Comparison of ocular trauma between normalized and the COVID-19 epidemic periods in China: a multi-center cross-sectional study
Ya-Xin Zhang, Kang Feng, Meng-Yu Liao, Hua Yan,3
1Department of Ophthalmology, Tianjin Medical University General Hospital, Tianjin 300052, China
2Department of Ophthalmology, Peking University Third Hospital, Beijing 100191, China
3Tianjin Medical University, Tianjin 300070, China
Abstract
● KEYWORDS: ocular trauma; non-mechanical eye injuries; incidence; COVID-19; epidemiology
INTRODUCTION
In December 2019, a novel Coronavirus (severe acute respiratory syndrome Coronavirus 2) rapidly spread in China and around the world[1‐2]. The disease was first described in late December of 2019 as viral pneumonia based on reports from Wuhan, China. It was named COVID‐19 that arousing a new worldwide pandemic subsequently[3‐4]. In response to the COVID‐19 outbreak, the Chinese government launched nationwide measurements to prevent the spreading of infection at the end of January 2020. After a long time of practice, the epidemic in China has been brought under control. However,due to the COVID‐19 specific properties and strong infective,China had undergone a period of epidemic lockdown management in 2020 and entered a special anti‐epidemic period following the lockdown.
Previous publication has shown that the frequency and nature of accidents leading to severe ocular trauma have been affected by the on‐going pandemic[5‐6]. In some areas, the number of eye injuries has increased dramatically because of the pandemic[7]. While, some studies also put forward the opposite point of view, such as road accident injuries, geriatric trauma,etc. have decreased significantly[8]. At the same time, due to the forced intervention of government departments which changed the of life of some people, the occurrence characteristics of eye trauma are also very different from those in the past[9].This makes it particularly important to obtain the domestic characteristics of ocular trauma under the epidemic period.
In the study, we compared the characteristics of hospitalized patients with ocular trauma in China in 2019 (normalized period) and 2020 (COVID‐19 epidemic period) to explore the impact of the public health emergency on the incidence of eye injuries in China, which will provide a profile and referable evidence for prevention and control eye injuries in special times in future.
SUBJECTS AND METHODS
Ethical Approval The study conformed to the Declaration of Helsinki and was approved by the Review Board/Ethics Committee of Tianjin Medical University.
A multi‐center cross‐sectional study was performed to identify the impact of COVID‐19 on the presentation of ocular trauma. All patients who presented to the Ophthalmology Department and admitted to the hospital from 30 hospitals in 2019 (from 1stJanuary to 31stDecember) and 2020 (from 1stJanuary to 31stDecember) were included in the study, which had been described in previous publication[10]. Those victims with less damaged, who did not require being hospitalized,were excluded. The outbreak in China began in December 2019, while China did not under the “lockdown period” for preventing the epidemic, so it can be considered that January 1stto December 31st, 2019, is a non‐epidemic “normalized”stage. From January 1stto December 31st, 2020, China under the “lockdown stage” and a special anti‐epidemic period for preventing and controlling the COVID‐19 epidemic. Therefore,the year of 2020 was considered as “COVID‐19 epidemic period”.According to the geographical characteristics of China, we divided the area into seven geographical regions. Namely,North China (including Beijing, Tianjin, Hebei, Shanxi, and Inner Mongolia Autonomous Region); East China (including Shanghai, Jiangsu, Zhejiang, Anhui, Fujian, Jiangxi,Shandong, and Taiwan); South China (including Guangdong,Guangxi Autonomous Region, Hainan, Hong Kong Special Administrative Region, and Macau Special Administrative Region); Central China (including Henan, Hubei, and Hunan);Southwest China (including Chongqing, Sichuan, Guizhou,Yunnan, and Tibet Autonomous Region); Northwest China(including Shaanxi, Gansu, Qinghai, Ningxia Autonomous Region, and Xinjiang Autonomous Region); Northeast China(including Liaoning, Jilin, and Heilongjiang). Inner Mongolia Autonomous Region was included in Northwest China in the study, for most of the patients of the Affiliated Hospital of Inner Mongolia Medical University are coming from the west of Inner Mongolia.
In the study, we selected comprehensive tertiary A hospitals or eye specialist hospitals from 22 cities covering 20 provinces,municipality, and autonomous regions in China as the target hospitals that were listed after the article. Demographic and injured information of all cases were collected based on the hospitalized records and were input into the electronic version of the Excel data frame. Subsequently, the research group summarized the collected data from the participated hospitals.Special personnel from the research team mark the missing and incorrect data information and then contact the registrars to retrieve the original case data. If the original medical records are not detailed, the registrars contacted patients by telephone to supplement the information.
Statistical AnalysisThe statistical level of significance was preset at 0.05, and all the eligible data were analyzed using SPSS version 26.0 statistical software (SPSS Inc, Chicago,Illinois, USA), data collation and Figures were implemented using Excel (2016 version, Microsoft, Redmond, USA).
RESULTS
Totally 13 525 (7269 cases in 2019, 6256 cases in 2020)injured cases from 30 participated hospitals were included in this study. There were 11 129 (82.28%) male and 2396(17.72%) female in them whose average age is 40.58 (SD 19.22) years old (0‐94y).
In terms of geographical distribution, the cases of eye trauma in 2019 are mainly concentrated in Central region of China(26.04%,n=1893), East of China (23.76%,n=1727), and North of China (23.74%,n=1726), followed by Southwest of China (14.18%,n=1031), Northwest of China (7.90%,n=574),Northeast of China (2.15%,n=156), and South of China(2.23%,n=162). In 2020, the overall distribution is similar, but the distribution has changed. The number of cases in Northern(30.05%,n=1880) and Northwestern (10.01%,n=626) regions separately increased 8.92% (year‐on‐year) and 9.06% (year‐on‐year) while the other areas appear different degree of decline.The number of cases in the Northeast, East and Central decreased significantly, separately decreased 64.74%, 30.57%,and 24.46% (year‐on‐year; Table 1).
In 2019, farmers (37.75%,n=2744), workers (17.97%,n=1306) and individual (10.14%,n=737) accounted for the main injured patients, while other occupations accounted for a less proportion (Table 2).
The same distribution continued in 2020, number of eye trauma cases declined in all occupations especially in college/postgraduate and staff members which went down year‐on‐year 65.88% and 31.64% separately. Number of eye trauma in retirees, housewives and unemployed rose year‐on‐year 4.96%, 102.67% and 11.64% respectively (Table 2). In 2019,40.39% (2936/7269) injured cases were woke‐related injuries but the number had dropped to 36.32% (2272/6256; Pearson Chi2=23.56,P<0.001) in 2020.The proportion of eye injuries occurred at home increased to 28.53% (n=1785) in 2020, while that is 18.85% (n=1370) in 2019 and remains the highest of all known sites of injury. Data on eye injuries at other sites are presented in Table 3.
Most ocular trauma cases in 2019 are rupture (23.36%,n=1698), penetrating (28.60%,n=2079), contusion (15.82%,n=1150) and the similar happened in 2020 (rupture 23.16%,n=1449; penetrating 30.18%,n=1888; contusion 12.80%,n=801; Table 4). However, proportion of penetrating injuries showed an increasing trend during the epidemic (2020), while that of rupture and contusion decreased compared with the past(2019).
The incidence of mechanical eye injuries decreased in 2020,while that of non‐mechanical eye injuries (chemical/thermal/radiation) increase of 47.45% year‐on‐year. There were 255(3.51%, 255/7269) and 376 (6.01%, 376/6256) non‐mechanical injured cases in 2019 and 2020 (Pearson Chi2=47.33,P<0.001)separately (Table 4).
DISCUSSION
Since cases of COVID‐19 were detected in December 2019,the COVID‐19 epidemic has rapidly swept across countries around the world (https://covid19.who.int). To reduce the spread of the novel coronavirus, countries have promoted a range of unprecedented public health responses all over the world. These measures aim at reducing the speed and area of epidemic to decrease the acute pressure on the healthcare system[2]. Governments have restricted public life during the COVID‐19 pandemic, inter alia closing social places such as sports facilities and gyms, pubs and restaurants[1], which drastically reduced the amount of industrial and daily activities.For example, Americans were required to stay at home except to perform essential functions[4,11]. In Italy, the government ordered people to stay home, restricting movements with the exception of work, urgent matters and health reasons[12].Even after lockdown orders were lifted, many businesses,including gyms, remained closed due to social distancing requirements[1,13].
China has taken the most comprehensive, rigorous, and thorough prevention and control measures since the beginning of the epidemic. A complete lockdown was imposed by the government in 2020 and continued for more than two months and entered a special anti‐epidemic period following the lockdown. People spent most of their time at home, and even when buying necessities, they were confined to restricted areas. Therefore, there was a series of significant changes in residents’ work and daily living behavior in China in 2020.Thus, it is likely that the COVID‐19 affect the incidence and characteristics of ocular trauma in China. Severe ocular trauma, while rare, carries a risk of significant morbidity to the patient[14‐15]. Common reasons of injury are falls, allegedassaults, sporting injuries, and industrial accidents[16]. While prognosis is usually poor, the factor in determining the outcome is various such as the time elapsed between injury and primary repair[17]. Therefore, great attention should be paid to the characteristics of ocular trauma under COVID‐19 epidemic period in China for future prevention, control, and clinical treatment during serious public events in future.
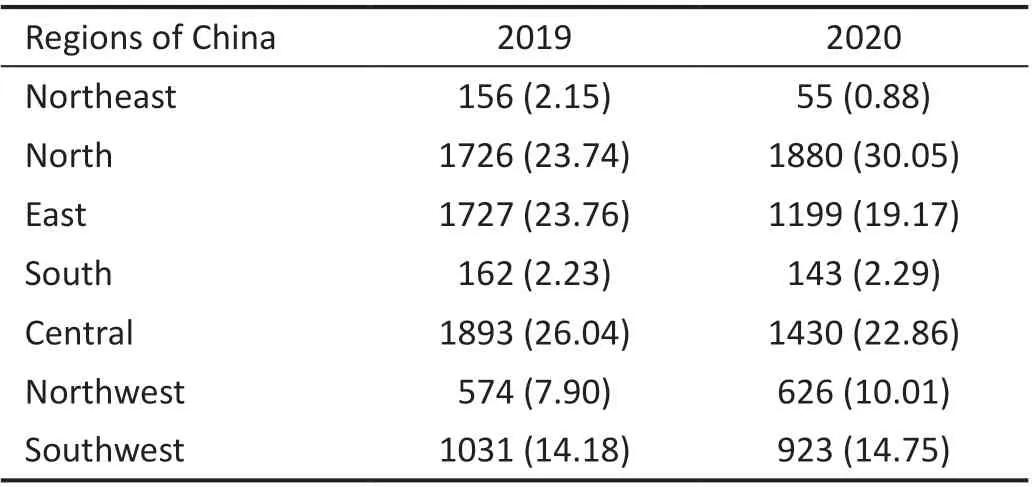
Table 1 The regions in China of injured cases in the study n (%)
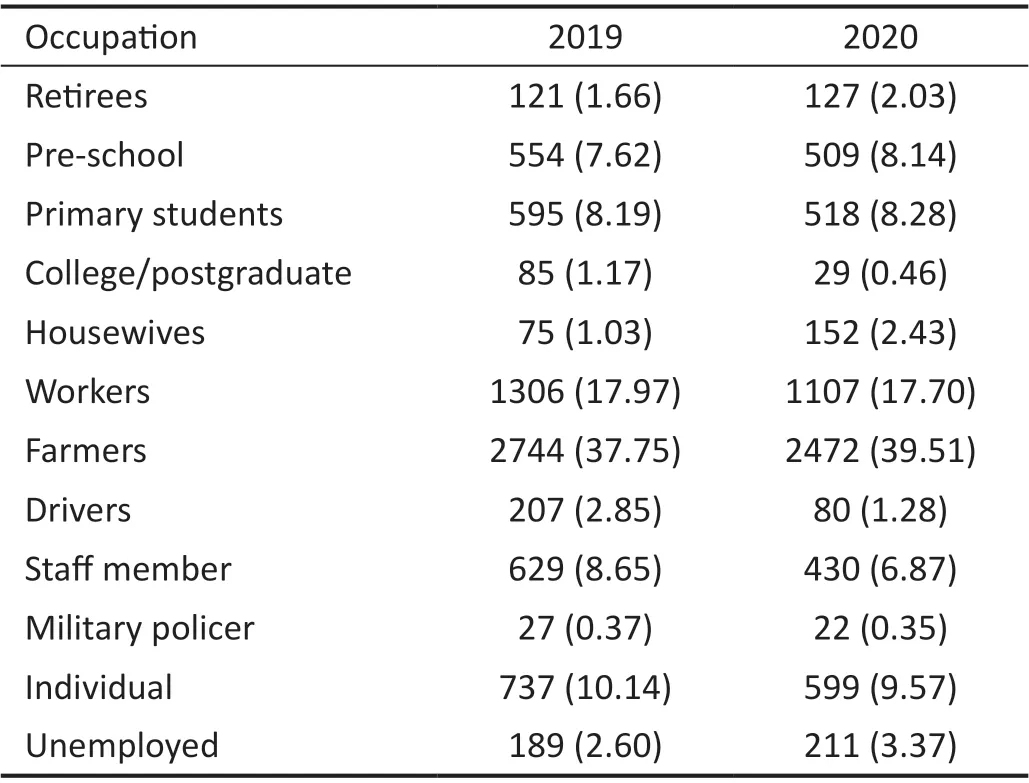
Table 2 The occupation distribution of injured cases in the study n (%)
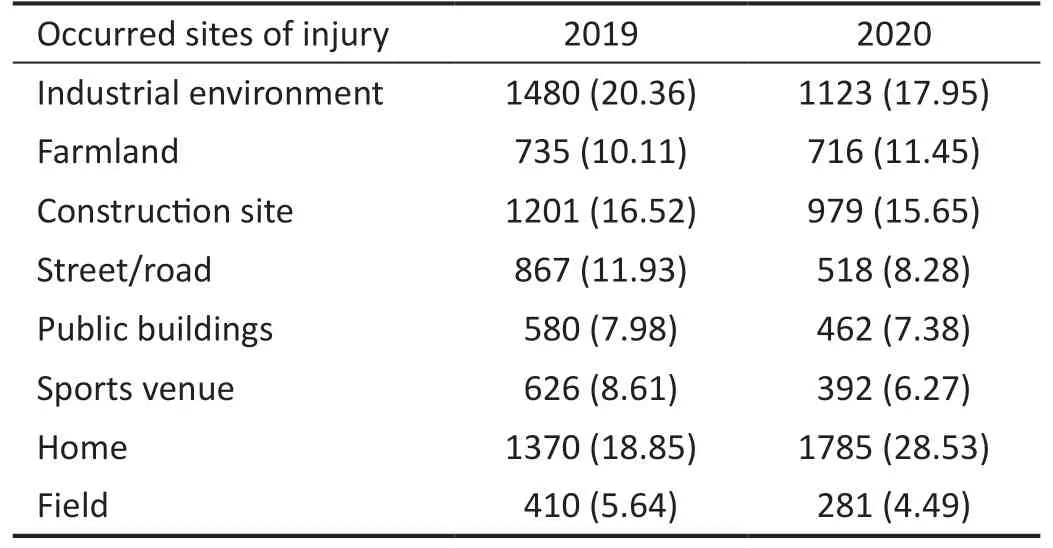
Table 3 The occurred sites of injury for cases in the study n (%)
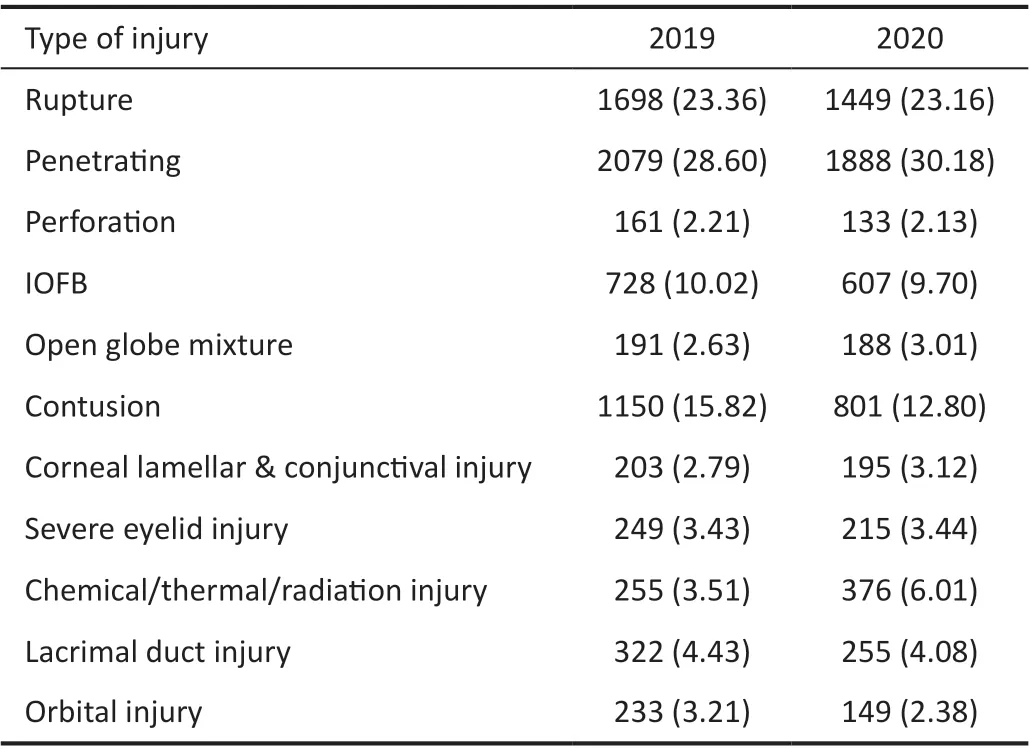
Table 4 The number of cases in different types of eye injuries in the study n (%)
Ocular trauma is an ophthalmological emergency, an important cause of blindness in one eye, and a huge social and economic burden[18‐19]. During the COVID‐19 epidemic period in 2020 in China, the number of severe ocular trauma cases was less than that in 2019. This result is consistent with the results observed in some other countries, mainly due to the reduction in traffic accidents, workplace accidents, and mechanical injury accidents during the epidemic[20‐21]. Pellegriniet al[12]studied the trends of ocular trauma during the pandemic in Italy, they found a striking 68.4% decrease in the number of eye injuries seen compared to the same period of the previous year. China has a vast territory, and different geographical regions show different characteristics of occurrence of ocular trauma. The number of eye trauma dropped significantly in Northeast, East, Southwest, and Central regions of China after the COVID‐19, while the number of cases increased in North and Northwestern regions of China (Table 1). It may be due to the government’s restrictions on population mobility,which resulted in the decline of the migrant population in developed cities, especially in East and Southeast regions.Northwest China is an inland area, so it is also the area that less affected by the epidemic. On the contrary, the tertiary class A comprehensive hospitals in Beijing, which belong to North of China, receive many complex eye injury cases from all over the country at any time.
When considering the influence of the occupation for ocular trauma, retirees and housewives are increased significantly(Table 2), for the reason that the prolonged indoor activities increase the risk of indoor eye trauma. Increased violence between intimate partners has also led to more eye injuries than ever before due to more time being confined at home[22‐23],and it is often women who were harmed in this process. In addition, many domestic services have been suspended due to the epidemic, leaving housewives to “do it themselves” that include some dangerous tasks such as changing light bulbs,dry cleaning clothes, replace fluorine in the air conditioner,and so on. At the same time, the proportion of work‐related injured cases in 2020 (36.32%, 2272/6256) is lower than that in 2019 (40.39%, 2936/7269), and there is statistically significant between them (Pearson Chi2=23.56,P<0.001),which confirmed that many people forced to stay at home and stop working under the epidemic, there is no doubt that this percentage will drop. What’s more, the rate of injuries among unemployed people has increased, maybe due to the sharp rise in unemployment during the pandemic. The clearly declined incidence of eye injuries in workers, farmers, and drivers(Table 2) due to closed factories and reduced outdoor work following the COVID‐19 outbreak. This can be verified in the results of the injured sites (Table 3).
Other researchers noted that patients with ocular trauma were more likely to have injuries at home and “do‐it‐yourself”or exercise during the COVID‐19 pandemic[24‐26], those are consistent with the results observed in this study. Corresponds to the previous result, the home injury was the highest among all kinds of injury sites, proportion of injury sites of “home”increased sharply in 2020 compared with 2019, which is the most noteworthy point for us. Under the COVID‐19 epidemic situation, the home has become the site of a high incidence of eye injuries, which noted us that home protection is also important in future especially during major public health events like the COVID‐19. Wearing protective goggles is essential to prevent eye injuries from household activities such as gardening, DIY activities and exercise, but the measure usually overlooked by populance[26‐27]. The long‐term limitation of activities during the epidemic made the people,especially young, lack sufficient self‐regulation ability[28‐29].Therefore, people are easily agitated due to the quarantine,which increases the possibility of a quarrel or even fight, so how to relieve psychological pressure during special period is worthy of exploration. In addition, more laboratory work has led to an increase in chemical injuries during lockdown from our study, which is the result of quarantine too. During the epidemic period, many students cannot leave school and experimental work became the first choice of many students,so laboratory safety education is particularly important. Lack of safety awareness will lead to a greater risk of injuries, such as sulfuric acid corrosion and gas explosion. Those results can be reflected through the composition ratio of the types of injury(Table 4) in the study.
Rupture, penetrating, and contusion are still the main types of injuries, which is consistent with the situation before the outbreak, so prevention measures for these types cannot be ignored. The proportion of open ocular trauma dropped by nearly one‐eighth, mainly due to a decrease in ruptures,penetrating injuries, and intraocular foreign body. Among them, the proportion of rupture and penetrating injury is still the highest, which consistence with some other foreign studies[30‐31]. However, the non‐mechanical ocular trauma,mainly the chemical injury, increased obviously. In this study,there were 255 (3.50%, 255/7269) and 376 (6.01%, 376/6256)non‐mechanical injured cases in 2019 and 2020 (Pearson Chi2=47.33,P<0.001) separately. The increase was closely related to prolonged indoor activity during the outbreak, such as the aforementioned laboratory‐occurring trauma. We should pay more attention to the non‐mechanical eye injuries during public events in future.
The main limitation of this study is that it is a cross‐sectional study based on hospitalized cases. The hospitals included in the study are distributed in various geographic regions in China.In China, eye trauma surgery cannot be carried out in some grassroots hospitals, and is generally sent to a higher‐level medical unit, and the patients tend to choose a comprehensive tertiary A hospitals or specialist eye hospitals for treatment.
The COVID‐19 pandemic will continue and recur for a long time in the future[2,13], it will change the medical mode, and the prevention and treatment mode of ocular trauma during public events periods in future[32‐34]. Effective measures should be carried out during the COVID‐19 epidemic and other public events. The findings of this study suggest that under the epidemic periods, the retirees and housewives should be paid more attention. Protective measures for indoor activities should not be ignored, especially when performing some high‐risk home activities. Moreover, more prevention and control measures should be focused on the non‐mechanical injuries during serious public events period in future.
ACKNOWLEDGEMENTS
Authors’ contributions: Zhang YX, Feng K, and Yan H had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Feng K. Acquisition, analysis,or interpretation of data: Zhang YX, Feng K. Drafting of the manuscript: Zhang YX. Critical revision of the manuscript for important intellectual content: Yan H. Statistical analysis:Feng K. Obtained funding: Yan H. Material support: Liao MY.Supervision: Yan H.
Foundations:Supported by National Natural Science Foundation of China (No.82020108007; No.81830026);Beijing‐Tianjin‐Hebei Special Project (No.20JCZXJC00180).
Conflicts of Interest:Zhang YX,None;Feng K,None;Liao MY,None;Yan H,None.
 International Journal of Ophthalmology2023年1期
International Journal of Ophthalmology2023年1期
- International Journal of Ophthalmology的其它文章
- Visual perception alterations in COVID-19: a preliminary study
- COVID-19 pandemic impact on ocular trauma in a tertiary hospital
- Apolipoprotein A1 suppresses the hypoxia-induced angiogenesis of human retinal endothelial cells by targeting PlGF
- Comparison of vegetable oils on the uptake of lutein and zeaxanthin by ARPE-19 cells
- Identifying a novel frameshift pathogenic variant in a Chinese family with neurofibromatosis type 1 and review of literature
- Recurrence risk factors of intravitreal ranibizumab monotherapy in retinopathy of prematurity: a retrospective study at one center
