Technique of using Cionni-modified capsular tension ring in the management of severely traumatic lens subluxation
Hao Jiang, Wei Zhang, Yan-Hua Chu
Tianjin Eye Hospital, Tianjin Key Lab of Ophthalmology and Visual Science, Tianjin Eye Institute, Clinical College of Ophthalmology Tianjin Medical University, Tianjin 300020,China
Abstract● AlM: To investigate the effect of Cionni-modified capsular tension ring (CTR) implantation in patients with severely traumatic subluxated cataracts.
● KEYWORDS: Cionni-modified capsular tension ring;subluxated traumatic cataracts; surgical technique;intraocular lens decentration; intraocular lens tilt
INTRODUCTION
Subluxated lenses are a major challenge for cataract surgeons.Subluxated lenses can be congenital (e.g., Marfan syndrome and microspherophakia) or acquired (e.g., ocular trauma)[1].Severe zonular instability increases the risks of cataract extraction during and after surgery.Cionni and Osher[2]proposed the concept of the capsular tension ring (CTR).The CTR can be used to treat mild zonulopathy[3].However,implantation of the CTR in eyes with greater zonular damage could not achieve sufficient stabilization and concentration of the intraocular lens (IOL) and the capsular bag.
In the case of traumatic lens subluxation, the degree of zonular destruction may be very severe and accompanied by the presence of vitreous in the anterior chamber (AC)[4].In addition, there could also be other problems that require additional treatment, such as traumatic mydriasiss, increased intraocular pressure (IOP), and iridodialysis.When these conditions are present, it is often difficult to maintain and stabilize the capsular bag.Cionniet al[5]developed a modified CTR (another name is Cionni-CTR) for cataract surgeries with significant zonular dialysis or compromise in eyes.The modified CTR is based on the traditional open-loop CTR, which has a fixation eyelet forward, thus enabling suture fixation of the modified CTR and IOL and capsular bag complex to the sclera[6].In our research, we reported the clinical characteristics and postoperative effects of patients with traumatic cataract and zonulopathy who underwent phacoemulsification and received a modified CTR and a posterior IOL.
SUBJECTS AND METHODS
Ethical ApprovalAll patients were given appropriate written informed consent.This research followed the purpose of the Helsinki Declaration.This study was approved by the Medical Ethics Committees of Tianjin Eye Hospital (KY-2023011).
We retrospectively reviewed 20 eyes of 20 patients who had traumatic subluxated cataracts with at least 6-clock hours of zonular loss or weakness who underwent cataract surgery by one surgeon (Jiang H) at the Tianjin Eye Hospital from January 1, 2017, to September 1, 2020.
We examined corrected distance visual acuity (CDVA)by a Snellen chart and converted it to logMAR value.We used the SRK II formula to evaluate the degree of the IOL implanted with Cionni-modified CTR.The degree of zonular loss or weakness was intraoperatively evaluated based on the amount of displacement and mobility of the lens.We used a single-point fixed capsular tension device to treat zonulysis at 6-8 clock hours.We used a double-point fixed capsular tension device to treat zonulysis of 8-12 clock hours.The complications included IOL decentration, retinal detachment and posterior capsule rupture (PCR).
Biomicroscopic examination was used to calculate the preoperative lens decentration and tilt[7].The grades of lens tilt are shown: D = severe (>45 degrees); C = marked (31-45 degrees); B = moderate (16-30 degrees); A = mild (<15 degrees); N = none.The grades of lens decentration are shown:D = severe (lens and lens equator not seen through dilated pupil); C = marked (lens equator seen through dilated pupil with aphakic optical axis); B = moderate (lens equator seen through dilated pupil with phakic optical axis); A = mild (lens equator not seen through dilated pupil with phakic optical axis); N = none.
Ultrasound BiomicroscopyWe performed ultrasound biomicroscopy (UBM) examination on all patients.Scans were performed with the undilated eye in the central position.The scan clip for each eye was recorded and selected for analysis.A scleral spur (SS) shows a hyperechoic area resembling an olecranon (elbow shape) in UBM images.We considered the line between the two olecranons as the baseline for the position of the IOL.Two perpendicular lines were drawn from the two optical endpoints of the IOL to the baseline, and the distance between the SS and intersection points was measured for analysis of IOL decentration.IOL decentration is equal to half the difference between these two distances (Figure 1).IOL tilt is assessed by the angle (θ) formed by the line between the baseline and the two optical endpoints (Figure 1).
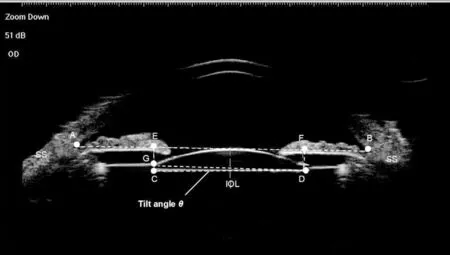
Figure 1 Measurement of intraocular lens (IOL) decentration and tilt on ultrasound biomicroscopy images of the anterior segment A line (line AB) was drawn between the two scleral spurs (SS) as the baseline for referencing the position of the IOL.Draw two vertical lines from the two optical end-points (C and D) of the IOL to the baseline with intersection points (E and F).The IOL decentration was equal to half of the difference between distances AE and FB.The IOL tilt was determined by the angle formed by the line between the two optical endpoints and the baseline.The tilt angle θ was calculated by the formula: θ = arctan CG/DG = arctan (CE-DF).
Surgical TechniqueThe same surgeon (Jiang H) performed all the surgeries under retrobulbar anesthesia.A 3.2-mm transparent corneal tunnel incision was made.a 0.9-mmwide puncture was made to insert a chopper.Then, we used Healon (Alcon Laboratory, USA) to maintain the AC.We used capsulorhexis forceps to make a 5.5-mm-wide central capsulorhexis.Then, we used a disposable pouch retractor to engage the capsulorhexis to center and stabilize the lens.Then, we performed hydrodissection.We used the phaco/chop technique and cortical aspiration by centurion phacoemulsification (Bausch & Lomb Inc.USA) to perform nuclear endocapsular phacoemulsification.We performed phacoemulsification at a low flow rate, and the infusion bottle height was 80 cm.The capsular bag and AC were filled with Healon.We implanted a foldable IOL into the capsular bag.Then, the Healon was removed behind the IOL by an I/A device.
According to the surgeon's assessment of zonal weakness during the operation, the type of modified CTR implantation was decided intraoperatively.When the loss or weakness of the zonules was less than 8 clock hours, a single-eyelet CTR was used.When it was 8 clock hours or more, a double-eyelet CTR was used.The 10-0 polypropylene suture was passed through the eyelets of Cionni-modified CTR.After that, the Cionnimodified CTR was passed into the capsular bag through the main incision by using a chopper and a tying forcep.The eyelet was located at the midpoint of the area of zonular dialysis anterior to the capsulorhexis.Then, we moved the suture needle under the scleral flap.We used central capsulorhexis to perfectly provide centration of the capsular bag by adjusting the suture and then sutured the Cionni-modified CTR to the sclera.After inflating the capsular bag with Healon, a foldable IOL was implanted into the capsular bag.Then, we used a biaxial I/A tip to remove the ophthalmic viscosurgical device.Some ophthalmic viscosurgical devices remained above the zonular dehiscence area.All the incisions were hydrated to check the stability.
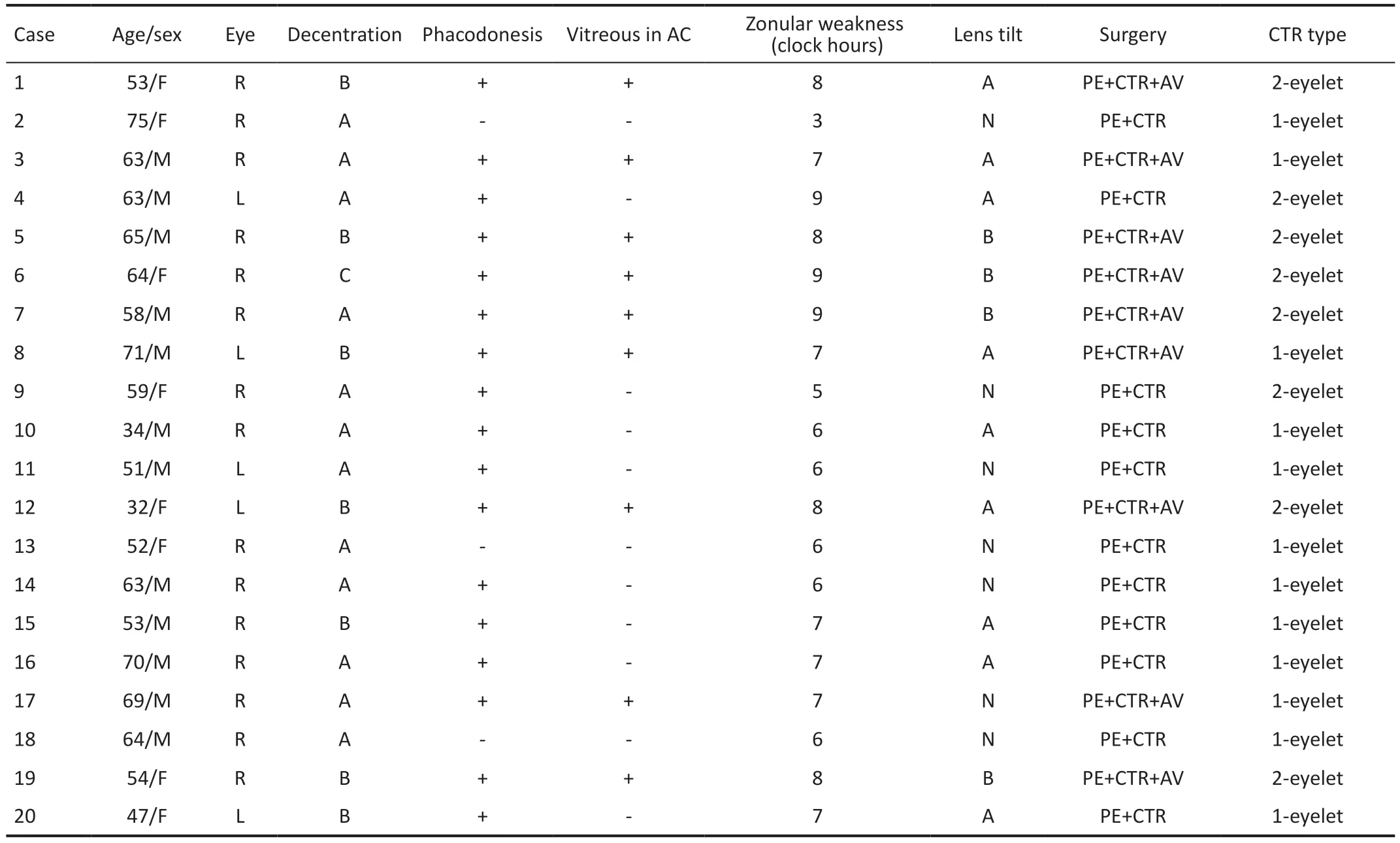
Table 1 Preoperative and intraoperative characteristics
After the operation, patients were topically given 0.1%pranoprofen (Alcon Laboratory Inc.USA) and 0.1% tobradex(Alcon Laboratory Inc.) four times daily for 7d, and then the dose was gradually reduced every week.
Statistical AnalysisThe result is presented as the mean±standard deviation (SD).Snellen visual acuity was changed to the logarithm of the minimum angle of resolution(logMAR).The Shapiro-Wilk test was used to confirm the normality of data distribution.The Student'st-test and Mann-WhitneyUtest were used to analyze the parametric and nonparametric data, respectively.The differences were considered statistically significant atP<0.05.
RESULTS
The mean age of the patients was 58.0±11.3 (range 32 to 75)y in the study (Table 1).The mean duration of follow-up was 17.3±12.8 (range 6 to 48)mo.Eight patients received a doubleeyelet CTR, and 12 patients received a single-eyelet CTR.The preoperative mean CDVA was 0.83±0.24 logMAR, and the postoperative average CDVA was 0.23±0.30 logMAR(P<0.05).Only 5 of the 20 eyes (25%) preoperatively had a CDVA of 20/80 or better compared with 18 eyes at the last visit (90%,P<0.05).The poor vision in the other 2 eyes at the last visit was due to posterior capsule opacification (PCO).At the last visit, 16 eyes (80%) had a CDVA of 20/40 or higher.Ten patients were followed up for at least one year, and 7 eyes had a CDVA of 20/40 or higher (70%) during the year.
Preoperatively, 8 eyes (40%) developed symptomatic decentration (grades 2 and 3; Table 1).During the surgery, all 20 eyes had centered IOLs (Figure 2A, 2B).At the last visit,the postoperative horizontal and vertical IOL decentration was 0.27±0.12 mm and 0.41±0.19 mm, respectively.No symptomatic decentration occurred in the eyes during the entire follow-up (P<0.05; Table 2; Figure 2C, 2D).Preoperatively,13 eyes (65%) had posterior lens tilt (Grade 1 or 2).At the last visit, the postoperative vertical and horizontal IOL tilts were 5.5°±2.5° and 6.1°±2.2°, respectively.
The preoperative examination revealed that 9 eyes (45%) of the AC had vitreous.Due to the presence of vitreous in the AC,9 eyes (45%) required bimanual anterior vitrectomy.These nine eyes preoperatively had vitreous prolapse with at least 6 clock hours of zonulysis.There were no cases of vitreous in the AC after surgery.There was also no endophthalmitis or retinal detachment.Eight eyes (40%) had PCO that was severe enough to cause poor vision.We performed neodymium(Nd):YAG laser capsulotomy on these eyes when the CTR was stabilized.
DISCUSSION
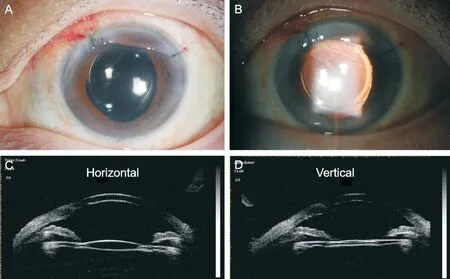
Figure 2 Representative anterior segment photography and ultrasound biomicroscopy photography A, B: Anterior segment photography illustrating the centered intraocular lens (IOL); C, D: Ultrasound biomicroscopy examination illustrating no symptomatic decentration of IOL.
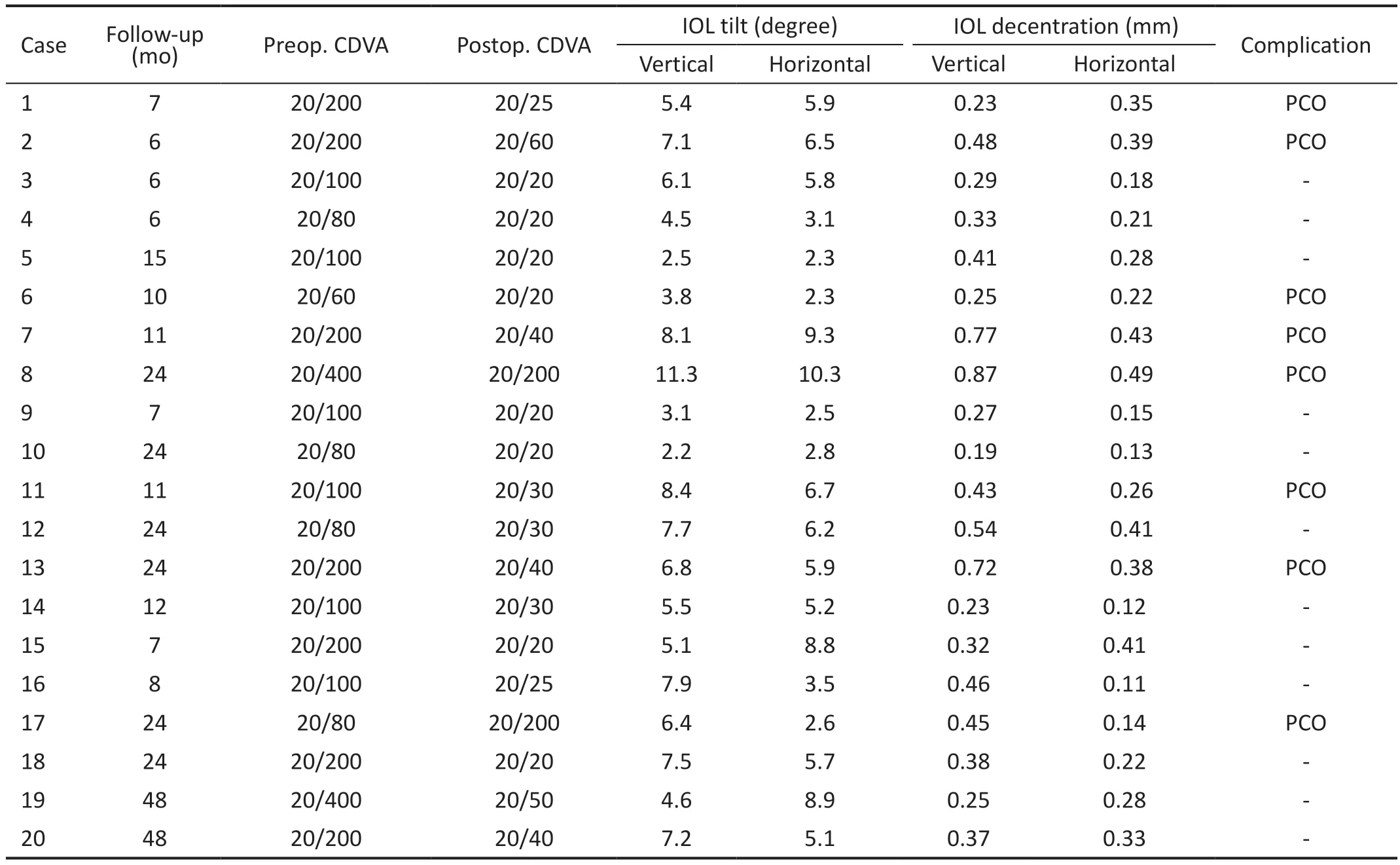
Table 2 Postoperative characteristics
Cataract surgery is difficult in traumatic eyes with zonular insufficiency or subluxation of the lens.Previously,intracapsular cataract extraction (ICCE) was necessary for patients with zonular dialysis[8].The capsular bag could not be saved in most cases.Implantation of AC IOL or sutured IOL to the sclera can cause several complications, such as glaucoma or retinal detachment[9-10].Cionniet al[5]reported an endocapsular ring with a fixed hook for use in eyes with zonular insufficiency.The CTR can be sutured to the sclera with the aid of this hook and without disrupting the capsular bag integrity.Another study reported that it is a relatively effective and safe option to use this Cionni-modified CTR with IOL implantation for the treatment of lens pediatric and adult eyes with zonular deficiency and subluxation of different etiologies[11].However,the effects of Cionni-modified CTR implantation on patients with traumatic subluxated cataract are relatively few.
CTR provided adequate stability and lens centration in the eye with less than 6 clock hours of zonular loss[12].It was found that the modified CTR was effective in maintaining capsular expansion in eyes with extensive zonular deficiency[13].When used together with iris hooks, this expanded capsular bag helped to maintain the vitreous back.The CTR served to lift the bag up against the iris and effectively isolated the AC from the vitreous cavity.The formation of a seal between the vitreous cavity and the AC helped prevent further aqueous misdirection and vitreous prolapse during phacoemulsification, which may lead to the posterior capsule moving forward, resulting in polymerase chain reaction (PCR)[14].However, it is difficult to insert surgical devices when patients present with dense cataracts or extensive zonular deficiency.Raiet al[15]found that inserting CTR as early as possible created additional pressure on the intact zonules, which led to further zonular deficiency.Therefore, a recommendation was made to delay CTR insertion as safely as possible.In the present study, the Cionnimodified CTR allowed implantation of IOL in the bag and intraoperatively promoted capsular bag centration.A minimal decentration of the IOL may occur in eyes with a single-eyelet CTR at the early postoperative period, and the decentration of the IOL was in the direction of fixation.In our study, the surgeon's assessment of zonular weakness determined which type of CTR to implant, as in other studies[16-17].Ocular trauma may have a more global angle of zonular weakness or dialysis than the intraoperatively estimated angle.Kimet al[18]showed that 6 (6.7%) of 90 eyes had symptomatic IOL decentration with an average follow-up of 17.8mo, and these cases were all caused by 10-0 polypropylene breakage.These cases involved pediatric eyes and adult eyes.Gurleret al[19]reported that after an average follow-up of 24mo, 6% of pediatric eyes needed secondary sutures for decentration of the IOL.Vasavadaet al[20]did not reveal symptomatic decentration of the IOL in eyes with traumatism, which is similar to our findings.The use of 10-0 polypropylene gives good immediate results, but the suture may disintegrate after several years, and this method needs to be improved in the future.
In the present study, the amount of IOL decentration and tilt measured by UBM was 0.48±0.24 mm of vertical IOL decentration, 0.32±0.13 mm of horizontal IOL decentration,6.1°±2.6° of horizontal IOL tilt, and 5.5°±2.6° of vertical IOL tilt.All eyes in our study showed improved CDVA at the last postoperative examination.Goel reported that 20 of 22 eyes with traumatic zonular loss had elevated CDVA[21].Zhaoet al[22]reported that in the capsular bag fixation group,horizontal IOL decentration was 0.22±0.17 mm, vertical IOL decentration was 0.25±0.19 mm, horizontal IOL tilt was 4.04±2.45 degrees, and vertical IOL tilt was 4.75±2.27 degrees,which was similar to our results.Furthermore, posterior segment pathology could be masked by cataracts in some cases and was not observed.Therefore, patients who have traumatic cataracts should be informed and warned of posttraumatic complications that may be found postoperatively.In the present study, there were no posterior segment complications associated with cataract surgeries, such as retinal detachment and macular edema.Due to the presence of vitreous in the AC during surgery, nine eyes required binocular anterior vitrectomy.PCO occurred in 8 eyes (45%) and was the most common visual complication after surgery.A study has shown that using intracapsular tension rings can reduce the secondary proliferation of lens epithelial cells[23].However, the Cionnimodified CTR had a fixed hook that lifted the anterior capsule away from the IOL, which facilitated lens epithelial cell migration into the capsule[24].In our study, we consider that the posterior capsule waves during the operation and the lens cortex are difficult to completely remove, which may lead to PCO after the operation.Thus, we performed Nd:YAG laser capsulotomy in these eyes, after which CTRs were stabilized.Our study indicated that it was safe to use Nd:YAG capsulotomy in eyes with traumatic cataract extraction and implantation of modified CTR.Daiet al[25]showed that phacoemulsification with CTR implantation combined with ophthalmic endoscope-controlled goniosynechialysis is safe and effective in the treatment of secondary angleclosure glaucoma induced by traumatic lens subluxation.Jianget al[26]proved that four-eyelet CTR can effectively increase the rotational stability of toric IOLs in cataract patients with high myopia and astigmatism.The above studies confirmed the good results of using CTR in patients with glaucoma and high myopia.In our study, we further found that capsular bag preservation and better IOL concentration can be achieved without major complications in patients with severely traumatic subluxated cataracts.
In summary, although the surgeries are time-consuming and technically challenging and the learning curve is steep, the capsular bag could be saved in severely traumatic subluxated cataracts by using modified CTR.By inserting a disposable pouch retractor to engage the capsulorhexis to the center before phacoemulsification and fixing the CTR after implantation of the IOL, complications can be minimized, and good visual effects can be obtained in these damaged eyes.
ACKNOWLEDGEMENTS
Foundations:Supported by the National Natural Science Foundation of China (No.82070968); China Postdoctoral Science Foundation (No.2022M712386); Tianjin Health Research Project (No.TJWJ2022MS040; No.ZC20166);Nankai University Eye Institute (No.NKYKK202203;No.NKYKK202206); Tianjin Eye Hospital Research Project(No.YKYB1902); Natural Science Foundation of Tianjin(No.20JCQNJC01860); Tianjin Key Medical Discipine(Specialty) Construction Project (No.TJYXZDXK-016A).
Conflicts of Interest: Jiang H,None;Zhang W,None;Chu YH,None.
 International Journal of Ophthalmology2023年7期
International Journal of Ophthalmology2023年7期
- International Journal of Ophthalmology的其它文章
- Chickenpox followed streaky multifocal choroiditis with prednison treatment in a girl with asthma
- Pneumonia and ocular disease as the primary presentations of Takayasu arteritis: a case report
- Unilateral blurred vision in pediatric patient associated with cavum velum interpositum cyst
- Highly cited publication performance in the ophthalmology category in the Web of Science database:a bibliometric analysis
- Comparison of efficacy of conbercept, aflibercept, and ranibizumab ophthalmic injection in the treatment of macular edema caused by retinal vein occlusion: a Metaanalysis
- Ocular manifestations and quality of life in patients after hematopoietic stem cell transplantation
