Biochemical indicators and the Peradeniya Organophosphate Poisoning scale in prediction and prognosis of organophosphorus poisoning: An observational prospective study
Shivcharan Jelia,Banwari Lal,Divya Airan
Department of General Medicine,Government Medical College,Kota,India
ABSTRACT Objective:To study the value of some biochemical indicators and Peradeniya Organophosphate Poisoning scale in prediction and prognosis of organophosphorus poisoning.Methods:This was a hospital-based prospective,observational study.Various biochemical tests viz. complete blood count,random blood sugar,liver and renal function tests,creatine phosphokinase,and electrolytes were performed.Patients were assessed based on the Peradeniya Organophosphate Poisoning scale.All the patients were followed till the end point like recovery/death.Results:Out of the 100 patients,72% were males and 28% were females.The majority of the patients were farmers and 21 to 30 years of age.Suicidal was the most common manner (92,92%).Based on the Peradeniya Organophosphate Poisoning scale,47% were mild,34% moderate,and 19% severe.Serum creatinine,creatine phosphokinase,serum glutamic-oxaloacetic transaminase,serum glutamic pyruvic transaminase,and alkaline phosphatase levels showed a significant correlation with severity.Conclusions: Some biochemical indicators such as creatine phosphokinase,alkaline phosphatase can be used as prognostic markers of organophosphorus poisoning.The Peradeniya Organophosphate Poisoning scale can be used for assessing severity of the poisoning.
KEYWORDS: Organophosphate Poisoning scale;Creatine phosphokinase;Creatinine;Alkaline phosphatase;Liver enzymes;Organophosphorus poisoning
1.Introduction
Organophosphorus compounds are being used as pesticides for more than 60 years worldwide.Around 3 million people are exposed to organophosphate compounds.The documented fatalities are estimated around 3 lakhs every year[1].Potential causes of organophosphorus poisoning include intentional or accidental ingestion,inhalation,and skin exposure to agricultural pesticides[2].Clinical manifestations of organophosphorus poisoning depend on the route of exposure,poison load,chemical nature,and solubility characteristics of the compound.Symptoms are classified as acute (minutes to hours),delayed (days to weeks),and late (beyond 2 weeks)[3-5].
The acute symptoms and signs are due to muscarinic,nicotinic,and central receptor effects.Muscarinic symptoms include salivation,lacrimation,urination,defecation,emesis,and abdominal cramps.Salivation and bronchorrhea may cause aspiration pneumonitis in drowsy patients.Acute muscarinic effects on the heart (bradycardia,hypotension) can be life-threatening.Nicotinic effects of muscle weakness contribute to respiratory distress.Acute central effects such as restlessness,agitation,confusion,and sometimes convulsions may further compromise the airway and increase the risk of aspiration and hypoxia[3,4].
With adequate atropinization,the acute cholinergic symptoms diminish within a few hours,but some patients develop delayed effects[6].Usually,cholinergic symptoms typically occur within 24 hours of exposure,but late onset cholinergic symptoms and signs have been observed after 40 to 48 hours in dichlofenthion poisoning[7].The intermediate syndrome is characterized by paralysis of proximal limb muscles,neck flexors,motor cranial nerves,and respiratory muscles.This syndrome usually occurs 24 to 96 hours after poisoning.Once the cholinergic phase settles down,weakness may persist for up to 18 days[8].
Some patients manifest altered consciousness or coma days after the poisoning,particularly after a period of normal consciousness.This clinical entity is defined as delayed organophosphate encephalopathy or “central nervous system intermediate.” Coma with absent brainstem reflexes or encephalopathy has been reported after 4 days of normal consciousness and spontaneously resolved after another 4 days[9].Few patients have delayed extrapyramidal symptoms too.Dystonia,rest tremor,cogwheel rigidity,and choreoathetosis are a few extrapyramidal symptoms reported after organophosphorus poisoning[3].
Red blood cell cholinesterase levels are gold standard for organophosphorus poisoning but it is not widely available so serum pseudocholinesterase activity is assessed for estimating severity of organophosphorus poisoning[10].Various studies[11,12]have shown a significant correlation between creatine phosphokinase levels and severity of organophosphorus poisoning.Serum creatine kinase may be also used as a prognostic marker of organophosphorus poisoning.There is a reported incidence of rhabdomyolysis in intermediate syndrome which is followed by a proportionate rise in creatinine kinase level[13].A study by Senarathneet al.[14]suggested a significant correlation between liver enzymes level on admission and the severity of poisoning.Another study by Gaikwadet al.shows deranged liver function tests in organophosphorus poising[15].
This study is to assess the prognostic significance of hepatic enzymes,creatine phosphokinase,and Peradeniya Organophosphate Poisoning (POP) scale in patients with organophosphorus poisoning.
2.Patients and methods
2.1.Study design and setting
This is a prospective observational study.It was conducted in Department of General Medicine,Government Medical College,Kota,and the Group of associated hospitals,Kota from January 2020 to December 2022.
2.2.Inclusion and exclusion criteria
All the organophosphorus poisoning cases confirmed by history and characteristic clinical features were enrolled in the study.Patients with exposure to undefined compounds,mixed poisoning,pre-existing chronic liver,renal,cardiac diseases,myopathy,active malignancy,and autoimmune diseases were excluded from this study.
2.3.Ethical Approval
Ethical clearance was taken from the Institutional Ethical Committee of Medical College (Approval No.F.3/Acad/Ethical clearance/2021/44).All the patients were explained in detail about this study and written informed consent was obtained for each patient before their enrollment in the study.
2.4.Methodology
All the patients of organophosphorus poisoning were investigated for various biochemical parametersviz.complete blood count,random blood sugar,serum electrolytes,liver function tests,renal function tests,and creatine phosphokinase (CPK).For the abovementioned blood investigations,2 mL of blood was withdrawn by venepuncture from the patients within 12 hours of admission to the hospital.The venepuncture site was properly cleaned and blood withdrawn was collected in EDTA vial.The sample was transported immediately to a central laboratory where the sample was analyzed.Measurement of blood cells was done using an automatic blood counter (Beckman Coulter AcT5 Diff).Glucose estimation was carried out by the autoanalyzer.Creatine kinase was measured using NAC activated method.All patients were treated with atropine accordingly.Patients were assessed based on the POP scale.The POP scale are classified into mild (0-3),moderate (4-7),and severe (8-11).All the patients were followed till the end point like recovery/death.
2.5.Primary and secondary outcomes
The primary outcomes included the duration of hospital stay and the need for ventilatory support.The secondary outcome included mortality or recovery.
2.6.Statistical analysis
Excel 2017 and IBM SPSS Statistics version 26 were used.Categorical variables were expressed as numbers and percentages.Continuous variables were expressed as median (Q1,Q3) since they were abnormally distributed.They were analyzed by Chi-square test and non-parameter test.P<0.05 were considered significant.
3.Results
A total of 100 patients with organophosphorus poisoning were included (Figure 1).
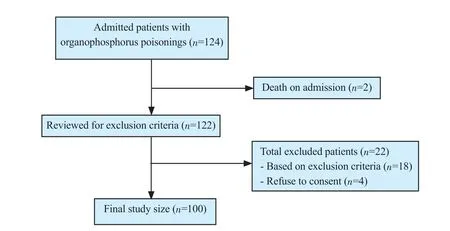
Figure 1.The study flow diagram.
3.1.Demographic and clinical characteristics
A total of 87% of patients were below 40 years of age.The majority of patients were males.A total of 69% of cases were from rural.Occupational history showed that the majority of patients (44%) were farmers followed by students (25%).A total of 92% of cases were due to suicidal intentions (Table 1).Nausea was the most common (95%) symptom followed by vomiting (88%).Most patients were in normal consciousness (Table 1).
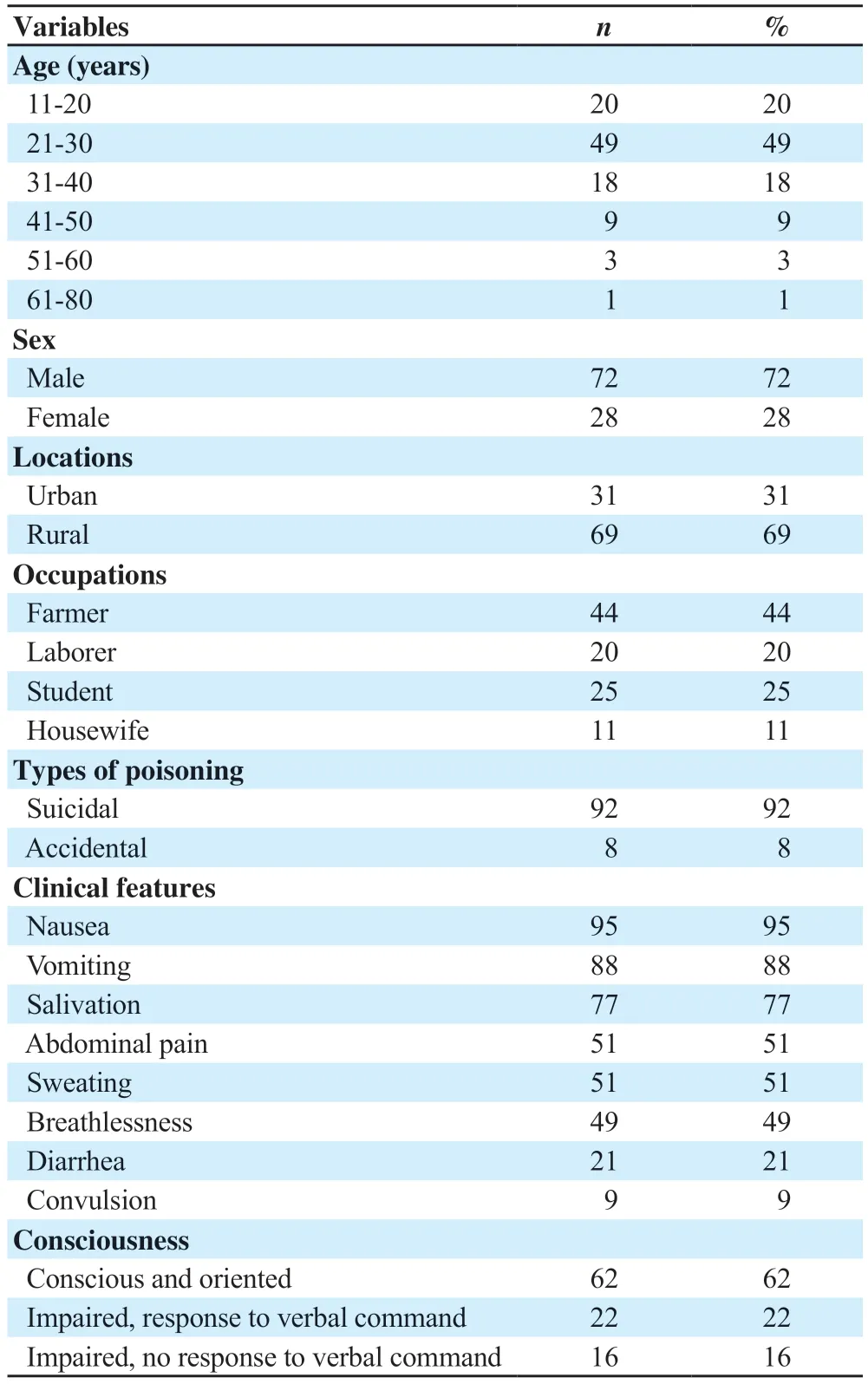
Table 1.Demographic and clinical characteristics (n=100).
3.2.Results of POP scale
Pinpoint pupil was observed among 54% of total patients while pupil size ≤2 mm was observed among 42% patients.Muscle fasciculation was present among 21% of patients.Around 49% patients had tachypnea.Out of the total patients,36% had bradycardia (Table 2).Based on the POP scale,47 patients were mild,34 were moderate,and 19 were in the severe category.
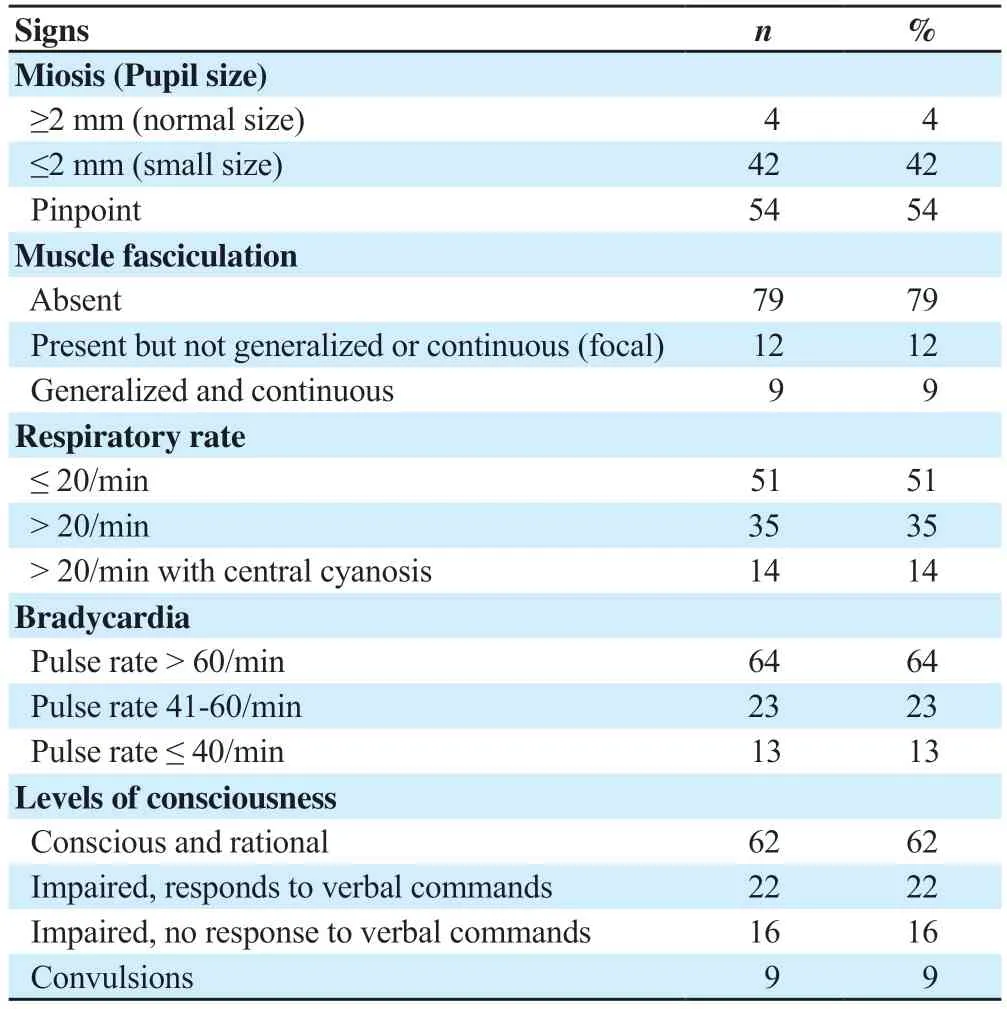
Table 2.Results of Peradeniya Organophosphate Poisoning scale (n=100).
3.3.Comparison of lab parameters between discharged and expired patients
There were significant differences in CPK and alkaline phosphatase between discharged patients and dead patients (P<0.001).And the differences in other parameters were not significant (Table 3).
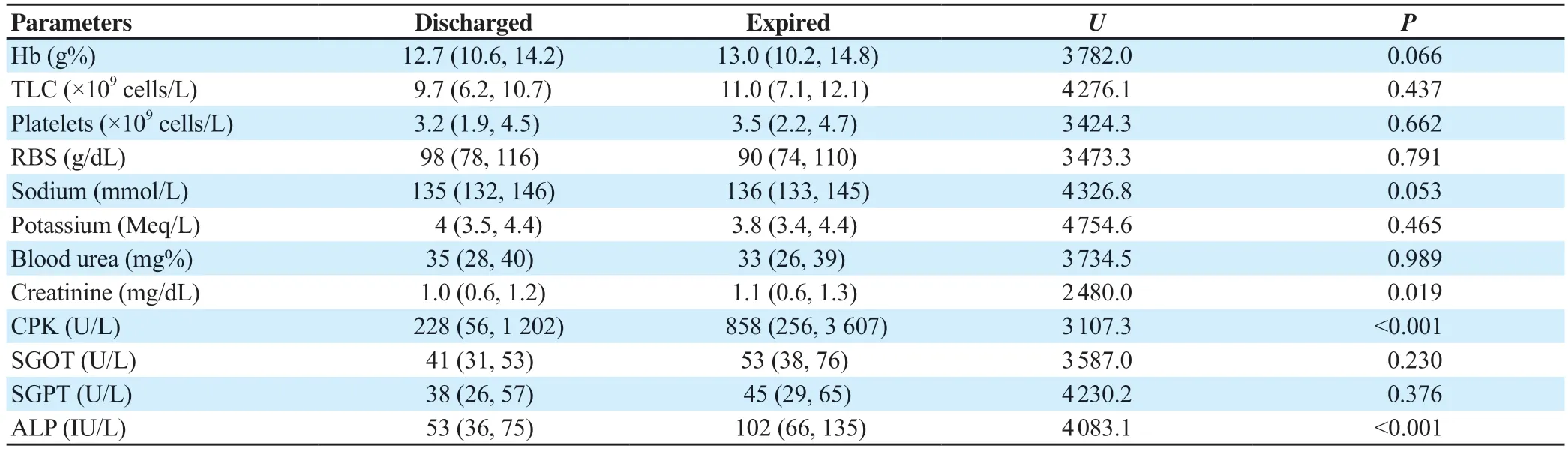
Table 3.Comparison of biochenmical parameters between discharged and expired patients (n=100,median,Q1,Q3).
3.4.Comparison of lab parameters among patients with different severities
Table 4 shows that patients with higher severity had higher levels of total leucocyte count,platelets,serum electrolytes,creatine kinase,CPK,serum glutamic-oxaloacetic transaminase (SGOT),serum glutamic pyruvic transaminase (SGPT),and alkaline phosphatase (P<0.05).
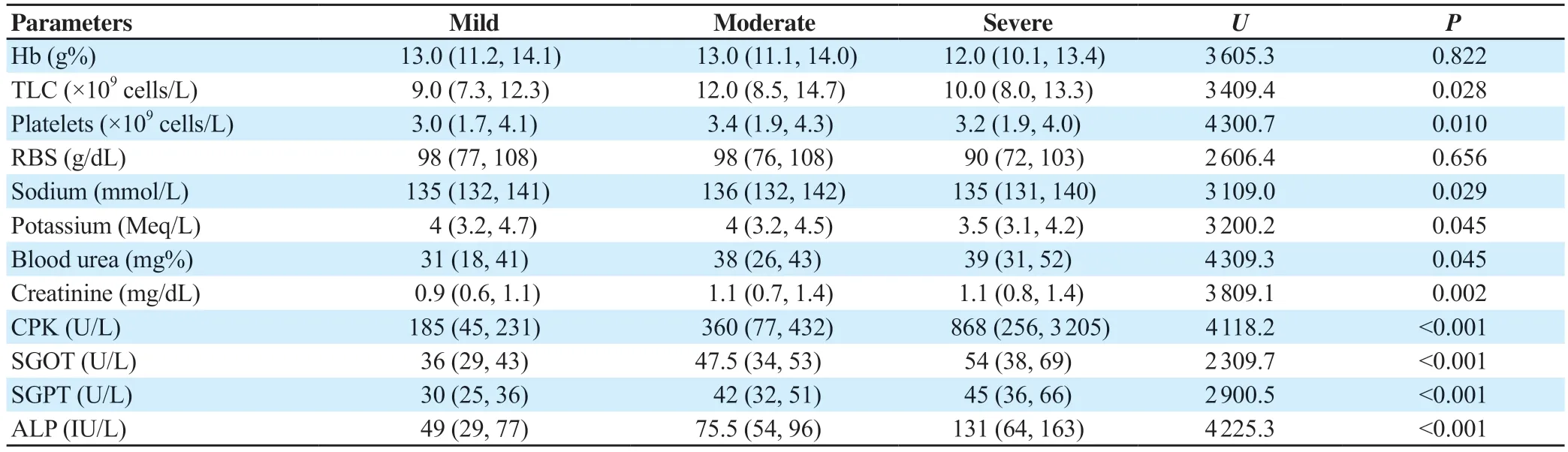
Table 4.Comparison of biochemical parameters among patients with different severities (n=100,median,Q1,Q3).
3.5.Outcome
A total of 26 patients had ventilator support and patients on a severe scale need more ventilator support (P<0.001) (Table 5).Duration of hospital stay of those on a severe scale [10 (8.1,13.2)]was longer,followed by the moderate category [7 (5.7,8.4)]and mild category [5 (4.4,5.7)].The difference was significant (P<0.001).
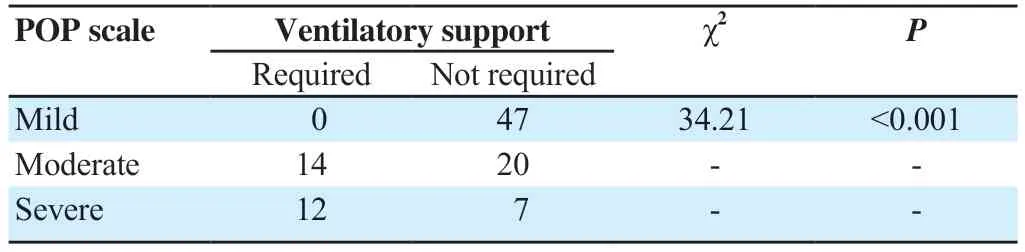
Table 5.Association between POP scale and ventilatory support (n=100).
A total of 91 patients were discharged after successful treatment and recovered while 9 patients were expired.A total of 36.84% of patients of the severe category expired (7/19) while only 5.88% of patients of the moderate category (2/34) expired and no patients from the mild category got expired.This difference was statistically significant (χ2=34.21,P<0.001).
4.Discussion
The present study showed that out of 100 patients,72% were males and 28% were females.It is similar to the study done by Dashet al.[16],which showed an incidence of 67% in males and 23% in females.It is also similar to the results demonstrated by Raveendraet al.[17]from Bengaluru,which showed that most of the patients were males (72%) compared to females (28%).Mundheet al.[18]also found 62.85% of males in their study.
In our study,87% of patients were below 40 years of age.Organophosphorus poisoning is common in the young generation as 67 patients were in the 20-40 age group,20 patients in the 11-20 age group,and only 13 patients were above 40 years of age in our study.Vernekaret al.[19]reported that 80% of the patients were younger than 30 years old.Less than 10% of cases were 40 years or above[19].Kamathet al.[20]showed that most patients were between 20 and 29 years (28%),followed by patients in the age group of 30-39 (21%)[20].A study by Mundheet al.[18]also found that most were young patients,81.42% of them being below 50 years.
Most patients came from rural areas.Regarding occupation,44% were farmers,25% were students,20% were laborers and 11% were housewives.Raveendraet al.[17]also showed that 72% of patients were involved in agriculture.Farmers are the leading group because of easy availability and accidental exposure during crop season in farms while a greater number of laborers in our study can be attributed to parallel COVID-19 pandemics leading to massive unemployment.Being a coaching hub of medical and engineering competitive exams,our city is responsible for a greater number of students opting for such drastic steps in despair.
The most common manner of poisoning was suicide (92%).Raveendraet al.[17]reported that all 100 patients consumed the poison with suicidal intentions.Mundheet al.[18]in their study found 70.27% of total patients had suicidal poisoning.
The present study illustrated that most of the patients manifested with nausea (95%),vomiting (88%),salivation (77%),abdominal pain (51%),sweating (51%),breathlessness (49%),diarrhea (21%) and least common being convulsions (9%).Mundheet al.[18]in their study found that vomiting was the most common symptom,present in 289 cases (89.47%) while convulsion was the least common symptom,present in 57 (17.65%) cases.Raveendraet al.[17]in their similar study found that the common presenting features were vomiting (96%),diarrhea (50%),lacrimation (50%),and altered sensorium (42%).
Of the 100 patients,47 (47%) were mild,34 (34%) moderate and 19 (19%) severe.In our study,none of the patients in the mild category required ventilatory support while 27.8% of patients in the moderate category and 66.7% of patients in the severe category required ventilatory support.Similarly,in a study done by Raveendraet al.[17],it was found that 3%,97%,and 100% of patients required ventilator support for mild,moderate,and severe grades,respectively.Kamath and Gautam[20]also reported that only 11.11% of the patients with mild poisoning needed ventilatory support,whereas 16.2% of patients with moderate poisoning and 100% of patients with a severe grade of poisoning required ventilator assistance.The incidence of respiratory failure increases with increasing severity.
In our study,the overall mortality was 9%.The mortality in the severe category is 36.8% followed by the moderate category (5.8%),and no death is seen in the mild category cases.Our results are very similar to the study done by Amiret al.[19],which showed significant mortality in the severe category (32%) while 4.5% and 0.09% in the moderate and mild categories respectively.In a study conducted by Peteret al.[21],the overall mortality was 13.1%.
The median duration of hospital stay was longer among the severe category and a higher percentage (66.7%) of patients with the severe category required ventilatory support during illness.
An increase in serum CPK levels reflects injury to the tissue of high CPK activity.CPK levels are useful in the diagnosis of acute medical conditions like myocardial infarction and skeletal muscle injuries.The present study showed that initial serum CPK levels had a high degree of correlation with the mortality and the severity of acute organophosphorus poisoning (P<0.001).These results are in agreement with the study conducted by Bhattacharyyaet al.[14].Muscle fiber necrosis and consequently raised CPK levels occur in severely acute organophosphorus poisoning cases.So,serum CPK is a cheaper,easily quantifiable,and more available biochemical marker for prediction and prognosis of patients with organophosphorus poisoning.
Meanwhile authors had linked the raised CPK levels to the rhabdomyolysis in intermediate syndrome.The excess acetylcholine seen in organophosphorus poisoning leads to reversible myocyte injury and the rise of different muscle enzymes,including CPK.However,the main disadvantage of serum CPK is its non-specificity.So,other conditions and diseases that may cause its elevation in patients with acute organophosphorus poisoning should be excluded.In our study,we observed that patients with higher scale scores had high values of SGOT,SGPT,and alkaline phosphatase.Risalet al.observed a significant correlation between SGOT and the severity of poisoning but they did not find any significant correlation between SGPT and bilirubin levels[22].In a study by Anormallikleriet al.[23],they found a statistically significant correlation between SGOT,SGPT levels,and the severity of organophosphorus poisoning.The liver metabolizes organophosphates through oxidation and sulfate or glucuronate conjugation and may undergo oxidative damage in case of organophosphorus poisoning.Hence,liver enzymes like SGOT and SGPT will be raised in severe organophosphorus poisoning cases.In our study,increase of SGOT and SGPT depends on the type of compound consumed.The main limitation of liver function tests is that underlying silent chronic liver disease cannot be ruled out for its non-specificity[22].
Further studies with a greater number of patients and in multicenters are required,since the present work was conducted on a relatively small number of patients,and in only one poisoning control unit.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Authors’contributions
SJ formulated the study concept and developed the study design.BL did a literature search and data collection.DA and BL did data and statistical analysis.Manuscript preparation was done by DA.All authors have reviewed and approved the final version of the manuscript.
 Journal of Acute Disease2023年4期
Journal of Acute Disease2023年4期
- Journal of Acute Disease的其它文章
- Heparin-binding protein combined with human serum albumin in early assessment of community-acquired pneumonia: A retrospective study
- Clinical profile of febrile encephalopathy patients at a tertiary care hospital in India: A retrospective study
- Effects of long COVID-19 among young adults in Turkey: A crosssectional study
- Epidemiology of animal bite injuries in North of Fars province in Iran
- Clinical and epidemiological features of pelvic fractures presenting to the emergency department in a tertiary health care hospital in south India: A retrospective study
- Central venous catheterization-related complications in a cohort of 100 hospitalized patients: An observational study
