Pathologic etiology and predictors of malignancy in children with cervical lymphadenopathy
Jee Woo Kim·Jee Yeon Baek·Ji Young Lee·Sung Min Lim·Ji-Man Kang·Won Kee Ahn·Seung Min Hahn·Jung Woo Han·Chuhl Joo Lyu·Jong Gyun Ahn
Cervical lymphadenopathy in children is a common disease entity that is accompanied by a variety of processes,ranging from benign disease to malignancy.Although the cause of cervical lymphadenopathy in children is often benign [1—4],the presence of enlarged lymph nodes can cause anxiety to parents because of its association with malignancy.Biopsy should be considered for the histologic diagnosis of persistent or unexplained cervical lymphadenopathy in children.However,biopsy is an invasive examination method,and it is difficult to clinically determine whether biopsy is needed in children with unexplained cervical lymphadenopathy.Therefore,clinicians should be aware of the differential diagnosis of lymph node enlargement in children and should identify situations in which malignancy may be suspected.In this study,we aimed to identify the etiology of pediatric cervical lymphadenopathy using biopsy and to analyze the risk factors associated with malignancy in children with cervical lymphadenopathy.
We retrospectively reviewed the medical records of children aged ≤ 18 years who had undergone excisional and fine needle aspiration biopsies at Severance Children’s Hospital in Korea between November 2005 and December 2019.All cases were identified using prescription codes,including those of lymph node biopsies.We excluded cases in which a lymph node biopsy was performed for a secondary purpose,such as the determination of metastasis or the surgical removal of other tissues (e.g.,thyroidectomy or parotidectomy) in patients with other underlying diseases.
To identify significant differences between the benign and malignant groups,univariate logistic regression analysis was used.Multivariable logistic regression analysis was performed to identify significant risk factors for the malignant group.Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated via univariate and multivariable logistic regression analyses.To compare the ability of laboratory findings and multivariable models to predict malignancy,receiver operating characteristic (ROC) curves were analyzed by estimating the area under the curve (AUC).
During the 14-year study period,113 cases were included in this study.The median age at biopsy was 14.0 years(interquartile range [IQR],8.0—17.0 years),and the female-to-male ratio was 1:1.1.The results of the histopathological analyses are summarized in Fig. 1.Of the 113 cases,87 (77.0%) were assigned to the benign group and 26 (23.0%) in the malignant group,respectively.In the benign group,the most common histopathological etiology was Kikuchi—Fujimoto disease (41.6%),followed by reactive hyperplasia (23.9%).In the malignant group,the most common histopathological etiology was lymphoma (16.8%),followed by Langerhans cell histiocytosis(2.7%).
Comparisons made between the benign and malignant groups are summarized in Table 1.Univariate logistic regression analysis revealed that the median age at biopsy and erythrocyte sedimentation rate (ESR) were lower in the malignant group than that in the benign group.However,the lymph node size was larger,and the white blood cell (WBC) count,platelet count,and absolute neutrophil count (ANC) were higher in the malignant group than in the benign group.Moreover,the multivariable logistic regression analysis identified increased lymph node size (OR:1.084;95%CI=1.015—1.158;P=0.017) and decreased ESR(OR: 0.956;95%CI=0.920—0.993;P=0.021) as signif icant risk factors for malignancy.
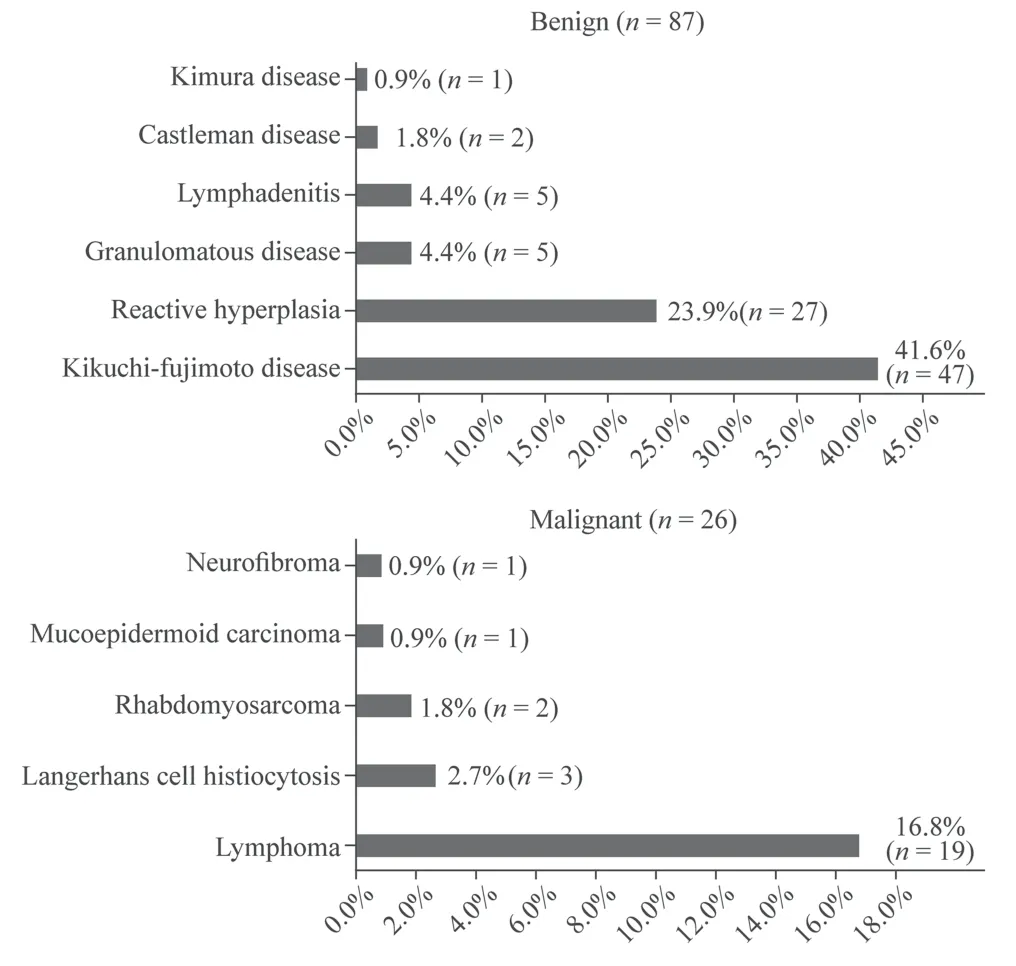
Fig.1 Results of histopathological diagnosis

Table 1 Patient characteristics and clinical symptoms,lymph node characteristics,and laboratory f indings in the two groups
We calculated the optimal cutoff values of lymph node size and ESR for differentiating the malignant group from the benign group by drawing ROC curves (Fig. 2 a).The AUC was 0.752 (95%CI=0.634—0.871;P<0.001) for cervical lymph node size and 0.684 (95%CI=0.504—0.863;P=0.034) for ESR.We also drew an ROC curve using cervical lymph node size and ESR together as a combined risk factor for malignancy.The AUC of cervical lymph node size and ESR was 0.852 (95%CI=0.751—0.953;P<0.001).The cutoff value of lymph node size to predict malignancy was 26 mm,with a sensitivity of 76.9%,specificity 67.4%,negative predictive value 90.6%,and positive predictive value 41.7%.The cutoff value of ESR was 7 mm/hour with a sensitivity of 42.9%,specificity 94.7%,negative predictive value 87.1%,and positive predictive value 66.7%.Based on the results of ROC analysis,we drew a scatterplot of cervical lymph node size and ESR (Fig. 2 b).As shown in the scatterplot of the linear decision boundary that separates benign disease and malignancy,cervical lymph node size and ESR are significant risk factors for malignancy.
In children with cervical lymphadenopathy,biopsy is usually performed when there is a high suspicion of malignancy[5].Nevertheless,in our study,77% of all children who had undergone cervical lymph node biopsy had benign disease.Other studies that analyzed the cause of pediatric cervical lymphadenopathy in patients who had undergone biopsy also reported more benign than malignant lesions [6—10].Among malignancies,lymphoma is one of the most common causes and is among the top three common causes in all studies.
Therefore,it is necessary to identify the risk factors predicting malignancy in cases of pediatric cervical lymphadenopathy.The etiology of pediatric cervical lymphadenopathy differs from country to country.In our study,Kikuchi—Fujimoto disease was the most common cause,whereas tuberculosis was the most common cause in Nigeria and Pakistan [6—8].In studies from Italy and India,reactive lymphadenitis was the most common cause [9,10].This suggests that epidemiological situations may vary depending on differences in infection or other environmental factors in each country,and clinicians should be aware of the epidemiological situations by studying the common causes of the disease in each country.The cause of Kikuchi—Fujimoto disease is not yet known.Interestingly,Kikuchi—Fujimoto disease accounted for 41.6% of cases with cervical lymphadenopathy in this study but was less common in other studies,suggesting that there may be ethnic differences in outbreaks.
In this study,the main risk factors predicting malignancy in children with cervical lymphadenopathy were the size of the lymph nodes and low ESR.Our finding of an association between cervical lymph node size and malignancy is consistent with the results of previous studies.Fatih Celenk et al.[11] reported larger lymph node size and left-sided lymphadenopathy as significant predictors of malignancy in children.Tsai et al. [12] demonstrated that larger lymph node size,more advanced age,supraclavicular location,tumor fixation,tenderness,and larger tumor size were significant predictors of malignancy in 166 patients with neck masses.However,the cutoff value of the cervical lymph node size that can predict malignancy in children has not previously been determined.Our study found this cutoff value to be 26 mm.In general,biopsy is recommended when cervical lymph nodes greater than 2 cm are persistently palpable in children [13].Our results provide evidence to support this recommendation.Therefore,clinicians should carefully note the lymph node size during physical examination.
In our study,a low ESR was a laboratory risk factor predicting malignancy in children with cervical lymphadenopathy.However,the results of some previous studies are not consistent with our findings.Şen et al. [14] reported that the presence of anemia,leukocytosis,thrombocytosis,and elevated ESR were related to the risk of malignancy in cervical lymphadenopathy.Oguz et al. [15] reported that the risk factors associated with malignancy of peripheral lymphadenopathy were anemia,leukocytosis,and elevated ESR,C-reactive protein (CRP),and lactate dehydrogenase (LDH).However,in this study,CRP,LDH,and WBC count were not found to be significant predictors of malignancy.Although ESR was previously thought to be elevated in cases of malignancy,our results indicated that a lower ESR is a meaningful risk factor for malignancy.The cutoff value for ESR was 7.0 mm/hour,but the sensitivity was 42.9%,which makes it difficult to use it in clinical situations.However,unlikein previously known cases,ESR can be normal in cervical malignancy in children.Moreover,a study demonstrated that the prevalence of malignancy in patients with elevated ESR is low and that the elevation of ESR is not a sign of malignant disease [16].Therefore,even if ESR is normal in children with cervical lymphadenopathy,clinicians must check for malignancy through a biopsy.
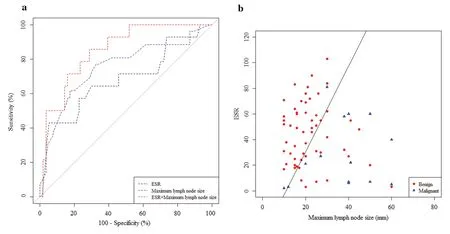
Fig.2 Risk factors for malignancy in children with cervical lymphadenopathy. a Receiver operating characteristic curves for lymph node (LN) size and erythrocyte sedimentation rate (ESR) for the prediction of malignancy.The area under the curve was 0.752 (95% CI=0.634—0.871; P<0.001)for cervical lymph node size,0.684 (95% CI =0.504—0.863; P =0.034)for ESR,and 0.852 (95% CI =0.751—0.953; P < 0.001) for cervical lymph node size and ESR together; b Scatterplot of cervical lymph node size and ESR showing the results of the benign and malignant groups
This study had some limitations.First,since it was conducted at a single tertiary hospital,it is not representative of all cases of pediatric cervical lymphadenopathy in South Korea.Second,excisional biopsy was performed only on patients in whom malignancy was suspected,which could have resulted in a selection bias.
In conclusion,our study showed that in children with cervical lymphadenopathy who had undergone biopsy,there were more benign than malignant lesions,and the three most common etiologies were Kikuchi—Fujimoto disease,reactive hyperplasia,and lymphoma.A large lymph node size and a low ESR were significant predictive factors of malignancy.However,patient symptoms showed no significant difference between the benign and malignant groups.Further studies including a larger number of patients may show more significant results.
AcknowledgementsWe thank all the patients and their parents for their kind cooperation.We thank all the medical staff who provided care for patients.
Author contributionsJWK contributed to obtaining institutional approval,acquisition and analysis of data,and drafting and revising the manuscript.JMK assisted in data analysis and drafted and revised the manuscript.JYB,JYL,SML,WKA,SMH,JWH,and CJL carried out the analysis and interpretation of the data,and reviewed and revised the manuscript.JGA conceptualized and designed the study,coordinated and supervised data collection,and drafted and revised the manuscript.All authors read and approved the manuscript.
FundingNo funding was received for this study.
Data availabilityAll data generated during and/or analyzed during this study are available from the corresponding author on reasonable request.
Declarations
Conflict of interestAll authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approvalThis study was approved by the Institutional Review Board of Severance Hospital (IRB number: 2022—0803-011),and the requirement of obtaining informed consent was waived because of the retrospective nature of the study.The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
 World Journal of Pediatrics2023年3期
World Journal of Pediatrics2023年3期
- World Journal of Pediatrics的其它文章
- Monkeypox and the perinatal period: what does maternal–fetal medicine need to know?
- Monkeypox virus: past and present
- Stressful life events,psychosocial health and general health in preschool children before age 4
- Number and distribution of eosinophils and lymphocytes in the Japanese pediatric gastrointestinal tract: in search of a def inition for “abnormally increased eosinophils”
- Associations of preterm and early-term birth with suspected developmental coordination disorder: a national retrospective cohort study in children aged 3–10 years
- T-cell and B-cell repertoire diversity are selectively skewed in children with idiopathic nephrotic syndrome revealed by high-throughput sequencing
