Subcutaneous pedicled propeller flap technique for microscopic reconstruction of eyelid defects
Lei Zhong, Qian-Yi Lu, Pei-Rong Lu
The First Affiliated Hospital of Soochow University, Suzhou 215006, Jiangsu Province, China
Abstract● AlM: To describe the subcutaneous pedicled propeller flap technique for the microscopic reconstruction of eyelid defects and evaluate its outcomes.
● KEYWORDS: propeller flap; eyelid defect; microscopic reconstruction
INTRODUCTION
The reconstruction of eyelid defects is challenging because of the complex anatomy and esthetic importance of the eyelid.The appearance and function of the eyelids are two important factors to be considered in ophthalmic plastic surgery.Skin flap transplantation is a commonly used method in eyelid plastic surgeries.Historically, flaps such as sliding flaps and kite flaps were widely used for eyelid repair.The propeller flap is a unique pedicled island flap[1].The outstanding advantages of propeller flaps are the use of the adjacent skin to replace “like”with “like,”the closest possible color and thickness match to the tissue of the defect area,and flexible transposition.The propeller flap, which was first described in 1991[2], is widely used in plastic surgery at other body sites, but is still rarely used for eyelid reconstruction.To the best of our knowledge, there have been no reports on the use of this technique to repair posterior-layer eyelid defects.This paper aims to report the application and outcomes of the propeller flap technique for the microscopic reconstruction of defects involving the anterior or posterior layer of the eyelid.
SUBJECTS AND METHODS
Ethical ApprovalThis study was carried out in strict accordance with the principles of the Declaration of Helsinki of the World Medical Congress, and the study protocol was reviewed and approved by the Ethics Review Committee of the First Affiliated Hospital of Soochow University (ID: 2022-139).All methods were carried out in accordance with relevant guidelines and regulations.Written informed consents and clinical photograph publication permissions were obtained from all patients.

Figure 1 Demonstration of the subcutaneous pedicled propeller flap technique for the microscopic reconstruction of a defect in the anterior layer of the eyelid A: Positioning and designing the flap shape; B: Rotation of the pedicled propeller flap; C: Transplanted flap in the defect area; D: Appearance immediately after microsuturing.
Patient SelectionWe retrospectively enrolled 23 patients with eyelid defects due to tumor excision who underwent one-stage microscopic reconstruction with the subcutaneous pedicled propeller flap technique in the Department of Ophthalmology of the First Affiliated Hospital of Soochow University, Suzhou,China, between February 2017 and December 2021.The inclusion criteria were as follows: 1) patients with eyelid defects due to tumor excision who underwent one-stage microscopic reconstruction with the subcutaneous pedicled propeller flap technique; 2) all operations were performed by the same surgeon; 3) patients provided informed consent for the surgery after their preoperative condition had been explained to them; and 4) patients were followed up as required.The exclusion criteria were as follows: 1) patients had other uncontrolled acute ocular diseases before the surgery; 2)patients with a tendency to develop hypertrophic scars; and 3)patients who did not attend their follow-up appointments.We recorded the following clinical data: age, gender, pathological tumor diagnosis, defect size, and follow-up duration.
Surgical TechniqueAll surgeries were performed under an ophthalmic operating microscope.The conjunctival sac of the surgical eye was topically anesthetized with 0.5% proparacaine hydrochloride ophthalmic solution.Local infiltrating anesthesia was induced (2% lidocaine with epinephrine at 1:200 000 dilution), and the eyelid tumor was excised.Tumors suspected to be malignant were excised using Mohs micrographic surgery and sent for rapid pathological characterization[3].Eyelid reconstruction was performed after confirmation of negative tumor margins.
For the microscopic reconstruction of defects involving the anterior layer of the eyelid, the subcutaneous pedicled propeller flap technique was performed using the following steps: 1) a donor site adjacent to the defect area was selected;2) the propeller flap was designed according to the length and width of the eyelid defect; 3) a pedicle was made for the propeller flap by using the adjacent subcutaneous orbicularis oculi muscle; 4) the subcutaneous pedicled propeller flap was rotated by 180° to cover the defect and sutured with 7-0 polypropylene sutures.The donor site was closed with 7-0 nylon sutures (Figure 1).
For the microscopic reconstruction of defects involving the posterior layer of the eyelid, the steps of the subcutaneous pedicled propeller flap technique were as follows: 1) a donor site adjacent to the tarsal defect was selected, 2) the propeller tarsal flap was designed according to the dimensions of the tarsal defect, 3) a pedicle was made for the propeller tarsal flap by using the adjacent subcutaneous orbicularis oculi muscle,and 4) the tarsal flap was rotated by 180° to cover the defect.The incisions were sutured with 6-0 absorbable thread.
Postoperative Care and Follow-up ExaminationsFor 48h after the operation, a cold compress was used to reduce edema.Levofloxacin eye drops were applied to the eye three times a day for usually two weeks.The dressing was changed daily until the sutures were removed 1wk after the surgery.Outpatient review and eyelid photography were performed at 1, 3, 6, and 12mo after the operation, followed by annual outpatient reviews thereafter.The follow-up data recorded included survival rate of the propeller flap; appearance,position, and function of the eyelid; and tumor recurrence rate.Patient satisfaction was also assessed.
RESULTS
Surgical OutcomesThis study included a total of 23 patients,consisting of 12 men and 11 women (Table 1).The mean age of the patients was 58.9y (range, 31-82y).The tumor diagnoses were as follows: basal cell carcinoma, 9 patients; nevus,5 patients; papilloma, 5 patients; xanthelasma, 2 patients;meibomian adenocarcinoma, 1 patient; and keratoacanthoma,1 patient.The eyelid defect was graded[4-5]as mild in 7 patients, moderate in 12 patients, and severe in 4 patients.The eyelid defect involved the anterior layer in 22 patients and the posterior layer in 1 patient.All operations were successfully completed in a single stage.
Follow-up ResultsAll 23 patients (23 eyes) completed the follow-up.The shortest follow-up duration was 3mo, and the longest was 60mo.All the propeller flaps survived well.Postoperative edema and bruising were mild.There was no significant difference in color and luster with the adjacent tissues, and there was no dog ear phenomenon.No obvious scarring was observed.There were no obvious abnormalities in eyelid morphology and function.No adverse complications such as eyelid insufficiency, exposure keratitis, entropion,ectropion, ptosis, and eyelid retraction were found.No tumor recurrence was found till the last follow-up examination.All patients were satisfied with the surgical results.
Case Presentation
Case 1A 79-year-old woman with basal cell carcinoma in the right lower eyelid was left with a 16 mm ×7 mm defect in the anterior layer of the eyelid after tumor excision.Single-stage microscopic reconstruction with the subcutaneous pedicled propeller flap technique was performed.The subcutaneous pedicled propeller flap healed well, with no tumor recurrence or abnormal eyelid morphology during 46mo of follow-up.The right eye looked even younger than the left eye after the reconstruction, and the patient was satisfied with the result(Figure 2).
Case 2A 56-year-old man presented with meibomian adenocarcinoma of the right eye.After tumor resection, the patient had a tarsal defect measuring 13 mm ×7 mm.The propeller pedicled flap technique was used to microscopically repair the defect in the posterior layer of the eyelid.The tarsal propeller flap survived well over 20mo of follow-up.There was no obvious abnormality in the morphological function of the eyelid, no foreign body discomfort on the eye surface, and no tumor recurrence.The patient was satisfied with the surgical result (Figure 3).
Case 3A 31-year-old woman presented with a nevus on the inner lower eyelid margin of the right eye.After tumor resection, the anterior eyelid defect measured 5 mm×5 mm.This young patient had high requirements for eyelid appearance.We considered that if a sliding skin flap were to be used for eyelid reconstruction, the local vertical tension would be high, and the dog ear phenomenon and local ectropion would be a possibility.We therefore preferred the pedicled propeller flap for this patient.The postoperative local tension was not obvious.The scar was slight, and there was no dog ear phenomenon, eyelid ectropion, or other deformities.The patient was satisfied with the surgical result (Figure 4).
DISCUSSION
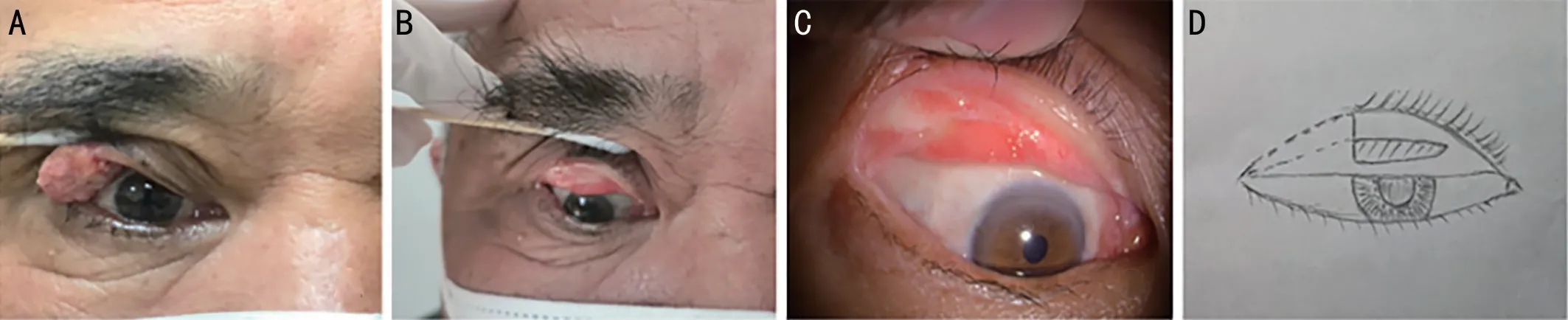
Figure 3 Microscopic reconstruction with the subcutaneous pedicled propeller flap technique for a defect in the posterior layer of the eyelid after the excision of a meibomian adenocarcinoma A: Preoperative photo.B: At 20mo after the operation, the tarsal surface is smooth and flat.The color of the tarsal plate in the transplanted area and the shape of the palpebral margin are good.C: Appearance of the eyelid under a slit-lamp microscope at 20mo after the surgery.D: Diagram showing the transposition of the propeller tarsal flap.A pedicled propeller flap was taken from the healthy tarsus near the fornix and transplanted into the temporal tarsal defect area by using 180° rotation and transposition.
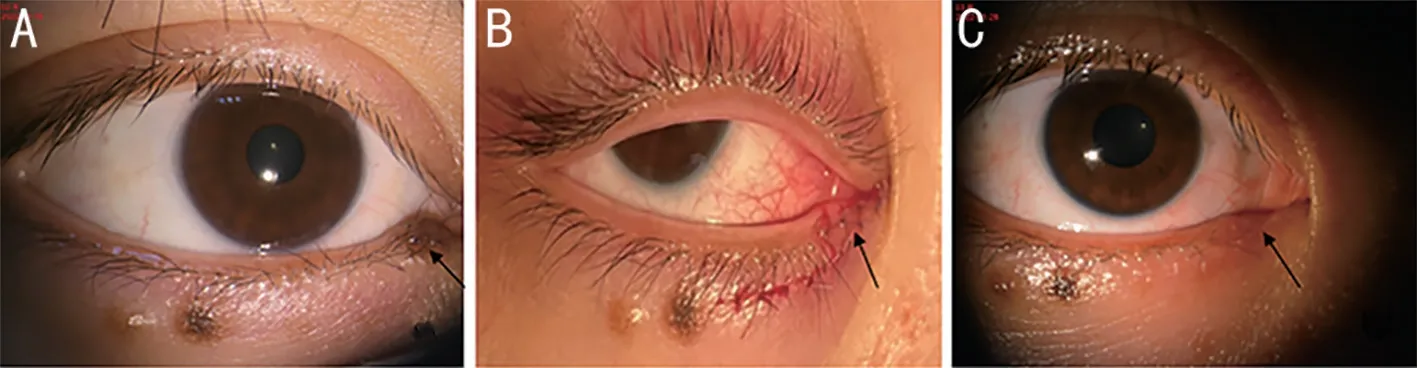
Figure 4 Microscopic reconstruction with the subcutaneous pedicled propeller flap technique for an inner eyelid defect after the removal of an intradermal nevus A: Preoperative photo.The black arrow shows the tumor on the inner lower eyelid margin of the right eye.B: The black arrow shows the propeller flap, which has been rotated and microsutured.C: Appearance at 3mo after the operation.The black arrow shows primary healing of the surgical site with slight scarring and good eyelid appearance.
Due to the special structure and function of the eyelid, the surgical reconstruction of eyelid defects is difficult and challenging for ophthalmologists.In most cases, autologous tissue transplantation should be performed to try to achieve the dual effects of functional and morphological reconstruction.While there is no one perfect reconstruction method that works for all patients, local flaps, such as sliding flaps, rotated flaps, and kite flaps, are widely used for eyelid reconstruction in clinical practice[6-9].The subcutaneous pedicled propeller flap differs from the above-mentioned flaps in that it offers the following advantages: 1) As the pedicle consists of the subcutaneous orbicularis muscle, the rotation is more flexible than skin pedicle flaps and without distortion at the base of the flap.2) Using adjacent tissues to create the flap ensures the closest possible match between the flap tissue and the defect tissue in terms of structure, color, and texture.3) The abundant blood circulation of the eyelid provides favorable surroundings for the survival of the propeller flap[10].This is particularly advantageous in the periocular area where there is a shortage of tarsal tissue in the vertical direction, but abundant tarsal tissue is present in nearby areas such as the nasal or temporal area[11].However, attention should be paid to the positioning,size, and shape of the flap during the design stage[12].
For the conventional repair of posterior eyelid defects,available options for restorative materials include palatal mucosa[13], autologous labial mucosa[14], allogeneic sclera[15],and conjunctival flap with auricular cartilage grafting[16].The use of the palatal mucosal graft for upper eyelid reconstruction is controversial because the hard palate mucosa is composed of keratinized, stratified squamous epithelium, which can irritate the ocular surface[13].Allogeneic sclera and acellular dermal grafts carry the risk of infection and rejection.Auricular cartilage is a good material for the autogenous replacement of tarsal tissue[16].However, auricular cartilage cannot be exposed to the ocular surface, and a conjunctival flap should be made to cover the auricular cartilage to protect the ocular surface.The surgical procedure is relatively complicated, and is suitable for patients with severe eyelid defects.In patients with mild-to-moderate defects in the posterior layer of the eyelid, especially when the tarsal tissue is insufficient in the vertical direction but is abundant on the nasal or temporal side, our subcutaneous propeller tarsal flap is the best choice,as it offers the advantages of nearby material, convenience,flexibility, and high survival rate.One of the patients in this study had a moderate defect in the posterior layer of the eyelid after meibomian adenocarcinoma resection.The lateral defect in the upper tarsal plate exceeded 1/3 of the total tarsus length after the excision of the meibomian tumor.We designed a subcutaneous propeller tarsal flap pedicled with the orbicularis muscle from the normal tarsus on the nasal side (donor site)and rotated the flap along its pedicle to repair the temporal tarsal defect area.The tarsal flap healed well.Over 20mo of follow-up, the tarsal surface in the surgical area was smooth;the eyelid appearance and function showed no obvious abnormality, and there was no tumor recurrence.The feasibility of using the propeller flap technique to repair and reconstruct posterior-layer defects of the eyelid was well demonstrated in this case.The subcutaneous pedicled propeller flap technique is more complicated for eyelid defects in the posterior layer than for defects in the anterior layer.During the operation,the upper edge of the tissue flap should be sutured and fixed with the elevator aponeurosis to preserve the function of upper eyelid lifting, and the knots should be buried between the tissue layers to keep the smoothness of the tarsal surface.At the end of the operation, tarsorrhaphy was performed, and the eyelid adhesion was maintained for 3mo.The purpose of tarsorrhaphy was to inhibit the formation of propeller tarsal flap scar contracture and maintain a normal position of the eyelid[16].
Aesthetic and functional outcomes can have a profound effect on people's self-esteem and confidence, or help them to return to a normal life.Therefore, eyelid defects should be repaired with thoughtful planning and expertise[17].There is no one perfect reconstruction method that works for all,and each method has its advantages and disadvantages.The key to a successful reconstruction includes a thorough understanding of the patient's condition, a proper assessment of the extent and location of the defect, and individualized selection of the optimal reconstruction method.Avoiding tension, addressing laxity, and eyelid esthetics should all be taken into consideration.In addition, adequate preoperative communication and risk notification; attention to postoperative care such as clean dressing changes, early compression dressing, adequate immobilization, and local ice compress; and regular follow-up examinations are very important for the final outcome.
Patients' expectations of the outcomes of reconstructive surgery are continually increasing.Recently, the techniques of ophthalmic plastic surgery have been trending towards the precise and meticulous.The advantages of microscopy-assisted blepharoplasty have been reported previously[18-20].Meticulous operation and minimization of iatrogenic injury are important factors for the success of the operation[21].Reconstruction of the eyelid defect must be meticulous.All the operations in this study were performed under an ophthalmic operating microscope.Compared with conventional ophthalmic plastic surgery under direct vision, surgery under a microscope has obvious advantages in terms of the clarity of the visual field,the convenience of lighting regulation, the precision and meticulousness of the operation, and the surgeon's comfort.Furthermore, in our study, the postoperative scars were mild, and the patients expressed a great deal of comfort and satisfaction after the microscopic operation.
In conclusion, the subcutaneous pedicled propeller flap technique for the microscopic reconstruction of eyelid defects is easy to perform and has satisfactory outcomes in terms of eyelid function and esthetics.This technique merits clinical application, and is expected to serve as a new method of tissue flap transplantation for blepharoplasty.However, the performance of this technique in the repair of posterior-layer eyelid defects needs to be confirmed in more patients.
ACKNOWLEDGEMENTS
Authors’contributions:Zhong L was a major contributor in surgery, data collection, article design, analysis, and writing.Lu PR was a major contributor in article design, critical review and guidance support.Lu QY was a major contributor in data collection, article writing and work support guidance.All authors read and approved the final manuscript.
Foundation:Supported by theYoung Talent Program of Gusu Health Project (No.GSWS2020014).
Conflicts of Interest: Zhong L,None;Lu QY,None;Lu PR,None.
 International Journal of Ophthalmology2023年7期
International Journal of Ophthalmology2023年7期
- International Journal of Ophthalmology的其它文章
- Chickenpox followed streaky multifocal choroiditis with prednison treatment in a girl with asthma
- Pneumonia and ocular disease as the primary presentations of Takayasu arteritis: a case report
- Unilateral blurred vision in pediatric patient associated with cavum velum interpositum cyst
- Highly cited publication performance in the ophthalmology category in the Web of Science database:a bibliometric analysis
- Comparison of efficacy of conbercept, aflibercept, and ranibizumab ophthalmic injection in the treatment of macular edema caused by retinal vein occlusion: a Metaanalysis
- Ocular manifestations and quality of life in patients after hematopoietic stem cell transplantation
