Long-term observation on safety and visual quality of implantable collamer lens V4c implantation for myopia correction: a 5-year follow-up
Xiao Chen, Li Li, Jing Rao, Yue-Xi Chen, Yang Gao, Rui-Xue Huang, Qi-Zhi Zhou,3
1Aier Eye Hospital, Jinan University, Guangzhou 510071,Guangdong Province, China
2Chongqing Aier and Vision Care Hospital, Chongqing 400000, China
3Aier Eye Hospital Group Company Limited, Changsha 410000, Hunan Province, China
4Jinan University, Guangzhou 510000, Guangdong Province,China
Abstract● AlM: To elucidate the safety and visual quality of implantable collamer lens with central hole (ICL V4c) implantation for correcting moderate and high myopia for at least 5y.
● KEYWORDS: implantable collamer lens with central hole; myopia correction; refractive surgery; visual quality
INTRODUCTION
Implantable collamer lens (ICL; STAAR Surgical, Nidau,Switzerland) is a posterior chamber phakic intraocular lens implanted to correct myopia, hyperopia, and astigmatism.In recent years, the prevalence of myopia has obviously increased and the ICL implantation has been rapidly developed to correct myopia.In April 2019, STAAR Surgical announced the sales of 1 million ICL lenses, and in June 2022, approximately three years later, STAAR Surgical celebrates the cumulative sales of 2 million ICLs[1].Especially, with the appearance of the central hole of ICL V4c, complications such as lens opacification,postoperative high intraocular pressure (IOP),etc.have been reduced, and might be more tolerant to low vault[2-3].And in the past, only a few studies reported the long-term (5-8y followedup) effectiveness and safety of ICL V4c implantation and the safety index (SI) is 1.03 to 1.12 and efficacy index (EI) is 0.79 to 0.90[4-7].While the comprehensive evaluation of long-term visual quality, ICL hole location after the lens implantation was insufficient.
Therefore, this retrospective study aimed to elucidate the safety, objective and subjective visual quality, central hole position and other indicators for five years or more after ICL V4c implantation, and the study outcome might provide comprehensive information for the long-term use of ICL V4c.
SUBJECTS AND METHODS
Ethical ApprovalThe study adhered to the Declaration of Helsinki principles and was approved by the Ethics Committee of Chongqing Aier Eye Hospital (approval No.IRB 2019006Z6).All patients provided the signed informed consent.
SubjectsA retrospective analysis was performed on patients who received ICL V4c implantation at Chongqing Aier Eye Hospital, Chongqing, China between January 2015 and December 2016.Inclusion criteria were as follows: 1) age between 18 and 45y; 2) preoperative spherical equivalent (SE)ranged from -3.0 to -18.0 D; 3) in the refractive state for about 2y with the diopter change of less than 0.5 D/y; 4) followed-up postoperatively for ≥5y.Exclusion criteria were as follows: 1)patients who were pregnant or lactating during the follow-up period; 2) a history of ocular surgery before lens implantation or ophthalmopathy; 3) unable to follow up on time and cooperate with the examination.Notably, the implantation and examination conformed with the ICL surgical indication and relevant national guidelines.
Preoperative and Postoperative ExaminationsBefore the lens implantation, and 1d, 1wk, 1mo, 1 and 5y after the surgery, uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), spherical equivalent (SE),IOP, pupil diameter, axial length, and corneal endothelial cell density were recorded.At the last follow-up, we measured the vault, central hole position and visual quality.The central distance between ICL and natural crystals is the vault[6], which was measured using OCT (HD-OCT 5000, Carl Zeiss, Meditec Inc., Germany).We measured the vault by skilled technicians under natural light without dilated pupils.The central hole of the ICL lens was assessed using the image analysis system of slit lamp photography by drawing a circle with the pupil as the center and dividing the upper nasal, lower nasal, upper temporal, and lower temporal quadrants with horizontal and vertical lines.Moreover, the central hole was located at the center of the pupil, the nasal horizontal line was situated in the middle, and the temporal horizontal line was positioned in the middle.OPD Scan III analyzer (NIDEK Inc., San Jose,CA, USA) measured the aberration in the central 4 mm area in the dark room.Optical quality analysis system II (OQAS,Visiometrics, Terrassa, Spain) was utilized to measure the modulation transfer function cutoff frequency (MTF cutoff),objective scattering index (OSI), and Stroller's ratio (SR) in the 4 mm pupillary area.OQAS was used under low illumination conditions in a darkroom, where the patient's pupil center was aligned with the instrument's optical axis during measurement and remained consistent throughout the measurement process.OPD Scan III is an aberrometer with Placido based on a shack Hartmann.The study of aberration using OPD Scan III has been applied in previous studies and has clinical significance,including studies in the 4 mm area[8-9], with the help of Fourier transform, OQAS is designed according to the asymmetric pattern of the double-pass technology[10].It is currently the only instrument that can be used to objectively measure the optimal aberration and the impact of human eye transparency loss.It provides optical quality parameters, such as MTF, SR,and OSI[10].In our study, retinal image quality measurements were evaluated using a 4.0 mm pupil.This standard size is usually used for analyzing ocular aberrations, which is closer to measuring visual acuity using undilated pupils[11].
The Visual Quality Scoring Table used in the studies by Mangione[12]and Hayset al[13]was adopted to develop a questionnaire consisting of 12 items, such as daytime distance vision, daytime near vision, close reading, watching the computer screen, day driving, night driving, night vision,night halo, night glare, visual fatigue, overall satisfaction with the surgical procedure, and willingness to choose surgical option again, with each item scoring 1-5 points.The 1 point was denoted as very dissatisfied and 5 points denoted as very satisfied, that is, the higher the score, the higher the satisfaction.All examinations and questionnaires were completed by the same examiner.
Statistical AnalysisSPSS version 23.0 (IBM Corp.,Armonk, NY, USA) was employed for statistical analysis.The Kolmogorov-Smirnov test was used to analyze normal distribution.Pairedt-test or repeated measurement ANOVA was used to compare preoperative and postoperative indicators with normal distribution, and the Chi-square test was used for inconsistent data.AP-value of <0.05 was considered statistically significant.
RESULTS
Patient Demographic CharacteristicsA total of 58 patients(114 eyes) were recruited for this retrospective study, with an average follow-up period of 69.25±3.80mo (ranged from 60 to 82mo), including 73 eyes (64.0%) with ICL implantation and 41 eyes (36.0%) with toric implantable collamer lens (TICL)implantation.The lens sizes were 12.1 mm in 10 eyes (8.8%),12.6 mm in 63 eyes (55.3%), 13.2 mm in 39 eyes (34.2%), and 13.7 mm in 2 eyes (1.8%).The preoperative mean age was 25.67±7.29y.The mean preoperative SE was -8.66±1.97 D(Table 1).
Visual Acuity and RefractionAt the preoperative and the last visit CDVA (logMAR) were 0.04±0.10 and 0.00±0.04,respectively (t=-4.281,P<0.001).At 5y postoperatively, 110 eyes (96%) and 68 eyes (59.6%) of UDVA were better than 20/40 and 20/20 respectively.Compared with the preoperative CDVA, 74 eyes (65%) of the postoperative UDVA did not change or gained more than one line.Compared with the preoperative CDVA, the postoperative CDVA did not change or gained more than one line in 89% of eyes, of which 7% of eyes gained two or more lines (Figure 1).SE was-8.66±1.97 D and -0.65±0.63 D, respectively before and 5y after the implantation (t=-43.252,P<0.001).Postoperative SE at ±0.50 D and ±1.00 D accounted for 55.3% and 76.3%,respectively.
Safety and Effectiveness IndicesAt the last visit, the SI(postoperative CDVA/preoperative CDVA) was 1.01±0.02; the EI (postoperative UDVA/preoperative CDVA) was 0.99±0.42.
Intraocular Pressure, Vault, Axial Length, and Endothelial Cell DensityThe IOP was 13.99±2.58, 13.12±2.82,12.69±2.31, and 14.89±2.50 mm Hg before the implantation,and 1d, 1mo, and 5y after implantation (F=29.013,P<0.001),respectively.The IOPs in all cases were <25 mm Hg.The mean vault at the last follow-up was 510.59±245.61 μm.The proportion of eyes with low vault (<100 μm), 100-1000 μm,and high vault (>1000 μm) were 1.8%, 95.6%, and 0.9%,respectively, in which the eyes with vault >750 μm accounted for 19.3% (22/114).The mean axial length was 26.71±1.09 mm and 26.83±1.20 mm before and 5y after the implantation,respectively (t=-3.843,P<0.001).The mean axial length increased by 0.29±0.71 mm at the last follow-up.The rate of endothelial loss was 1.55%±7.65%.
Central Hole PositionAmong 95 eyes, the central hole was located in the supratemporal area in 31 eyes (32.7%), the infratemporal area in 35 eyes (36.8%), the middle temporal area in 14 eyes (14.7%), the supranasal area in 8 eyes (8.4%),the median in 5 eyes (5.3%), and the subnasal area in 2 eyes(2.1%; Figure 2).
Visual QualityAt 5y postoperatively, the OSI was 1.5±1.2;the SR was 0.17±0.06; the MTF cut-off was 29.84±11.19 cycles per degree (cpd).The total spherical aberration, coma,trefoil, and total higher-order aberrations were 0.05±0.10,0.09±0.11, 0.21±0.13, and 0.28±0.28 μm, respectively.According to the visual quality questionnaire, 90.9% of patients were willing to choose ICL implantation again,3 (5.5%) people were not certain about choosing the ICL implantation again, and 1 (1.8%) patient moderately disagreed to choose the surgery again; 98.2% of patients were satisfied with the surgical procedure; 98.1% of the patients said that their distant vision in the daytime was better than that before the surgical implantation; 83.6% of the patients said that they had visual fatigue normally.Based on the visual quality questionnaire at 5y after surgery, the highest score was for patients willing to choose the surgery again, and the lowest score was for asthenopia (Table 2).
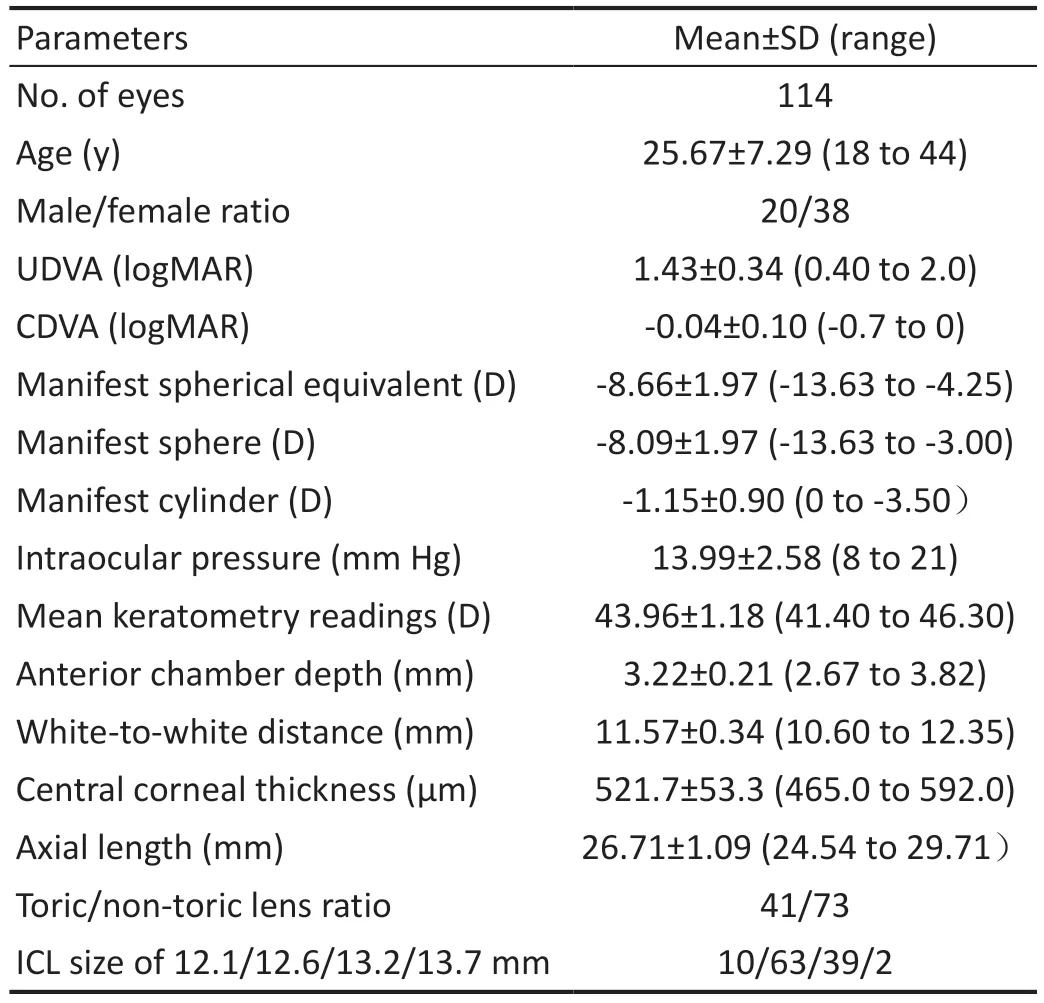
Table 1 Demographic characteristics of patients
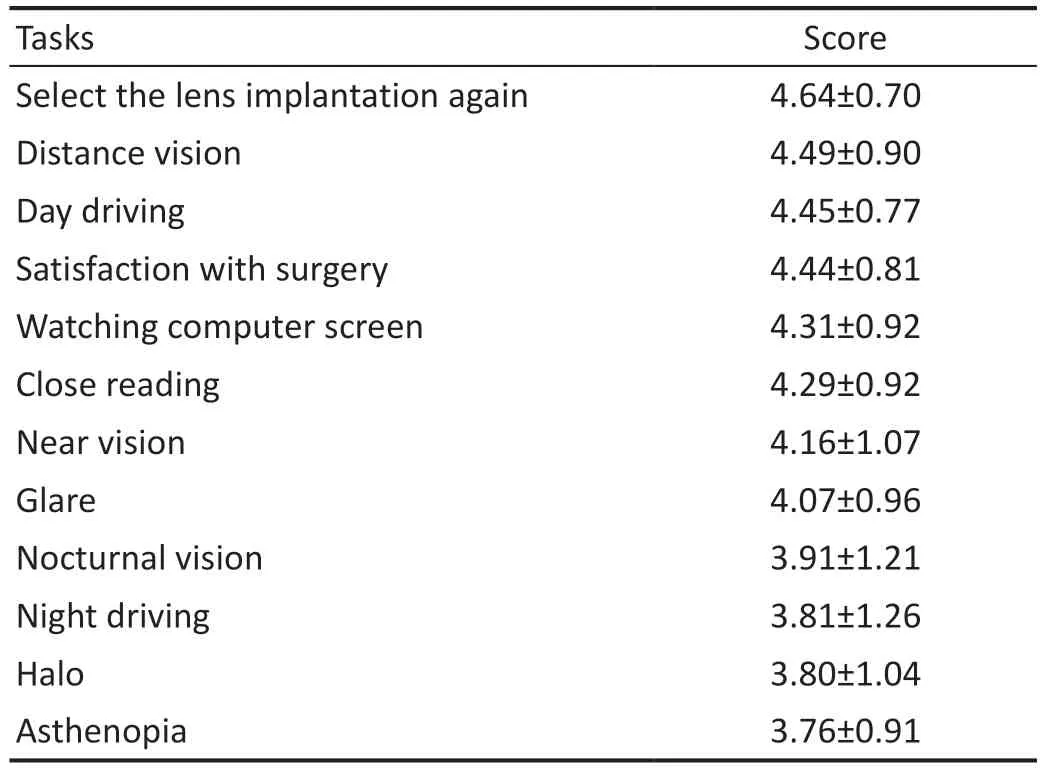
Table 2 The score of visual quality questionnaire
Adverse EventsAdverse events occurred in 4 eyes (3.5%)in 3 patients at 5y after surgical implantation.Following a trauma incident, one patient had TICL rotation in the right eye and it was adjusted, and the spontaneous TICL rotation of the opposite eye was also adjusted.The second patient (0.9%) had iris incarceration in left eye (0.9%), and relieved by surgical intervention.The third patient suffered from ICL movement in left eye following trauma.All these cases were operated twice,and the postoperative CDVA was greater than or equal to the preoperative CDVA (Table 3).
DISCUSSION
This retrospective study revealed that ICL implantation was safe and effective for five years or more.The safety and effectiveness indices were 1.01 and 0.99, respectively.The ICL placement in the eye was considerably stable.Furthermore,patient satisfaction regarding the surgical procedure and benefit was high.Based on the results of the visual quality questionnaire, 98.2% patients were satisfied with the surgical implantation, and 90.9% patients were willing to choose the ICL implantation again.
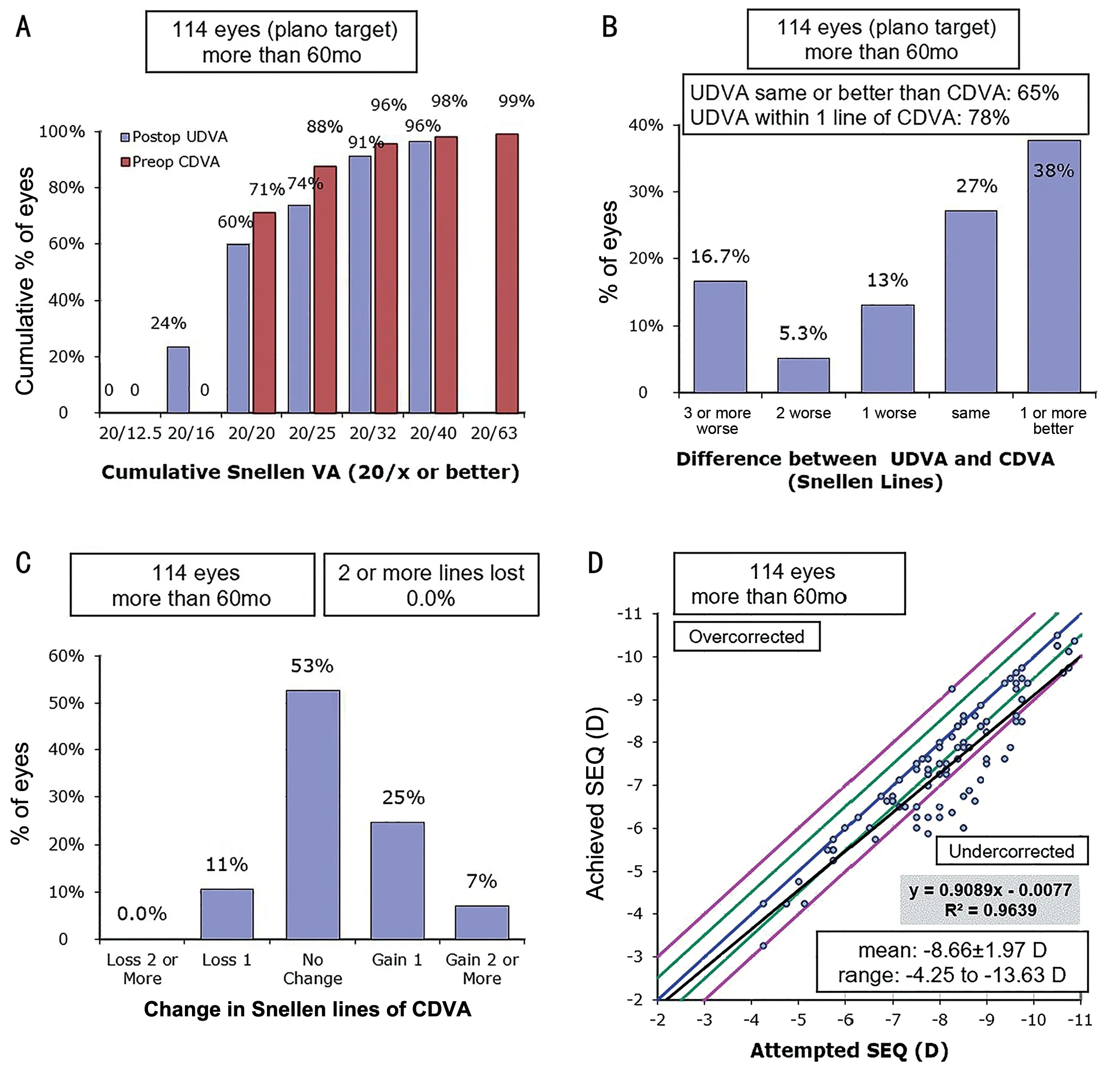
Figure 1 Visual acuity and refraction UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; VA: Visual acuity; SEQ:Spherical equivalent refraction.
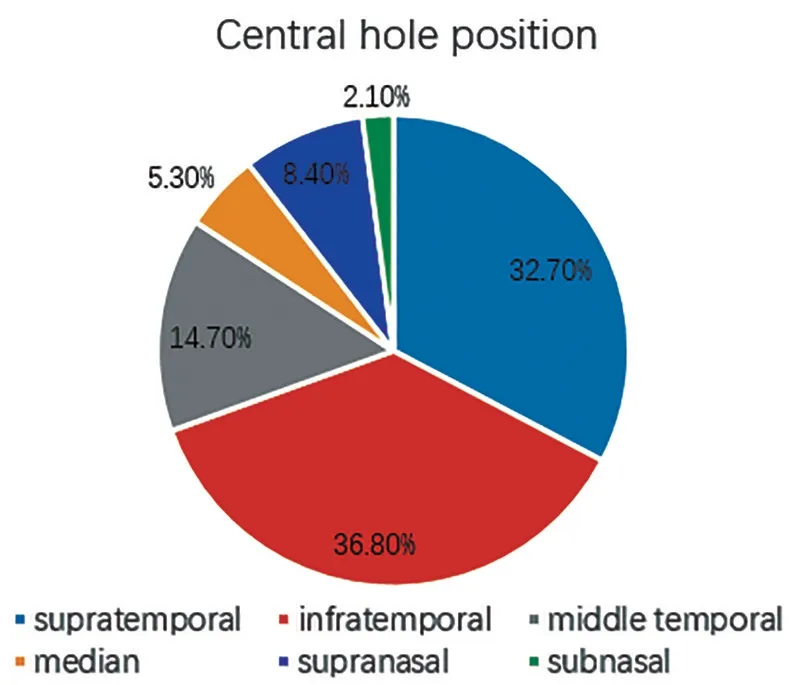
Figure 2 Location of central hole 5y after lens implantation.
In some previous studies, the SI was 1.03 to 1.12 and EI was 0.79 to 0.90 three to ten years after ICL V4c surgical implantation[4,6-7,14-15].In our study, the SI was slightly lower,and EI was slightly higher than previous reports.The variation may have been related to our preoperative comprehensive optometry taking 20/20 as the best stop point for correcting the distance vision.However, the safety index was above 1.0.The percentage of eyes with UDVA 20/40 or better was 95.35%,and the percentage of eyes with UDVA 20/20 or better at 5y was 46.51%, which was close to the outcomes of Chenet al's study[5].In our study, UDVA of ≥20/40 was present in 96% of eyes, and UDVA of ≥20/20 was seen in 59.6% of eyes.
The 5-year outcomes from the study by Alfonsoet al[4]on ICL V4c showed that the proportion of SE within ±0.50 D and ±1.00 D was 64.7% and 90.1%, respectively, which was slightly lower than our results.Additionally, in Papa-Vettorazziet al's[15]10-year follow-up study, the proportion of SE at±0.50 D was 42%, and the proportion of SE at ±1.00 D was 64%, which was lower than our results.In general, the longterm predictability of ICL implantable was high.
Chenet al[5]elucidated the high myopia (HM) group and superhigh myopia (SHM) group of patients five years after ICL surgical implantation and found that the axial length increased by 0.16 and 0.39 mm, respectively following ICL implantation.In our study, the axial length increased by 0.29 mm after surgical implantation at last follow-up.The preoperative SE in our study was -8.66 D, which was lower than -8.94 D in the HM group in the study by Chenet al[5].However, due to the use of different equipment in measuring the axial length,variations may have arisen in the axial length.We used A-mode ultrasound and Chenet al's[5]study utilized the IOL Master.In a previous study[16], the axial length measured by A-scan was higher than that measured by the IOL master.In our study, the increase in axial length after ICL, accompanied by the rise of axial myopia, was an important factor affecting the long-term stability and predictability of ICL implants.
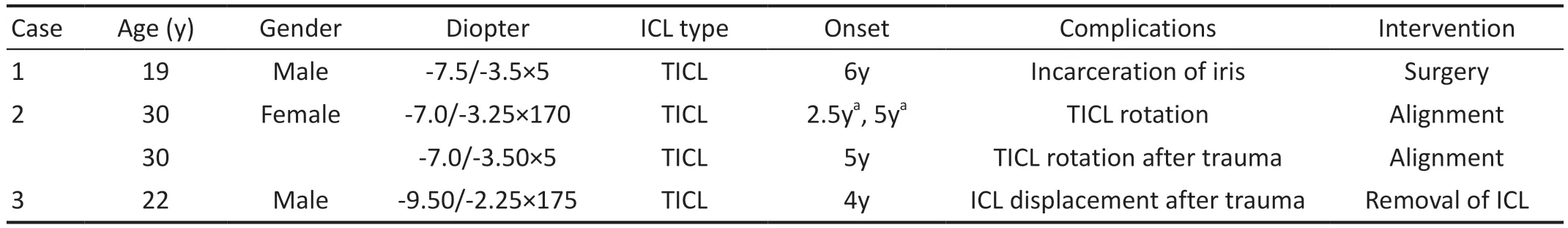
Table 3 Post-implantation adverse events and intervention
The physiological endothelium loss rate[17]of 0.6%/y five years without surgical intervention and the ICL loss rate of about 3.0% were found in a previous study[17], which was much higher than our loss rate of 1.55%.In this retrospective study, the density of the corneal endothelial cells in one eye after surgical implantation was reduced.The patient had no history of secondary surgery and no history of trauma.But the decrease in corneal endothelial count did not cause any clinical symptoms or corneal changes, and the patient was closely followed up.
Our results found that the location of the central hole was more temporal than the nasal position and superior to the inferior location.A previous study by Zhouet al[18]also confirmed that when the pupil was considered as the center, the central hole of ICL was mostly located on the temporal side, but the upper temporal part was more than the lower temporal region.The possible reasons might have been the following: 1) Change of pupil position: In a previous study[19], when the pupil contracted, the pupil center moved to the upper part of the nose and the central hole shifted to the pupil center temporally.2)Impact of Kappa angle: A previous study[20]showed that the average kappa angle of myopia was 5.0°, which was a positive value, indicating that the pupil center of myopia was located at the nasal side, making the central hole position relative to the temporal side of the pupil.3) Iris movement: Ultrasound biomicroscopy (UBM) imaging found that after ICL implantation, the lens made contact with the posterior surface of the iris, which may have caused the ICL to move with the movement of the iris[21].4) The influence of posterior chamber structure: The ciliary body thickness of the nasal side was greater than that of the temporal side[22].It may have caused the ICL shifting to the temporal side.From our observation,the position of the central hole did not change with the time of ICL implantation in the eye, indicating the stability of ICL in the eye.
Based on the visual quality questionnaire outcome, the patients were satisfied and were willing to choose the surgical procedure again.Aligning with the previous study results,more than 91.67% of patients will select the ICL surgery again,and their satisfaction with the surgery was higher than 87.5%[5].In this study, the visual fatigue score was the lowest.The main factors responsible for the lowest score may have been the following: 1) Our patients were generally with a higher degree of myopia, and there might have been insufficient adjustments before the implantation.2) From wearing a pair of glasses to not wearing a pair of glasses, more adjustment functions might have been needed after the surgical implantation.In our study,a detailed evaluation of the symptoms of visual fatigue was not performed.Ametropia and changes in refractory function may have led to visual fatigue after the ICL implantation.A previous study[23]found that the ICL implantation in the posterior chamber affected the lens or suspensory ligament,resulting in a decline in the early postoperative adjustment and a recovery in the late postoperative period, however, after one year postoperatively the adjustment range was still lower than that before surgical implantation.
According to the literature reports on long-term observation after the ICL implantation, adverse events included cataracts,especially anterior sub-capsular opacification.However, the incidence of cataracts in ICL V4c implantation was low and may be more tolerant to low vault than ICL V4 because of the existence of a central hole[2].In this study observation for 5y or more after ICL implantation, no cataracts were found, which may have been related to the ideal lens vault, gentle surgical procedure, and the use of ICL with a central hole, which was consistent with the long-term follow-up study by Alfonsoet al[4].In the present study, the probability of rotation of TICL was 1.8%,including spontaneous rotation in 1 eye and post-traumatic rotation in 1 eye.The TICL rotation may have been related to trauma, inappropriate lens size, ciliary sulcus fixation angle,and low lens vault[24-25].Furthermore, one eye (0.9%) had iris incarceration.The surgical procedure was smooth.One year after the implantation, a small amount of anterior synechia of the iris appeared near the original incision.There was no uncomfort such as redness or eye pain.The IOP was normal,and the vault was 960 μm.The iris incarceration may have been caused by the inadvertent squeezing of the eyeball to the corneal incision by the patient.At the last follow-up visit, a second surgery was performed to remove the iris incarceration.Postoperative UDVA 20/20, IOP, and pupil were normal.
This study also had certain limitations.First, this study was a retrospective study with small sample size.Because of the long follow-up time, some patients who were satisfied with the results of their vision were reluctant to go to the hospital after the surgery.Therefore, the actual results may have been better.A prospective study with a larger sample size in the future is ideal for evaluating the long-term efficacy and safety of ICL implants.Second, the visual quality indicators such as aberration and OSI were not measured before the ICL surgery.To better evaluate the visual quality after the ICL implantation,we will measure the visual quality before and after the ICL implantation in the future.
In conclusion, ICL V4c implantation was safe and effective for the correction of high myopia up to 5y after surgery.The ICL was stable the position of the central hole was mostly located on the temporal side, which was still worth further exploration.And patient satisfaction was high.It also showed an excellent visual acuity, and there were few adverse reactions, but be ware of the degree increase caused by axial length.Education on the necessity of postoperative examination should be encouraged and proper follow-up should be done.In the long run, ICL implantation might be an alternative method to correct myopia.
ACKNOWLEDGEMENTS
Foundations:Supported by the Science and Technology Innovation Program of Hunan Province, China(No.2020SK50103); Hunan Clinical Medical Technology Innovation Guiding Project in 2020.
Conflicts of Interest:Chen X,None;Li L,None;Rao J,None;Chen YX,None;Gao Y,None;Huang RX,None;Zhou QZ,None.
 International Journal of Ophthalmology2023年7期
International Journal of Ophthalmology2023年7期
- International Journal of Ophthalmology的其它文章
- Chickenpox followed streaky multifocal choroiditis with prednison treatment in a girl with asthma
- Pneumonia and ocular disease as the primary presentations of Takayasu arteritis: a case report
- Unilateral blurred vision in pediatric patient associated with cavum velum interpositum cyst
- Highly cited publication performance in the ophthalmology category in the Web of Science database:a bibliometric analysis
- Comparison of efficacy of conbercept, aflibercept, and ranibizumab ophthalmic injection in the treatment of macular edema caused by retinal vein occlusion: a Metaanalysis
- Ocular manifestations and quality of life in patients after hematopoietic stem cell transplantation
