Clinical features, radiological imaging, and treatment strategies of nonmetallic intraorbital foreign bodies: a retrospective analysis
Guang-Rui Chai, Ming Chen, Zi-Xun Song, Lu Liu
Department of Ophthalmology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province,China
Abstract● AlM: To provide comprehensive data on nonmetallic intraorbital foreign bodies (IOFBs) by summarizing and analyzing material types, clinical manifestations, imaging features, and treatment strategies.
● KEYWORDS: orbital trauma; nonmetallic intraorbital foreign body; clinical manifestations; computed tomography;magnetic resonance imaging
INTRODUCTION
An intraorbital foreign body (IOFB) refers to foreign bodies present in the orbit but outside of the eyeball,which is a type of open orbital trauma counting for 1/6 of all orbital trauma cases[1].IOFBs may cause serious damage to the structure and function of the eyeball or the contents of the orbit[2].The clinical features and complications vary with the material, size, shape, and location of the foreign bodies.
Regarding the material, foreign bodies can be divided into metallic (e.g., iron, aluminum, copper, lead), inorganic nonmetallic (e.g., glass, rock, sand, concrete), and organic nonmetallic (e.g., wood, thorns, bones, plastic, grease)materials[3].Among them, metallic foreign bodies are the most common, and a clinical diagnosis is relatively easy using computerized tomography (CT) examination.As a result,there are many published studies related to metallic foreign body cases.In contrast, nonmetallic foreign bodies have various components, complicated shapes, and diverse injury conditions, making clinical diagnosis extremely difficult.Thus, this type of IOFB is easily missed and/or misdiagnosed,which requires a comprehensive analysis of multiple imaging examinations.However, it is still challenging to completely remove IOFBsviasurgery, and the failure rate of the surgery is relatively high.To the best of our knowledge, few papers have been published regarding the treatment of nonmetallic IOFBs, although they are more prone to triggering severe complications[4-6].Only a handful of retrospective analyses with limited cases have been reported[7-10].Thus, it is necessary to conduct summaries of a series of nonmetallic IOFB cases to provide more information to improve the clinical diagnosis and treatment of IOFBs in the future.
This study aimed to provide comprehensive data on nonmetallic IOFBs by summarizing and analyzing material types, clinical manifestations, imaging features, and treatment strategies.The results from this study can be used as a reference to improve the treatment of nonmetallic IOFBs in the future.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Ethics Committee of the Shengjing Hospital of China Medical University (No.2020PS523K).All clinical procedures were performed in accordance with the Declaration of Helsinki.Informed consent was obtained from the subjects.
Patients and Data CollectionA retrospective analysis of the clinical data of patients with nonmetallic IOFBs was performed based on cases in the Department of Ophthalmology, Shengjing Hospital of China Medical University, from January 2012 to December 2020.There were 28 patients in total aged between 3 and 72y (Table 1).Trauma history, previous diagnosis and treatment, clinical manifestations, and CT and magnetic resonance imaging (MRI) findings of the patients were recorded.IOFBs were removed from all patients under general anesthesia.The subsequent condition of the patients following surgery was tracked for 6mo, and the imaging results were reviewed.Finally, we analyzed the epidemiological features,causes of injury, IOFB materials, clinical features, imaging manifestations, associated complications, and management outcomes of the cases and summarized the diagnosis and treatment methods.
RESULTS
Nonmetallic Intraorbital Foreign Body MaterialsAmong the nonmetallic foreign bodies, there were 19 cases of organic foreign bodies, including toothpick (1 case), straw (1 case),chopstick (3 cases), branch (6 cases), brush (2 cases), wooden stick (3 cases), plastic fragments (2 cases), and grease (1 case),as well as 9 cases of inorganic foreign bodies, including glass(4 cases), sand and stones (3 cases), and firecracker residue (2 cases), as shown in Table 2.
Entrance Route of Nonmetallic Intraorbital Foreign BodiesThe entrance routes of the nonmetallic foreign bodies are summarized in Table 2 and included the upper eyelid skin (7 cases), lower eyelid skin (4 cases), inner canthal skin (2 cases),outer canthal skin (1 case), lower fornix conjunctiva (6 cases),upper fornix conjunctiva (2 cases), inner canthal conjunctiva (4 cases), and outer canthal conjunctiva (2 cases).
Locations of Nonmetallic Intraorbital Foreign BodiesThe IOFB locations are summarized in Table 2 and included themedial side (11 cases), lateral side (2 cases), inferior side (5 cases), superior side (8 cases), and orbital apex (posterior side, 2 cases, Figure 1).In three cases, the IOFBs entered the maxillary sinus; in another two cases, the IOFBs entered the intracranial space.
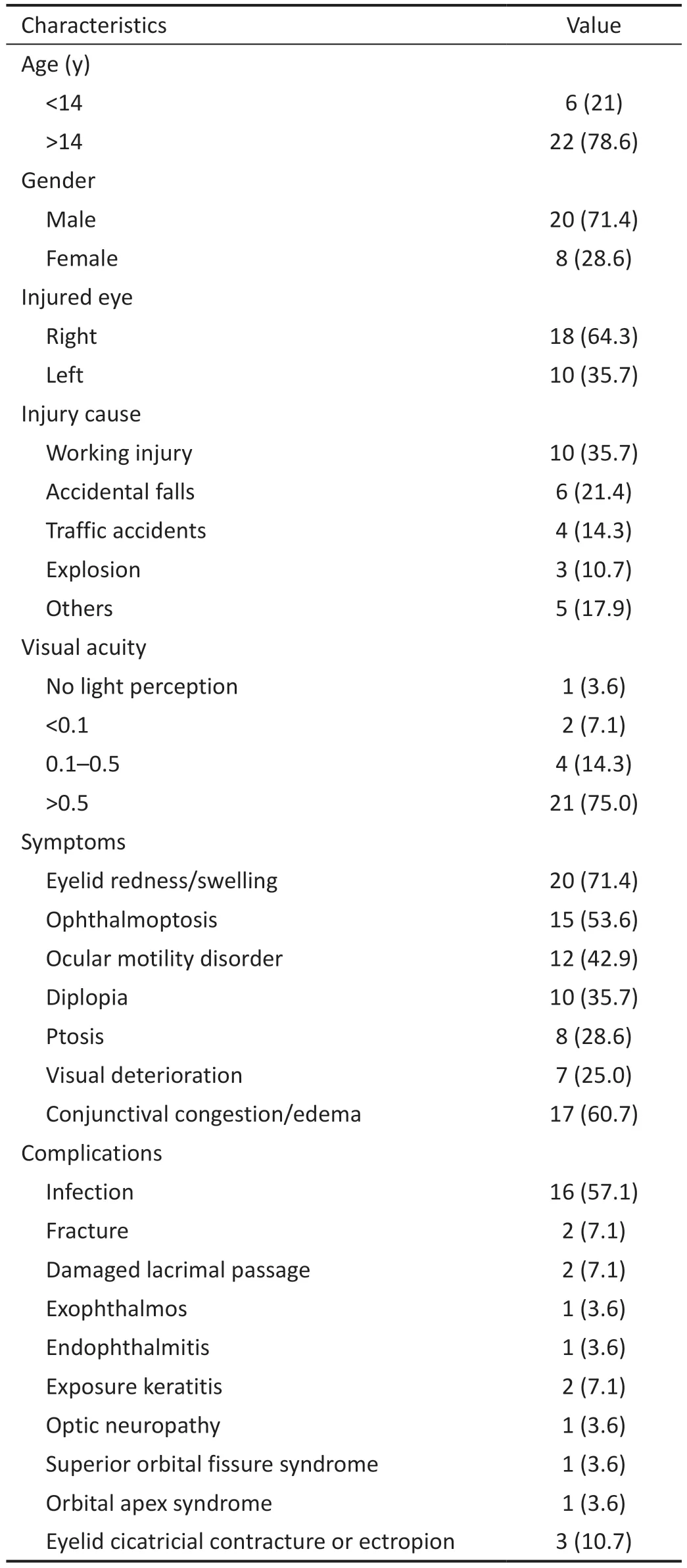
Table 1 Patient demographics n (%)

Figure 1 Schematic of locations of nonmetallic intraorbital foreign bodies in the orbit.
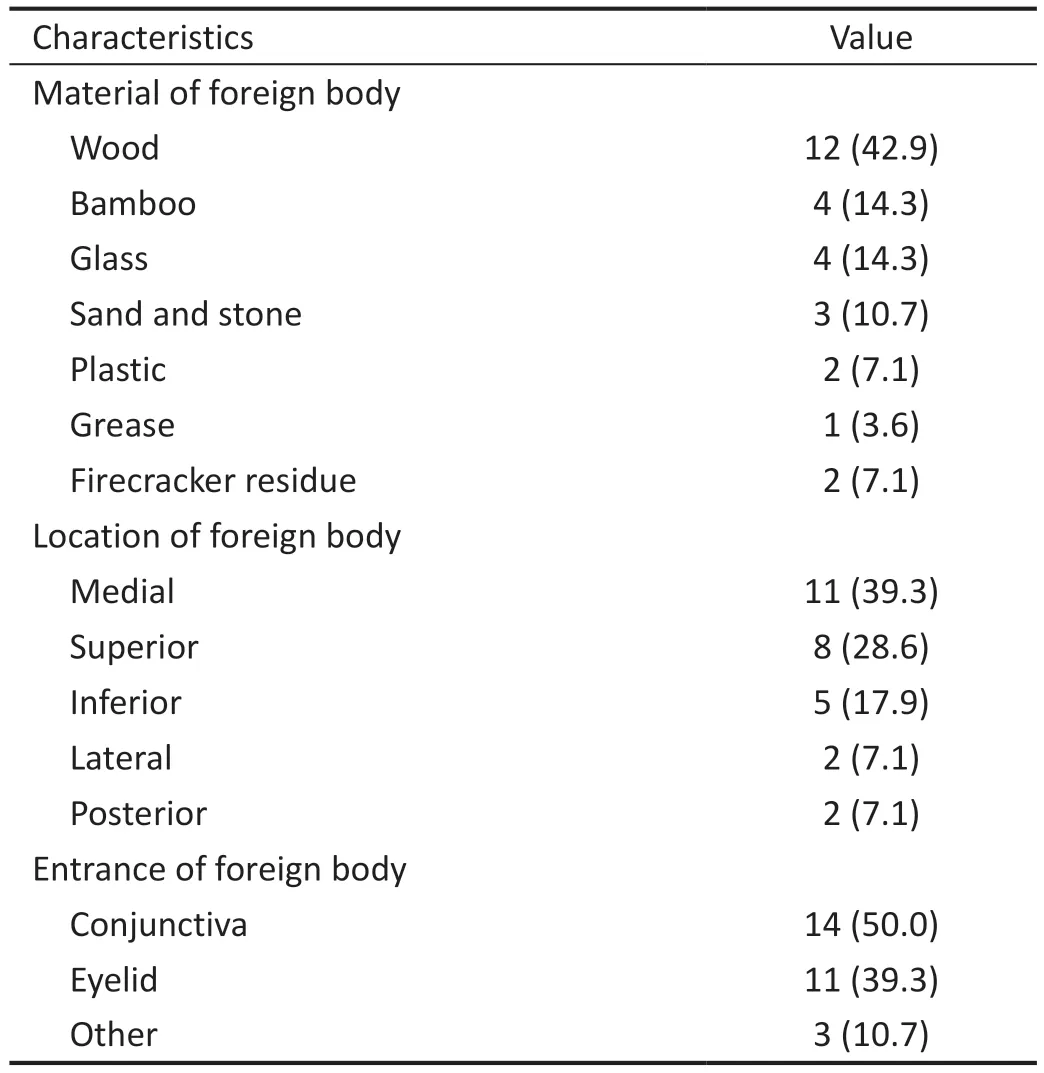
Table 2 Foreign body information n (%)
Clinical ManifestationsThe visual acuity testing results are summarized as follows: without light perception (1 case),light perception below 0.1 (2 cases), between 0.1 and 0.5 (4 cases), and above 0.5 (21 cases).Redness/swelling of the eyelids and pain were the most commonly observed clinical manifestations in most cases.Other clinical manifestations included exophthalmos (15 cases), eyeball displacement (6 cases), eyelid cicatricial contracture or ectropion (3 cases),ptosis (8 cases), ocular motility disorders (12 cases), periorbital protruding mass (3 cases), conjunctival hyperemia or edema(17 cases), and elevated orbital pressure (6 cases).For plantderived foreign bodies, the specific clinical manifestations included periorbital skin or conjunctival fistula, where pus was repeatedly discharged from the fistula.The main clinical manifestations are shown in Figure 2.The complications included intraorbital cellulitis (11 cases), eyeball contusion (4 cases), eyeball rupture (1 case), lacrimal duct rupture (2 cases),lacrimal sac injury (1 case), endophthalmitis (1 case), orbital fracture (2 cases), and exposure keratitis (2 cases), as shown in Table 1.
Computerized Tomography ImagingCT examinations were performed on all patients before surgery.Different CT values were achieved according to the different materialsof the foreign bodies (Table 3).Figure 3 illustrates some representative CT images of different foreign bodies, such as wood (A), grease (B), and glass (C), using the imaging system (Neusoft) in Shengjing Hospital.It was found that plant-derived foreign bodies, such as twigs (Figure 4A),toothpicks (Figure 4B), and chopsticks (Figure 4C), showed irregular or strip-shaped low-density shadows in the early stage of the injury, with the CT value falling in the range of-699 to -293 Hounsfield units (HU), while in the late stage,the density of the foreign bodies increased.For example, the CT values of five cases of plant-derived foreign bodies increased to 70-153 HU 2wk after the injury.When the window width and level were controlled at 350-500 HU and 30-40 HU, respectively, the foreign bodies presented as highdensity striped shadows surrounded by irregular soft tissue shadows with fuzzy boundaries.After adjusting the window width to 150-200 HU, the contrast between the foreign bodies and surrounding tissues was enhanced, presenting a clear boundary and showing the morphology of the foreign bodies.As toothpicks (Figure 4B) and chopsticks (Figure 4C)usually had less water content after processing, they showed a higher density of soft tissues in an orbit in a CT image, with CT values ranging from 42 to 147 HU and from 70 to 237 HU, respectively.Inorganic foreign bodies, such as gravel(Figure 4D) and glass (Figure 4E), presented as high-density block shadows with single or multiple pieces of various sizes that were distributed in a disseminated manner.Owing to the irregular shapes of these foreign bodies, their edges were sharp,with some angular protrusions.The CT value of the gravel foreign body was in the range of 557-745 HU, and that of the glass foreign body was 782-1922 HU.Firecracker residues appeared in the CT image as mottled soft tissue shadows mixed with high-density shadows, which had irregular shapes and were scattered and distributed.The grease foreign bodies appeared in the CT image as low-density shadows with smooth boundaries (Figure 4F), which usually had CT values ranging from -132 to -88 HU.
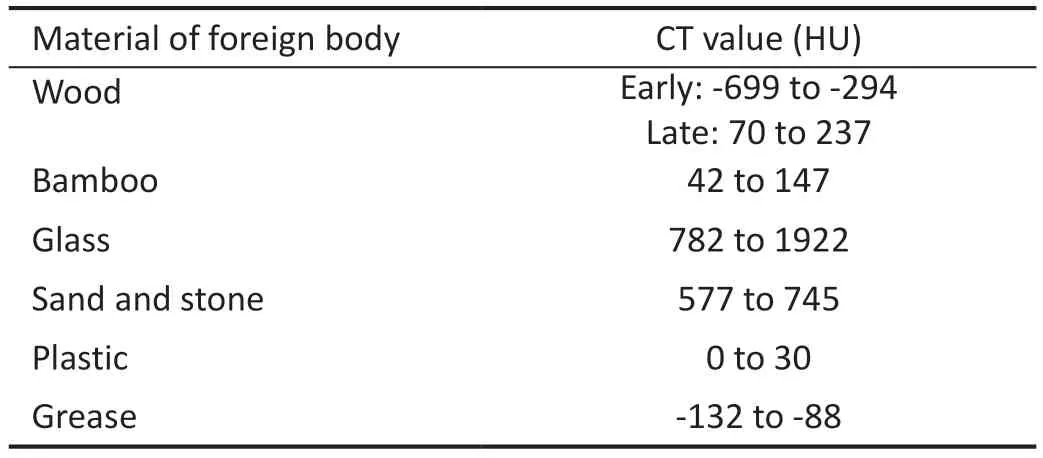
Table 3 CT values of foreign bodies
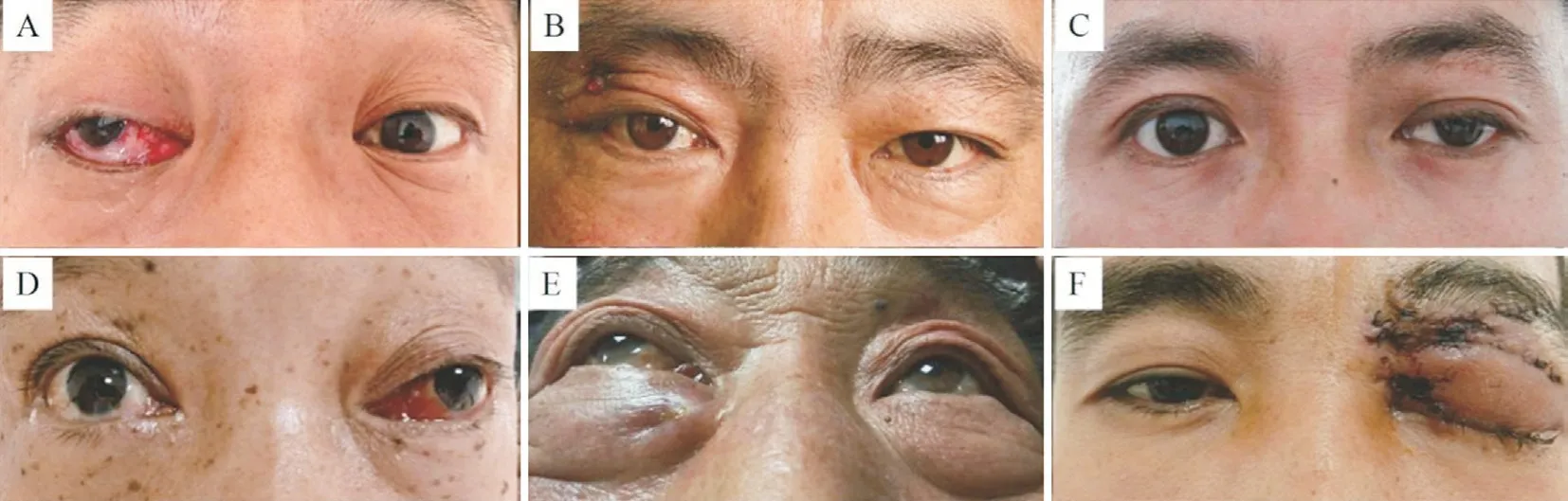
Figure 2 Clinical manifestations of intraorbital foreign bodies A: Conjunctiva hyperemia and edema; B: Periorbital skin fistula; C: Ptosis; D:Eyeball displacement; E: Exophthalmos; F: Eyelid cicatricial contracture.
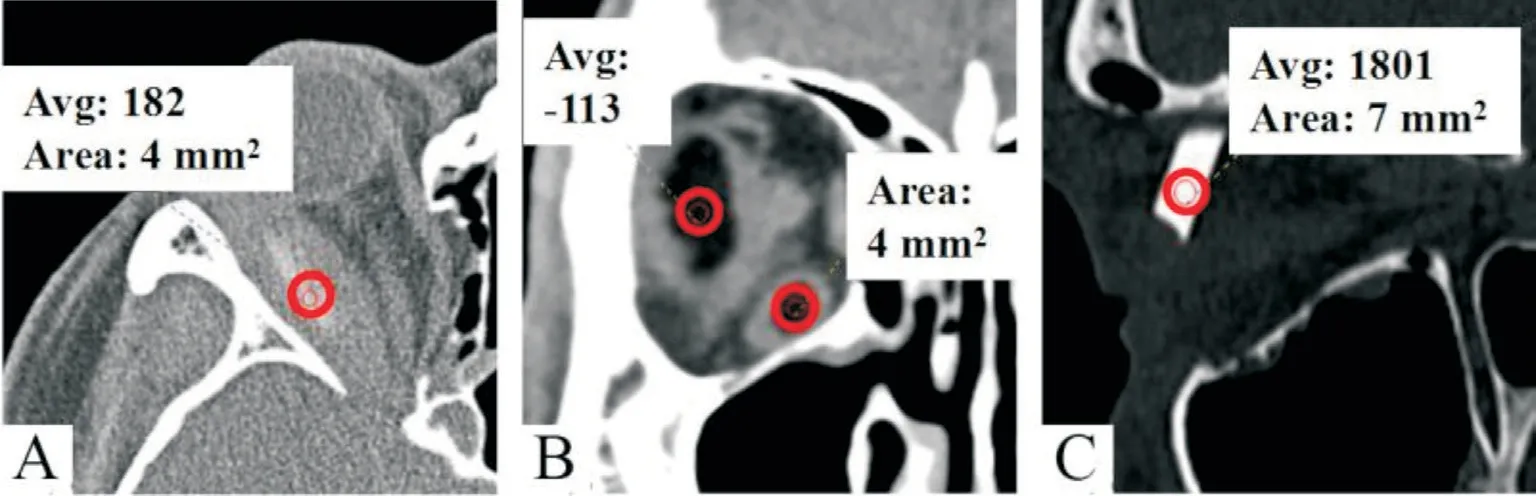
Figure 3 Computed tomography (CT) values of different foreign bodies CT values were measured by an imaging system (Neusoft).A: Wood; B:Grease; C: Glass.
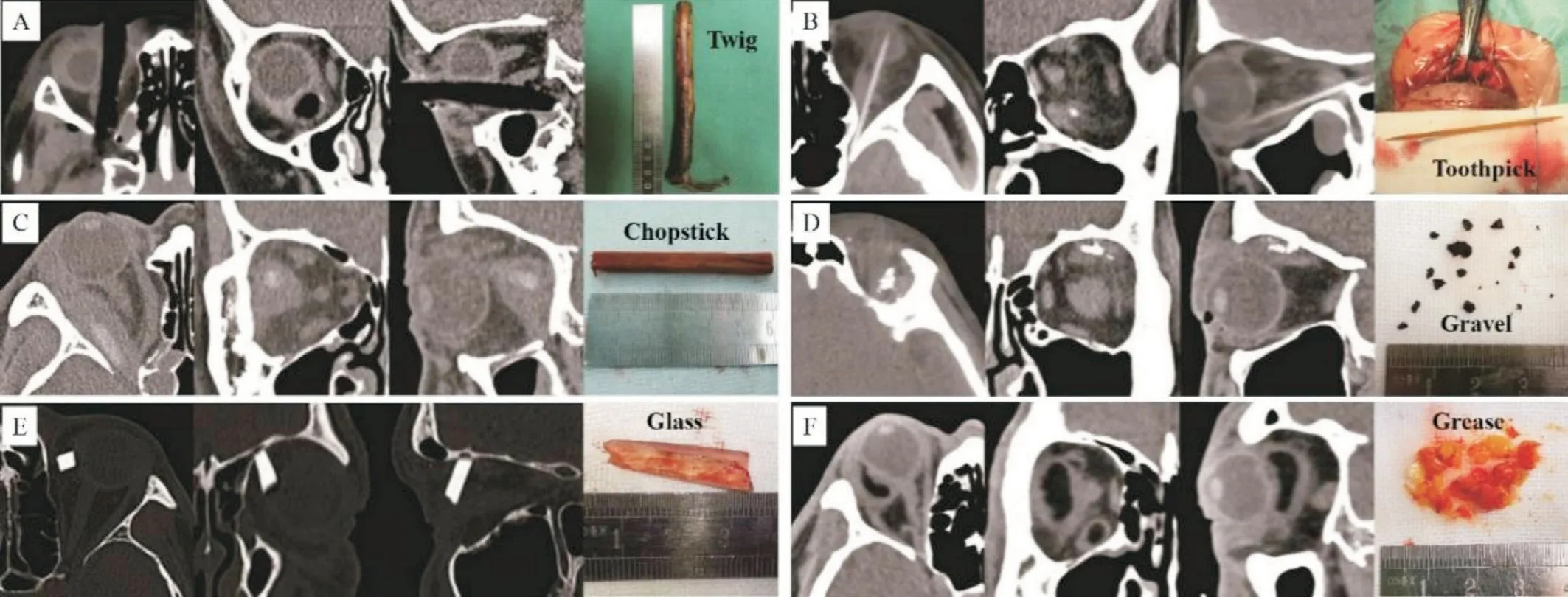
Figure 4 Computed tomography images of different foreign bodies A: Twig; B: Toothpick; C: Chopstick; D: Gravel; E: Glass; F: Grease.
Magnetic Resonance Imaging ExaminationTen cases of plant-derived foreign bodies and one case of a grease foreign body were examinedviaMRI.The plant-derived foreign bodies (Figures 5A-5C) showed low signals in both T1-weighted images (T1WI) and T2WI.The surrounding inflammatory tissues showed irregularly shaped mid-signal shadows, which were enhanced after further development.In addition, in five cases of plant-derived foreign bodies, pus cysts were observed around the foreign bodies, which showed circular high-intensity shadows in the T2WI.The grease foreign body illustrated a high signal in the T1WI and low signal in the T2WI (Figure 5D).
Surgical Treatment and Follow-upAll patients underwent removal of IOFBs under general anesthesia.Most patients underwent only one surgery to remove all foreign bodies and the surrounding inflammatory tissues; however, two patients underwent two surgeries.Postoperatively, each patient received intravenous broad-spectrum antibiotics (such as cephalosporin antibiotics) and oral anti-inflammatory agents for 7-10d.All patients were tracked and followed up for half a year after the surgery.Postoperatively, 15 patients experienced relief of herniated eyeball exophthalmos, and eye movement,ptosis, and visual acuity improved in four, two, and one cases,respectively.No surgery-related complications were observed in this study.The wounds of all patients healed well, and the fistula disappeared.An imaging review showed that all foreign bodies were completely removed.
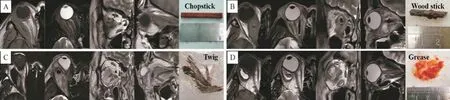
Figure 5 Magnetic resonance imaging of the foreign bodies A: Chopstick; B: Wood stick; C: Twig; D: Grease.
DISCUSSION
Nonmetallic IOFB injuries commonly occur during traffic accidents, accidental falls, bouncing injuries, or stab wounds during work or play.The high velocity and sharp shape of foreign bodies are the main reasons for these injuries.In this study, the nonmetallic foreign bodies included tree twigs/branches, chopsticks, bamboo toothpicks, wood sticks, glass,gravel, and plastic.In previous studies, more cases of children and young people were reported[11-12], while elderly patients only accounted for a small percentage.The reason may be that children easily fall when playing games and young people involved in carpentry work are at risk of injury by plantderived foreign bodies[13].In addition, inconvenience-induced falling is another reason for foreign bodies entering the patients' orbits.
Anatomically, the orbit has a pyramidal structure, with its apex located at the optic nerve foramen; the superior and inferior orbital fissures are two other paths to enter the skull directly in addition to the optic nerve.During an injury, a foreign body may pass through or stay in the space between the eyeball and orbital bone wall.To describe how a foreign body passes through the orbit, Turbinet al[14]counted 37 cases of transorbital foreign body trauma and divided the orbit into four areas.Based on a retrospective study of the orbital entrance area, they tried to predict the most likely path of the orbital foreign body.Shelstaet al[7]and Yoshiiet al[15]found that foreign bodies are mainly observed in the superior,medial, and inferior areas of the orbit and are uncommon in the posterior and lateral areas.This conclusion is consistent with the statistical results of this study.
The clinical manifestations caused by nonmetallic IOFBs vary based on the different materials of the foreign bodies.Common clinical manifestations include orbital cellulitis, orbital hematoma, proptosis, ptosis, ocular motility disorder, diplopia,orbital abscess, optic neuropathy/atrophy, superior orbital fissure syndrome, and orbital apex syndrome.The specific clinical manifestations are periorbital skin and/or conjunctival fistula, which are often caused by plant-derived organic foreign bodies.The porous structure of the plant surface provides a three-dimensional platform for bacterial growth[16],which leads to persistent and spreading inflammation.Thus,it is difficult to form an organic package to block purulent inflammation in cases of plant-derived foreign bodies and skin and/or conjunctiva rupture, and pus overflow frequently arises.Purulent inflammation and scar hyperplasia usually last for a long time, enabling the fistula to be closed temporarily.When the pressure rises owing to the accumulation of pus, the fistula can rupture again and release pus.Furthermore, the specific clinical manifestations are not related to the space-occupying effects of foreign bodies, mechanical damage, or rejection reactions[17].Scars and foreign body granulomas can exert the mechanical effects of space-occupying masses, which may manifest as exophthalmos and mechanical ptosis[18].However,clinical manifestations are often caused by a combination of multiple factors.For example, eye movement disorder can be attributed to mechanical damage to the extraocular muscles or oculomotor nerve and/or a large foreign body that hinders eye movement or contraction of the extraocular muscles.Scar adhesion can also lead to restrictive eye movement disorders.Therefore, the complete removal of foreign bodies is not the end of the story, but only the prerequisite of clinical treatments[17].Common complications of IOFBs include internal structural damage to the eyeball, orbital wall fracture,ptosis, eye movement disorder, lacrimal duct injury, and intracranial infection.Generally, a personalized multistage surgical repair plan is required.
For children or patients with an unclear medical history,more careful examinations and analyses are required by doctors.The clinical manifestations caused by IOFBs may last from a few weeks to months or even decades.Children often cannot describe their medical history clearly in detail,and some adult patients fail to recall the injury process and judge whether there is a foreign body.These conditions make diagnosis difficult and inaccurate, leading to a delay in further treatment[19].Besides, nonspecific symptoms of penetrating traumas, including vision changes, ophthalmoplegia, ptosis,tearing, drowsiness, fever, vomiting, and seizures, also bring the challenge to the timely and accurate diagnosis[20-21].As a result, rapid diagnosis and effective treatment of retained IOFBs are challenging for ophthalmologists.
Imaging examinations are of great significance for the diagnosis of IOFBs.Although the price of X-ray films is low,they can only detect substances that cannot be penetrated by X-rays.Thus, the high false-positive rate and low sensitivity make X-ray imaging unstable for IOFB detection.In contrast, ocular ultrasound has a higher sensitivity than X-ray and has been used for the inspection of foreign objects in closed eyeballs.For an open injury, probe squeezing during examination may aggravate the injury.In addition, ocular ultrasound cannot fully display the orbit, resulting in poor spatial orientation[22].Thus, it is not suitable for IOFB cases.
CT is considered the optimal imaging method for accurately detecting and locating metal-, stone-, and glass-based IOFBs[23].Therefore, CT is usually the first choice for orbital trauma and suspected foreign body penetration.Foreign bodies, such as metal, stones, and glass, are easily detected by CT scanning because of their high density.However, CT may occasionally fail to identify plant-derived foreign bodies, such as twigs and wood sticks; these foreign objects can be invisible in a CT image owing to their low density.Thus, both the quantity and shape of foreign bodies are difficult to measure.In addition, the CT image features of plant-derived foreign bodies may change over time, resulting in misdiagnosis or missed diagnosis[24-25].Successful detection of a plant-derived foreign bodyviaCT scanning is a complicated process coupling many factors, such as the size and material of the foreign body, as well as the degree of hydration.Generally, dry wood with low density is easily mistaken for ensnared air because of the similar density range during CT scanning.In contrast, fresh wood has a density similar to that of fat, making it difficult to differentiate in a CT image.Besides, the residues of wooden foreign bodies may have a density equivalent to or higher than that of fat after long-term retention in the wound because of the absorption of liquid and granulation[26].
MRI can only be applied to patients without metallic foreign bodies.It is considered a preferred choice for detecting organic foreign bodies.MRI shows low-intensity images of plantderived foreign bodies in open injuries.The shape and location of the low-density foci are very helpful in distinguishing the foreign body remaining in the image from other low-density signals.Unlike CT scanning, wooden foreign bodies usually have hypointensity comparable to intraorbital fat on both T1WI and T2WI that are not enhanced.In T1WI, a wooden foreign body gives a more uniform sign and is more perceivable when compared with T2WI.As a result, the chance of obtaining wooden relicsviaT1-WI is higher than thatviaT2-WI[27].Nevertheless, even if CT scanning and MRI are performed simultaneously in a patient, it is still feasible to have a missed diagnosis and/or detected foreign bodies[28].
Based on this retrospective study, CT scanning has the following advantages when used to inspect nonmetallic foreign bodies.First, CT scanning requires a relatively short acquisition time compared with other inspection methods,which saves time for first aid.Second, the measured CT values may aid in identifying the material of the foreign body; the densities of glass and stones are the highest, which are similar to that of bones; the density of plastic is second in the ranking,which is close to the density of soft tissues; grease and orbital fat have comparable densities; and the density of wood in the early stage (within 72h after injury) was the lowest, which is close to the density of air.Third, CT scanning can show the position and geometry of the foreign body in the orbit as well as its relationship with the surrounding tissues at a glance, which is very helpful for preoperative predictions.Fourth, the window width and window level of CT scanning can be flexibly adjusted to possibly maximize its validity in distinguishing foreign bodies.For example, in this work, a window width of 200 HU and window level of 40 HU were used to effectively detect the wood stick as an IOFB.Using these parameters, the contrast between the foreign body and surrounding tissues can be enhanced, making the boundary and morphology of the foreign body more clearly displayed.Thus, if a wooden foreign body is suspected, physicians should remind radiologists to better adjust the CT scanning parameters.In addition, for a suspected foreign body with a density less than water, the window width and level should be changed to ~1500 and ~500 HU, respectively, to distinguish it from air[29].Finally, CT scanning is the safest examination method when the material of the foreign body remains uncertain after trauma.
Treatment and prognosis depend on the structure and location of the foreign body as well as whether there is a secondary infection.Generally, a foreign body with a larger size is much easier to diagnose, detect, and remove before or during surgery.Conversely, smaller foreign bodies usually increase the possibility of missed diagnoses and/or difficult surgical manipulations.
Inorganic IOFBs, such as glass and gravel, are well tolerated in the orbit with a lower possibility of infection.Whether these IOFBs need to be removed must be decided based on their location and the associated complications.Because organic IOFBs, such as twigs and wood sticks, can cause inflammation and serious complications, they must be removed completely.Therefore, once an IOFB is diagnosed as plant-derived,surgery needs to be performed immediately to remove it[30].Plant-derived foreign bodies are more easily broken into pieces than metal- and glass-based foreign bodies, leading to residual or displaced secondary infections[31].Therefore, it is necessary to pay additional attention during surgical exploration to avoid leaving residues of plant-derived foreign bodies.After removal,iodophor, hydrogen peroxide, and antibiotics must be used to repeatedly flush the orbital cavity.A drainage strip can be placed during this process if necessary.In addition, secretions and pus need to be collected for further bacterial culture to select effective antibiotics based on the culturing results.Many pathogenic microorganisms can lead to infections, of whichStaphylococcusandStreptococcusare commonly seen[32-34].In the postoperative period, systemic broad-spectrum antibiotics are essential for preventing and controlling orbital infection[35].For plant-derived IOFBs, antifungal treatments are recommended because of the regular polymicrobial nature of related infections[36].
Regarding the choice of surgical access, a wound that is safe,small, and close to a foreign body is usually preferred.For open wounds and fistulas, it is better to select the original wound and fistula location to remove the foreign body and fistula simultaneously.When a wound is completely closed,it is recommended to choose the surgical approach according to the site and size of the injury and the intraorbital location of the foreign body, aiming to minimize secondary damage to surrounding tissues.It has been reported that a surgical navigation system can be applied to determine the incision position for old wounds with wound healing, scar hyperplasia,and fibrosis, which may contribute to avoiding iatrogenic injuries and repeated operation failures[37].Some foreign bodies also cause damage to the tissue constructs around the orbit.In this case, diagnosis and treatment require the collaboration of a multidisciplinary team consisting of ophthalmologists,otorhinolaryngologists, oral and maxillofacial surgeons,neurosurgeons, and radiologists[38-39].Therefore, for each suspected IOFB case, detailed ophthalmicand appropriate imaging examinations should be performed to assess the location, size, and material of the foreign bodies, and evaluate the potential damage caused by the surgery.In addition, it is necessary to fully understand the options and prognosis of patients.The opinions of the ophthalmologist and patient are equally important for making the final treatment decision[40].
In summary, the diagnosis and treatment of nonmetallic IOFBs are complicated processes with diverse conditions and multiple potential complications.Organic foreign bodies account for the majority of nonmetallic IOFBs.Clinical manifestations vary owing to the varied nature of the foreign bodies.CT images and values facilitate the identification of the foreign body material, although some wooden ones can sometimes be misdiagnosed or missed.MRI may help discover wooden foreign bodies and grease.Residual organic IOFBs can cause infections and inflammation, which should be completely removed.The surgical treatment of nonmetallic IOFBs is a complicated process, which may require a multidisciplinary team.
ACKNOWLEDGEMENTS
The authors thank all the patients who trusted them and all the doctors and staff who helped them in this study.
Authors’contributions:Chai GR conceived and designed the study.Song ZX and Liu L performed the sample collection and data analysis.Chai GR wrote the manuscript.Chen M revised the manuscript and provided recommendations.All authors have read and approved the final manuscript.
Conflicts of Interest: Chai GR,None;Chen M,None;Song ZX,None;Liu L,None.
 International Journal of Ophthalmology2023年7期
International Journal of Ophthalmology2023年7期
- International Journal of Ophthalmology的其它文章
- Chickenpox followed streaky multifocal choroiditis with prednison treatment in a girl with asthma
- Pneumonia and ocular disease as the primary presentations of Takayasu arteritis: a case report
- Unilateral blurred vision in pediatric patient associated with cavum velum interpositum cyst
- Highly cited publication performance in the ophthalmology category in the Web of Science database:a bibliometric analysis
- Comparison of efficacy of conbercept, aflibercept, and ranibizumab ophthalmic injection in the treatment of macular edema caused by retinal vein occlusion: a Metaanalysis
- Ocular manifestations and quality of life in patients after hematopoietic stem cell transplantation
