16 studies and 1,309 BCR prostate cancer patients showed that the sensitivity and specificity of68Ga-PSMA PET imaging in diagnosing BCR prostate cancer metastasis were 80% and 97%,respectively.The sensitivity and specificity of pelvic lymph nodes and distant metastasis are both 86%,and it still expresses good diagnostic performance when the PSA level is low (<1.0 ng/mL).
With the continuous development of clinical research,scholars have discovered that some non-prostate tumors also take up68Ga/18F-PSMA,including liver cancer,lung cancer,renal cell carcinoma,thyroid cancer,breast cancer,central nervous system tumors,etc.The potential reason may be that PSMA is highly expressed in new blood vessels of these kind of tumors.Schmidtet al.(15) showed that detecting PSMA expression in lung cancer can be used to accurately screen beneficiaries of targeted PSMA therapy.In addition,a study (16) found that68Ga/18F-PSMA can detect lesions with no18F-FDG uptake,suggesting that68Ga/18F-PSMA PET/CT can be an effective supplement to18F-FDG PET/CT.However,it is worth noting that most studies on the application of68Ga/18F-PSMA PET/CT or PET/MRI in the diagnosis and treatment of non-prostate cancer tumors have small sample sizes or even only case reports,so large sample studies are needed to confirm it in the future.
PSMA-targeted radioligand therapy
The NCCN guidelines (https://jnccn.org/view/journals/jnccn/21/10/article-p1067.xml) indicate that177Lu-PSMA-617 is a treatment option for patients with ≥1 PSMApositive lesion and/or metastatic disease that is predominately PSMA-positive and with no dominant PSMA-negative metastatic lesions who have been treated previously with androgen receptor-directed therapy and a taxane-based chemotherapy. Some studies (17-23)demonstrated that177Lu-PSMA-617 has a positive effect on overall survival (OS),progression-free survival (PFS),PSA response and improvement of quality of life in mCRPC patients.
177Lu-PSMA-I&T is a great potentially promising radiopharmaceutical.A study (24) conducted in an East Asian population to evaluate the efficacy and safety of177Lu-PSMA-I&T in mCRPC patients found that radioligand therapy using177Lu-PSMA-I&T achieved good response in mCRPC patients,including 75% of patients achieved partial response (PR) or stable disease (SD),significantly improved quality of life,and were well tolerated.In addition,PSMA-I&T is easy to produce,which promotes its clinical application.
225Ac-targeted PSMA therapy is a new option for patients with advanced prostate cancer who are ineffective with other therapies,including177Lu-PSMA therapy.Some studies (25-27) have evaluated the efficacy of225Ac-PSMA-617 in mCRPC patients (including patients resistant to177Lu-PSMA-617),and preliminary results show its therapeutic potential.Among 26 mCRPC patients (who had received abiraterone or enzalutamide,docetaxel chemotherapy and177Lu-PSMA),65% of the patients had a decrease in PSA>50%,and the median OS was 7.7 months after receiving225Ac-PSMA-617 treatment (27).
PSMA-targeted radionuclide therapy with different radiopharmaceuticals has different biodistribution characteristics and toxicity.The combination of low-dose multiple radiopharmaceuticals can improve the efficacy.A study (28) suggested that a single course of tandem therapy with low-activity225Ac-PSMA-617/full-activity177Lu-PSMA-617 may safely enhance response to PSMA-targeted radioligand therapy in patients with late-stage/end-stage mCRPC,and it can minimize xerostomia severity.Another study (27) showed that 15 mCRPC patients received225Ac-PSMA-617 after progressing on177Lu-PSMA treatment,and 5 cases experienced a PSA decrease of >50%,but the overall treatment tolerance was poor.
Radiopharmaceuticals targeting SSTR
NENs are a type of heterogeneous malignancies that originate from the neuroendocrine system.In terms of pathology,according to the degree of differentiation,NENs is divided into well-differentiated neuroendocrine tumors (NETs) and poorly differentiated neuroendocrine carcinomas (NECs).Well-differentiated NENs can express high levels of SSTR.Somatostatin analogues (SSA) can specifically bind to SSTR.SSA drugs include SSTR agonists and SSTR antagonists.The radiopharmaceuticals targeting SSTR currently approved by the FDA include68Ga-DOTATATE,68Ga-DOTATOC,64Cu-DOTATATE,and177Lu-DOTATATE (Table 1).They are all SSTR agonists.
SSTR-targeted imaging
SSTR PET imaging is of great value in the diagnosis,staging,recurrence monitoring,guiding treatment,and monitoring prognosis of NENs (29). The NCCN guidelines (https://jnccn.org/view/journals/jnccn/19/7/article-p839.xml) recommend SSTR-PET/CT or SSTRPET/MRI as an imaging way for NENs.Haidaret al.(30)performed68Ga-DOTA-NOC PET/CT examination on 104 patients of NETs diagnosed by pathology and followup,and found that the diagnostic sensitivity,specificity,negative predictive value,and positive prediction value were greater or equal to 90.0%,and the accuracy was 0.931.68Ga-DOTA-SSTR PET/CT is superior to conventional imaging and SPECT imaging in initial tumor staging (31,32).In addition,SSTR PET imaging is also valuable in guiding treatment (33-35).Patients with positive68Ga-DOTA-SSTR PET/CT imaging may benefit from peptide radioreceptor therapy (PRRT) and SSTR analog treatment (35).
However,there are some disadvantages about radionuclide-labeled SSTR agonists.The tumor detection rates,especially the detection rate of liver metastases,are still limited (36).The clinical value of SSTR agonists is mainly limited by the following factors: 1) low detection sensitivity for small tumors;and 2) relatively high background activity in normal organs (especially liver,kidneys,and spleen).This limits the detection in small metastases with length less than 1 cm or poorly differentiated (G3 grade) NENs (37).In recent years,in vivoandin vitroresearch results have shown that NENs has higher uptake rate of SSTR antagonists than SSTR agonists,and the retention time of the former in tumor cells is longer than that of the latter (36,38-40).Therefore,the use of radionuclide-labeled SSTR antagonists emerges as a new approach to molecular imaging and treatment of NEN.SSTR antagonists currently successfully developed include68Ga-NODAGA-JR11,68Ga-DOTA-JR11,68Ga-NODAGA-LM3 and68Ga-DOTA-LM3.
In addition to NENs,SSTR imaging has also shown value in other tumors such as meningiomas (41-45) and multiple myeloma (46).A systematic review (47) found that68Ga-DOTA-SSTR PET studies may revolutionize the routine neuro-oncology practice,especially in meningiomas,by improving diagnostic accuracy,delineating radiotherapy targets,and evaluating patient eligibility for radionuclide therapies.
SSTR-targeted radioligand therapy
The NCCN guidelines (48) and the European Neuroendocrine Tumor Society (ENETS) consensus(49,50) recommend that PRRT is the first choice of treatment for patients with unresectable or metastatic NENs.In a NETTER-1 trial (51),the researchers found that the median OS with177Lu-DOATATE plus longacting octreotide is 11.7 months longer than with highdose long-acting octreotide alone in patients with midgut NETs. Despite final OS not reaching statistical significance,the results might be considered clinically relevant.The current clinical protocol for PRRT is to use177Lu or90Y-labeled SSTR agonists (such as90YDOTATOC and177Lu-DOTATATE),which can exert a tumor inhibitory effect,alleviate patients’ clinical symptoms,and prolong PFS (52). The combined application of90Y and177Lu nuclides can exert their complementary effects and improve the therapeutic effect on tumors of different sizes.NENs patients who used the combination of90Y-DOTATOC and177Lu-DOTATATE had a higher objective response rate,and the incidence of adverse reactions of both regimens was low (53).
PRRT with177Lu-DOTATATE is generally administered via intravenous injection for systemic radionuclide therapy (SRT).In SRT,a considerable amount of the radioactive dose is dissipated within the systemic circulation due to intravenous administration of radionuclides for therapy and therefore only part of the radiopharmaceuticals reaches the target sites.Some dosimetry studies (52,54) have also demonstrated the toxicity to bone marrows and kidneys from177Lu-DOTATATE SRT treatment due to systemic and offtarget exposure.Intra-arterial radionuclide therapy (IART)allows direct delivery of177Lu-DOTATATE to the tumor sites within the liver via intra-arterial cannulation of the hepatic artery.Some studies (55-57) about NENs demonstrated that IART led to higher tumor concentration and lower overall systemic toxicity (57) compared with SRT.In addition,in the treatment of meningiomas,some studies (58,59) have shown that IART can also increase the radioactive doses of tumor sites.As a result,IART seems to deliver high radioactive doses to tumor sites,therefore reducing overall systemic toxicity in comparison to SRT.However,large samples and prospective studies are still needed to verify that.
Radiopharmaceuticals targeting PD-1/PD-L1
In recent years,immune checkpoint inhibitor therapy has become an attractive research direction in tumor therapy.Among many new therapeutic targets,immune checkpoint inhibitors targeting PD-1 and PD-L1 have been widely used in clinical practice.However,not all tumor patients have good response to PD-1/PD-L1 targeted therapy because of the variable PD-1 or PD-L1 expression in tumors (60). Radiopharmaceutical imaging targeting PD-1/PD-L1 can screen potential beneficiaries in realtime,non-invasively,and dynamically during immunotherapy and can predict treatment effects,thereby guiding PD-1/PD-L1 targeted therapy and prognosis assessment.
Several radiopharmaceuticals targeting PD-1 or PD-L1 are currently investigated in clinical trials.The PD-1 imaging agents include89Zr-pembrolizumab,64Cupembrolizumab,and89Zr-nivolumab.A study (61)indicated that89Zr-nivolumab showed a significant tumor uptake rate in patients with PD-1-positive advanced nonsmall cell lung cancer.Tumor uptake of PD-L1 radiopharmaceuticals (89Zr-atezolizumab and68Ga-BMS-986192) is superior to predictive biomarkers based on immunohistochemistry or RNA sequencing in assessing clinical response to immune checkpoint inhibitor therapy(62,63).
In addition,some novel radiopharmaceuticals targeting PD-1/PD-L1 are also being studied.68Ga-NOTA-WL12 is a peptide-based PET imaging agent.The first-in-human findings (64) showed the safety and feasibility of68Ga-NOTA-WL12 for noninvasive,in vivodetection of PD-L1 expression levels in non-small cell lung cancer patients,which indicates the potential benefits for clinical PD-L1 therapy.Additionally,68Ga-THP-APN09 is a novel68Galabeled nanobody.A study (65) found that this tracer can detect PD-L1 expression levels in tumors,which may make it possible to predict response to PD-1 immunotherapy combined with chemotherapy.
Radiopharmaceuticals targeting HER2
HER2 is overexpressed mainly in breast cancer but also expressed in gastrointestinal,ovarian,and bladder cancer.Currently,various types of radionuclide-labeled probes including monoclonal antibodies and their fragments,nanobodies,affibodies and peptides are used in HER2 imaging.
Radiolabeled trastuzumab and pertuzumab can highly accumulate in HER2+tumor tissue,which is helpful for the detection and treatment of these tumors.In the first human study of89Zr-pertuzumab,Ulaneret al.(66) indicated that the imaging of the HER2 tracer is significant for assessing HER2 heterogeneity and for targeting patients with metastases unsuitable for biopsy,because they found 20% of patients with HER2-primary tumors will develop HER2+metastases finally.Tamuraet al.(67) used64Cu-DOTA-trastuzumab to image six HER2+breast cancer patients and they found that the radiation exposure of64Cu-DOTA-trastuzumab was 2.5 times lower than89Zrtrastuzumab.In addition,64Cu-DOTA-trastuzumab could be used to image other HER2+malignancies,such as advanced HER2+gastric cancer (67).
A novel affibody68Ga-NOTA-MAL-MZHER2 (68Ga-HER2) was developed by the team of the Department of Nuclear Medicine of Peking University Cancer Hospital and the team of Min Yang of the Jiangsu Institute of Atomic Medicine.They found that it is a feasible method to noninvasively detect the HER2 status in advanced gastric cancer patients and enable early detection with a low dose.Ongoing anti-HER2 therapy did not influence68Ga-HER2 affibody imaging,which allowed repeated evaluations to monitor the HER2 status after anti-HER2 therapy.This method provides anin vivounderstanding of advanced gastric cancer biology,and it can help oncologists improve individualized therapy plans (68).
Radiopharmaceuticals targeting Nectin-4
Nectin-4 has been reported to be overexpressed in 69% of tumor specimens,including breast cancer,lung cancer,pancreatic cancer,esophageal cancer,ovarian cancer,etc.For urothelial carcinoma,more than 80% of tumor specimens express Nectin-4,and 60% show moderate-tohigh staining (69).
Because the doses of antibody-drug conjugates (ADC)that can reach the targeted lesions are mainly related to the Nectin-4 expression level,it is necessary to monitor Nectin-4 expression before and during the ADC treatment (70).
Recently,the Peking University team developed a new radioactive PET tracer68Ga-N188 and conducted the first human study of PET/CT imaging.The tracer has fast blood clearance rate,high tumor cell target affinity and specificity,and can provide high-contrast PET images to quantitatively evaluate the Nectin-4 expression levels of tissue and tumors.68Ga-N188 PET imaging can be used to assess Nectin-4 expression in urothelial carcinoma,helping to select patients who are most likely to benefit from enfortumab vedotin therapy.The research results of this article provide strong support for the application of68Ga-N188 PET that can be used as an auxiliary diagnostic tool for optimizing treatments targeting Nectin-4 (70).
Triple-negative breast cancer is a subtype of breast cancer that does not express all of progesterone receptor,estrogen receptor and HER-2,and it is related to an unfavorable prognosis.A study (71) confirmed the high expression of Nectin-4 in triple-negative breast cancer by SPECT/CT and explored the feasibility of photothermal therapy with Nectin-4 as the target.
Nuclear medicine equipment advances diagnosis and treatment of tumor
In this section,we will introduce the novel nuclear medicine equipment,namely total-body PET/CT and PET/MRI.They have various advantages compared to conventional PET/CT and play a significant role in the diagnosis and treatment of tumors.
Total-body PET/CT
The uExplorer,a long axial field-of-view (LAFOV)PET/CT instrument,has been used in clinical,and it has an axial field of view of 1.94 m (2).This allows the entire adult human body to be scanned in a single-bed position.LAFOV PET/CT scanners offer greater flexibility to optimize image acquisition in terms of image quality,radiation exposure of the patients,and acquisition time(72).These changes can reduce patient and staff doses (2),shorten acquisition time (3),optimize image quality,reduce radiopharmaceutical costs,and increase patient throughput(4).The reduction in the doses of radiopharmaceuticals can reduce the radiation exposure of the patients,which is especially meaningful for children.The short acquisition time is meaningful for claustrophobic patients,severely ill patients,and children,and it avoids the risks associated with the use of sedative medications such as chloral hydrate.
Using two or more molecular probes for imaging is one of the ways to improve the diagnostic performance of PET/CT.Affected by the limitations of conventional PET/CT,it is difficult to implement dual tracer imaging in clinical work.Total-body PET/CT has high sensitivity,so dual-tracer imaging is feasible when using total-body PET/CT.Liuet al.(73) investigated the feasibility of a one-stop FDG-FAPI dual-tracer imaging protocol with dual-low activity for oncological imaging.They reported that the one-stop dual-tracer dual-low-activity PET imaging protocol combines the advantages of18F-FDG and68Ga-DOTA-FAPI-04 with shorter duration and lesser radiation and is thus clinically applicable (73).
Additionally,total-body PET/CT is helpful in the development of new radiopharmaceuticals.It can observe the distribution and metabolism of radiopharmaceuticals in the body in real-time and dynamically,which is helpful for pharmacokinetic research.In addition,the sensitivity of total-body PET is high,so it can be detected even if the low dose of radiopharmaceuticals,allowing research on lower drug doses to ensure safety.A study (74) used an ultra-low dose (0.37 MBq/kg) of18F-FDG to perform total-body dynamic imaging,and found the pharmacokinetic results were consistent with conventional doses(3.7 MBq/kg).In addition,using 1/10 of the dose,the radiation dose received by the patient was greatly reduced compared to the conventional dose group (median: 0.419vs.4.886 mSv;P<0.001) (74).What’s more,due to the high sensitivity of total-body PET/CT,it can detect signals generated by the decay of radionuclides with long halflives.Imaging can be possible over many half-lives without impairment in imaging quality (75).
PET/MRI
PET/MRI,as a new and promising multi-modal molecular imaging technology,began to be used in clinical since 2010.PET/MRI has great application in tumors,the cardiovascular system and the nervous system.This article mainly introduces its application in tumors.
PET/MRI can better display the morphology of lesions and their relationship with adjacent tissues,especially small lesions that cannot be displayed on PET/CT,owing to the good soft tissue resolution.In 2023,an international consensus recommendation for PET/MRI in oncology (76)summarized the application of PET/MR in many kinds of tumors.It demonstrates the significant value of PET/MRI in diagnosis,staging,restaging,biochemical recurrence,prediction and evaluation of therapy effect,prognosis,and evaluation of tumor aggressiveness.PET/MRI is superior to PET/CT in some aspects such as neuro-oncology and pleural invasion detection.
In addition,the combination of whole-body PET/CT imaging and local PET/MRI imaging can make up for the shortcomings of long PET/MRI examination time to a certain extent,and at the same time can give full play to the respective advantages of PET/CT and PET/MRI.
Conclusions
Nowadays nuclear medicine has shown significant value in the diagnosis and treatment of tumors,and radiopharmaceuticals are the cornerstone of the development of it.Both diagnostic and therapeutic radiopharmaceuticals are being developed.Therapeutic radiopharmaceuticals provide a new treatment method for tumor patients and have shown value in clinical practice.Radiopharmaceuticals targeting different targets promote precise diagnosis and treatment of tumors.New nuclear medicine equipment has also furtherly promoted the diagnosis and treatment of tumors and the research and development of new radiopharmaceuticals.It is believed that inspired by the novel radiopharmaceuticals,the rush hour of nuclear medicine is coming.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2023年5期
Chinese Journal of Cancer Research2023年5期
- Chinese Journal of Cancer Research的其它文章
- OpenNAU: An open-source platform for normalizing,analyzing,and visualizing cancer untargeted metabolomics data
- Genetic abnormalities assist in pathological diagnosis and EBVpositive cell density impact survival in Chinese angioimmunoblastic T-cell lymphoma patients
- Baseline radiologic features as predictors of efficacy in patients with pancreatic neuroendocrine tumors with liver metastases receiving surufatinib
- A novel multimodal prediction model based on DNA methylation biomarkers and low-dose computed tomography images for identifying early-stage lung cancer
- Genetic susceptibility loci of lung cancer are associated with malignant risk of pulmonary nodules and improve malignancy diagnosis based on CEA levels
- Update of latest data for combined therapy for esophageal cancer using radiotherapy and immunotherapy: A focus on efficacy,safety,and biomarkers
