Two-step strategy—conjunctival flap covering surgery combined with secondary deep anterior lamellar keratoplasty for the treatment of high-risk fungal keratitis
Abstract● AlM: To investigate whether the two-step strategy[conjunctival flap covering surgery (CFCS) combined with secondary deep anterior lamellar keratoplasty (DALK)] is effective for patients with high-risk fungal keratitis (FK).
● KEYWORDS: high-risk; fungal keratitis; conjunctival flap;deep anterior lamellar keratoplasty; two-step strategy
INTRODUCTION
Fungal keratitis (FK) is a leading cause of ocular morbidity worldwide, especially in developing countries[1-3].Corneal perforation or the need for therapeutic penetrating keratoplasty (TPK) occurs in up to 50% of severe FK[4].After identifying high-risk of corneal perforation, TPK is indicated[5].However, TPK performed during the period of acute infection is accompanied by a high incidence of intraoperative complications, fungal recurrence, and graft failure[6-7].Moreover, the severe shortage of fresh donor corneas also limited its application[8].
Gundersen[9]first described the technology of using conjunctival flap (CF) covering surgery (CFCS) to treat corneal ulcer in the late 1950s.CF not only prevents tears,proteolytic enzymes, and proinflammatory mediators from reaching the corneal ulcer but also provides an abundance of cellular components and growth factors, to increase the resistance against infection and corneal melting[10-11].CFCS as a simple and economical method has been widely applied in the treatment of refractory FK[12-13].
After stabilizing the cornea by CFCS, secondary deep anterior lamellar keratoplasty (DALK) could be performed to restore the clarity of cornea.Compared to TPK, the advantages of DALK include lower rate of intraoperative complications,longer graft survival and less dependent on fresh donor corneas[14-17].
Herein, we reported our clinical experiences and insights from 10 consecutive patients who were identified as highrisk and accepted the two-step strategy (CFCS combined with secondary DALK).The aim of the study was to investigate whether this two-step strategy is effective in transforming intentional TPK during acute infection to later optical DALK.
SUBJECTS AND METHODS
Ethical ApprovalThis noncomparative, retrospective case series was approved by the Ethics Committee of Union Hospital, Tongji Medical College, and Huazhong University of Science and Technology according to the tenets of the Declaration of Helsinki (UHCT22982).Informed consent was waived due to the retrospective nature of the study.
SubjectsConsecutive 10 patients (10 eyes) with high-risk FK between March 2021 and November 2022 were enrolled in the study.Patients who met the following high-risk criteria were included: 1) fungal hyphae were detected byin vivoconfocal microscopy (IVCM); 2) poorly respond to topical antifungal medications after 7d treatment; 3) the width of infiltration was more than 6.63 mm; 4) the infiltration involved the posterior 1/3 of the corneal stroma; and 5) with hypopyon and endothelial plaques.Participants were excluded by the following criteria 1) other types of keratitis; 2) FK with corneal perforations.
Medication ProceduresParticipants were received topical eyedrops hourly including 0.15% amphotericin B (XinYa,Shanghai, China) and 1% voriconazole (VCZ; Pfizer, New York, USA) for 2wk, every 2h for at least 6wk.Oral VCZ was administrated 200 mg twice daily for 4wk.The response to therapy was noted on slit lamp examination.To avoid posterior synechiae of the iris and reduce the inflammatory, 1% atropine and 0.1% bromfenac sodium eye drops were used.Hepatic and renal functions were monitored regularly.
Surgical TechniquesThe first step was performed under topical anesthesia and retrobulbar anesthesia by 2% lidocaine.First, the corneal lesion was removed until the residual cornea was smooth (Figure 1A, 1B).The edge of lesion was cut smooth to facilitate epithelial healing (Figure 1B).Subsequently, 0.1 mL VCZ (100 μg/0.1 mL) was injected in 4-5 divided doses around the infiltrate to form a drug deposit around the circumference of the lesion (Figure 1C).Finally,a bipedicle CF with partial Tenon's capsule was dissected according to the location and size of the ulcer; then the CF was loosely sutured with a 10-0 nylon to the cornea (Figure 1D).
After stabilization of the ocular surface and healing of the ulcer (Figure 1E), the second step was performed under general anesthesia.Briefly, the size of trephination was chosen according to the size of the scar diameter.After trephination to approximately 50% of corneal thickness, a 27-guage pneumatic needle was inserted into the stroma up to the center of the cornea.Air was injected gently into the mid-stroma until a big bubble (Figure 1F), or a group of small bubbles was formed extending beyond the border of trephination.Then,the corneal scar was removed layer by layer until the residual cornea was smooth without obvious opacification.The big bubble was punctured with a 63 μm-microtoothed forceps to allow escape of the air and collapse of the bubble (Figure 1G).Finally, glycerol cryo-preserved corneal graft with appropriate size and thickness was sutured interruptedly with a 10-0 nylon(Figure 1H).
Postoperative Management and Follow-upFollowing CFCS and DALK, routine examinations including visual acuity and slit-lamp examination were performed every day for 1wk.All patients were followed up daily for 1wk, biweekly for 1mo, monthly for 3mo, and then at different intervals after surgery.Sutures of the CFCS were removed 3-4wk postoperatively.Suture removal for DALK was 3-6mo.The main outcome measures were healing of the ulcer, recurrence of FK, reject reaction, best corrected visual acuity (BCVA) and relevant complications.Surgical success was defined as the survival of conjunctival and corneal graft.Failure was defined as corneal perforation or recurrence of FK or eyeball removal.Statistical AnalysisStatistical analysis was performed using SPSS 25.0.Demographic data and clinical variables were presented as mean±standard deviation (SD).
RESULTS
Baseline CharacteristicsTen patients with 6 males(60%) and 4 females (40%) detected fungal hyphae through IVCM were included in this study.The average age was 56.5±7.1y, ranging from 47 to 72y.The average diameter of corneal infiltrates was 7.50±0.39 mm, ranging from 6.94 to 8.13 mm.The mean depth of corneal infiltrates by anterior segment optical coherence tomography (AS-OCT)was 422.4±77.1 μm, ranging from 350 to 535 μm.The mean corneal thickness was 597.4±117.3 μm, ranging from 458 to 851 μm.Hypopyon and endothelial plaques were presented in all patients.Seven patients were fungal culture positive.Three of them were Fusarium specie and 4 were aspergillus specie(Table 1).
Prognosis Following Two-Step StrategyAfter the first CFCS, all fungal corneal ulcer healed within 4wk.The antifungal medications were withdrawn within 12wk.All patients competed DALK successfully within 5 (mean 3.65±0.9,ranging from 3 to 5)mo.The graft diameter was 7.75±0.39 mm.At the last follow-up (average 9.25±3.39, ranging from 5.5 to 17mo), no fungal recurrence or graft rejection appeared, and all patients showed improvement of BCVA.The mean final BCVA was 0.38±0.14, ranging from 0.15 to 0.6 (Table 1).One patient suffered from liver function impairment due to oral voriconazole for 4wk and recovered spontaneously after 1wk of drug withdrawal.
Representative Case Reports
Mild corneal opacity after DALK (Case 1)A 55-year-old female patient presented with a 7.2 mm width of central corneal ulcer and 1 mm hypopyon in her left eye (Figure 2A).IVCM detected a large number of fungal hyphae (Figure 2B)and later fungal culture result showedAspergillus specie(Figure 2B, insert).Her corneal thickness was 851 μm and the depth of infiltrate was 535 μm (Figure 2C).She was poorly responded to topical and oral antifungal medications after 7dtreatment and then CFCS was performed.The ulcer healed and the cornea became stable with a leucoma and superficial conjunctiva 3mo after the first step (Figure 2D).At 10mo follow-up after DALK, the BCVA was 0.3 although the central host cornea remained mild opacity (Figure 2E and 2F).ASOCT showed the corneal thickness was 524 μm and the residual host cornea was 95 μm (Figure 2F).
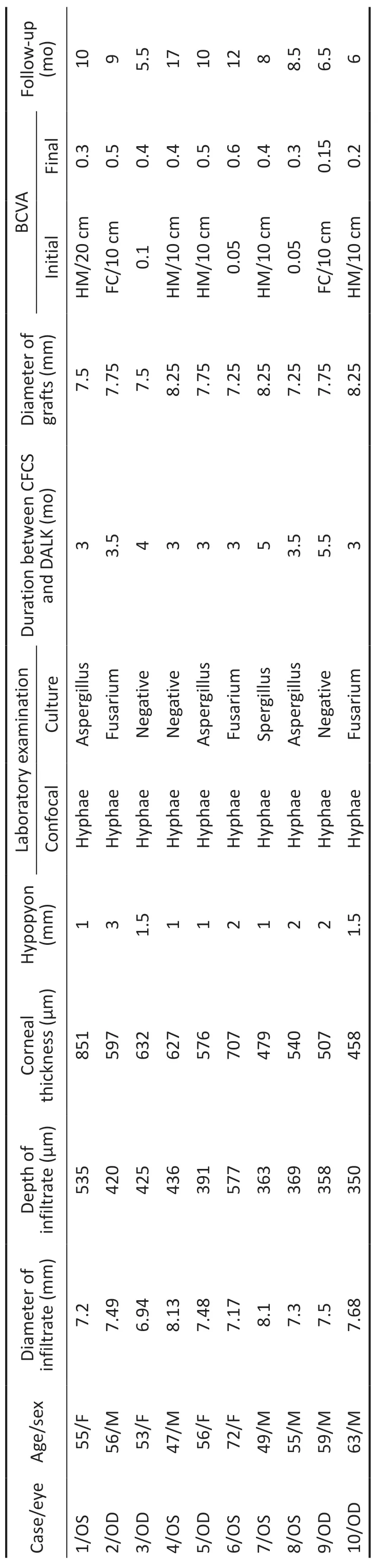
Table 1 Relevant clinical data of patients
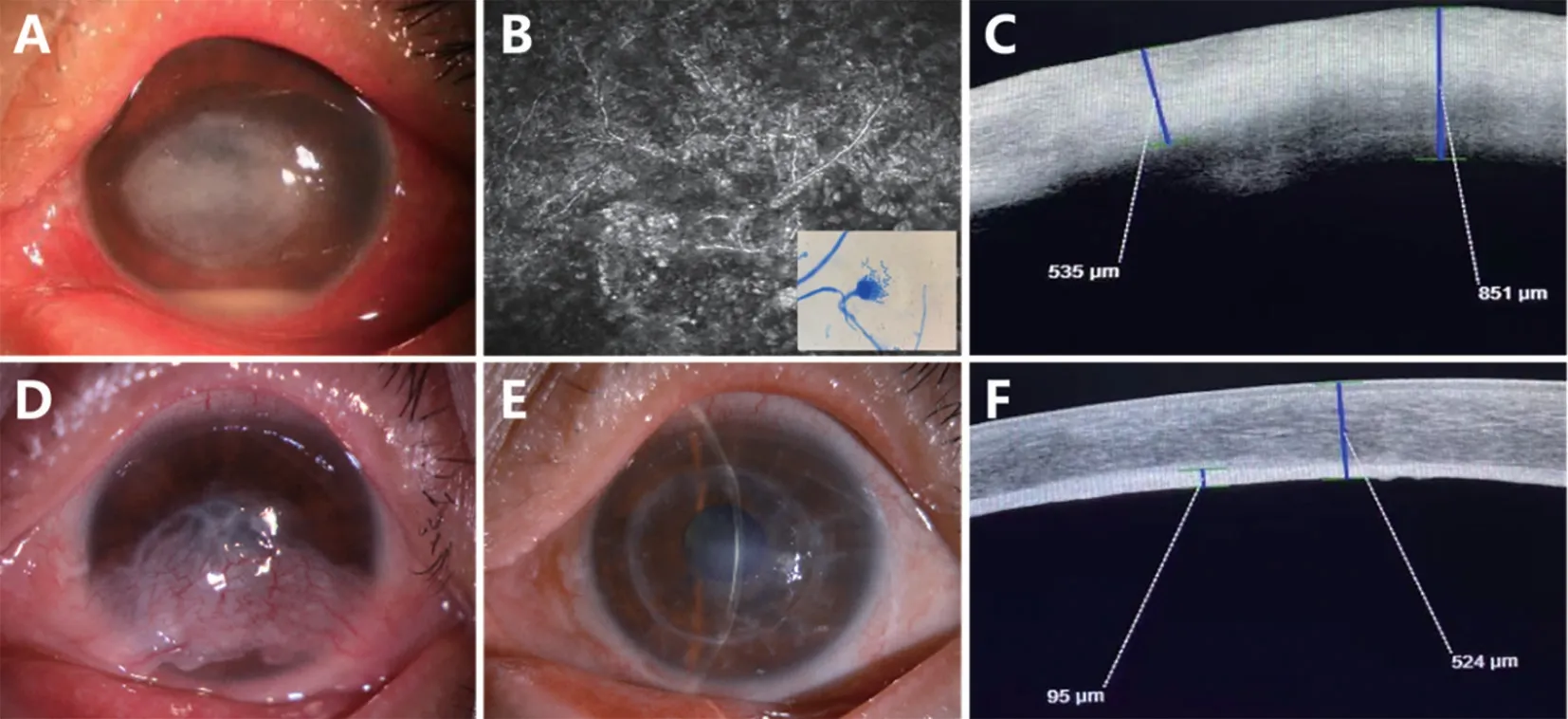
Figure 2 Case 1, slit-lamp photographs and examinations of a 55-year-old female with central corneal ulcer A: The patient presented with a 7.2 mm central corneal ulcer, 1 mm hypopyon in her left eye; B: Fungal hyphae were detected under IVCM and the cultured pathogen was Aspergillus specie (insert); C: The depth of infiltrate was 535 μm; D: The cornea became stable 3mo postoperatively; E, F: The central cornea remained mild opacity 10mo after DALK with 95 μm residual host cornea.IVCM: In vivo confocal microscopy; DALK: Deep anterior lamellar keratoplasty.
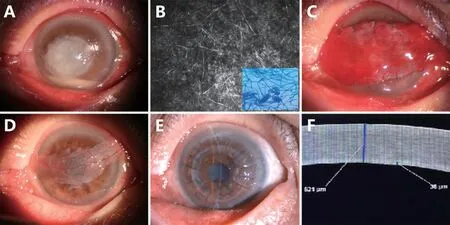
Figure 3 Case 6, photographs of a 72-year-old FK patient after plant-related trauma A: A large fungal ulcer with 2 mm hypopyon was observed by slit-lamp examination; B: Hyphae were detected and the cultured pathogen was Fusarium specie (insert); C: CFCS was performed successfully; D: A stable ocular surface was obtained 3mo after CFCS; E: A transparent cornea was reconstructed 3mo after DALK; F: The residual host cornea was 38 μm.FK: Fungal keratitis; CFCS: Conjunctival flap covering surgery; DALK: Deep anterior lamellar keratoplasty.
Transparent cornea after DALK (Case 6)A 72-year-old female patient was referred because of a 7.17 mm width of central corneal ulcer in her left eye after plant-related trauma(Figure 3A).IVCM revealed fungal hyphae (Figure 3B) and the cultured pathogen wasFusarium specie(Figure 3B, insert).After 7d treatment, CFCS was performed (Figure 3C).A stable ocular surface was obtained 3mo postoperatively (Figure 3D).A transparent cornea was restored 3mo after DALK (Figure 3E).AS-OCT showed the corneal thickness was 521 μm and the residual host cornea was 38 μm (Figure 3F).Her BCVA was 0.6 at the 12mo follow-up.
DISCUSSION
FK carries a relatively poor prognosis compared to other forms of infectious keratitis due to delays in microbiological identification, suboptimal efficacy and permeability of antifungal agents[3].Corneal perforation or the need for TPK occurs in up to 50% of severe FK[4].A secondary analysis of the Mycotic Ulcer Treatment Trial II defined the high-risk of corneal perforation or need for TPK as an infiltrate size of more than 6.63 mm, an infiltrate involving the posterior 1/3 of the stroma, and a hypopyon[5].In addition, endothelial plaques are considered as a sign of hyphae infiltrating Descemet's membrane.Once plaques are presented, TPK instead of DALK should be performed to reduce the risk of fungal recurrence[18].It has been well accepted that outcomes of TPK fare worse than those for optical DALK[14-16].Our results demonstrated that the two-step strategy is effective in transforming intentional TPK during acute infection to later optical DALK in high-risk FK.
Natamycin (NTM) is the most commonly used topical antifungal agent.It is currently the only drug approved by the United States Food and Drug Administration (USFDA) for the treatment of FK[19].But for various reasons in our region,NTM is not available.In this circumstances, VCZ has been the second-best topical drug for FK[3].Similar to NTM, VCZ shows a wide range of activity againstFusarium species.VCZ can be administered by a variety of routes, such as oral capsule form, intra- and stromal injection, and intravitreal injection route.Meanwhile, amphotericin B displays fungicidal activity for treatment of fungal ulcers[7].
CF rich in blood vessels and lymphatics provides an abundance of cellular components and growth factors to increase the resistance against infection and corneal melting[10-11].Many investigators have used CF to treat FK resistant to medical treatment[12-13].Besides, CF is economically easy to obtain, and CFCS could be performed by majority of ophthalmologists.In our study, an oversized full-thickness CF with partial Tenon's capsule was sutured loosely over the cornea to ensure adequate blood supply and avoid conjunctival flap necrosis.
The disadvantages of CFCS include poor cosmetics, low postoperative vision.DALK should be performed after the cornea is stable.With the improvement of surgical skills,ophthalmologists have attempted to perform pneumatic assisted DALK in patients[20].The use of glycerol cryopreserved cornea alleviates the severe shortage of fresh donor cornea[8].The retainment of recipient endothelium avoids the incidence of endothelial immune rejection[14-16].
Through clinical studies, other surgical techniques may be effective for FK, but there is no uniform recommendation.Collagen crosslinking (CXL) has antibacterial and corneal tissue strengthening properties, but its effectiveness against FK remains controversial.Some researchers have shown that adjuvant CXL therapy is effective in promoting ulcer healing,while others argue that CXL is not helpful for FK, especially in treating Fusarium infection[21-22].Periodic corneal debridement has been shown to increase the number of surgeries and prolong the treatment period, which may increase corneal scarring and accelerate corneal perforation.Finally, TPK is indicated for patients who do not respond to targeted drug therapy, corneal ulcers associated with corneal thinning (where intracellular therapy has a high risk of corneal perforation),and corneal perforation that occurs during drug therapy[23].However, TPK performed during acute infection is associated with a high incidence of intraoperative complications, fungal recurrence, and graft failure.In addition, the severe shortage of fresh donor corneas also limits its application[24].For TPK,two risk factors for graft failure were identified: size of corneal infiltrate and size of the corneal graft[7,24].In our study, the fungal pathogens have been eradicated before secondary DALK.The size of the graft should be larger than that of corneal opacity, and the cloudy corneal stroma was removed as deep as possible to reach the Descemet's membrane.This ensures that the cloudy cornea is removed as much as possible while minimizing rejection.It is undeniable that the cloudy corneal stroma might not be completely removed in some severe cases of corneal opacity especially when big bubble cannot be formed during keratoplasty.Penetrating keratoplasty will be necessary in this situation.Keratoprosthesis surgery will be recommended if repeated graft rejection happens after penetrating keratoplasty[25].
The limitations of the present study included a lack of controls and a small sample size.Besides, the two-step strategy has a long period of recovery.Nevertheless, the two-step strategy successfully transformed intentional TPK during acute infection to later optical DALK in high-risk FK.
In conclusion, the two-step strategy is safe and effective in the treatment of high-risk FK by transforming intentional TPK during acute infection to later optical DALK.The first step of CFCS avoids the recurrence of FK and corneal perforation,and the second step of DALK restores the corneal clarity and satisfactory visual acuity.It is a practical strategy, especially in areas lacking fresh donor corneas and eye bank services.
ACKNOWLEDGEMENTS
Authors’contributions:Conceptualization, Xie HT and Zhang MC; methodology, Xie HT, Zhang MC, and Wang JS; writing—original draft preparation, Wang YC, Wang JS,Wang B, and Peng X; writing—review and editing, Xie HT and Zhang MC; supervision, Xie HT and Zhang MC; project administration, Zhang MC; funding acquisition, Xie HT and Zhang MC.
Foundations:Supported by the National Natural Science Foundation of China (No.82171025; No.82070934); the Fundamental Research Funds for the Central Universities(No.HUST: 2019kfyXMBZ065); the Key Research and Development Program of Hubei Province (No.2021BCA146);the Clinical Research Foundation of Wuhan Union Hospital(No.2021xhlcyj03).
Conflicts of Interest:Wang YC,None;Wang JS,None;Wang B,None;Peng X,None;Xie HT,None;Zhang MC,None.
 International Journal of Ophthalmology2023年7期
International Journal of Ophthalmology2023年7期
- International Journal of Ophthalmology的其它文章
- Chickenpox followed streaky multifocal choroiditis with prednison treatment in a girl with asthma
- Pneumonia and ocular disease as the primary presentations of Takayasu arteritis: a case report
- Unilateral blurred vision in pediatric patient associated with cavum velum interpositum cyst
- Highly cited publication performance in the ophthalmology category in the Web of Science database:a bibliometric analysis
- Comparison of efficacy of conbercept, aflibercept, and ranibizumab ophthalmic injection in the treatment of macular edema caused by retinal vein occlusion: a Metaanalysis
- Ocular manifestations and quality of life in patients after hematopoietic stem cell transplantation
