COVID-19 pandemic impact on ocular trauma in a tertiary hospital
You-Mei Xu, Li-Ping Du, Ya-Dan Huo, Guang-Qi An, Xue-Min Jin, Peng-Yi Zhou
1The Academy of Medical Sciences, Zhengzhou University,Zhengzhou 450000, Henan Province, China
2Department of Ophthalmology, the First Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, Henan Province,China
Abstract
● KEYWORDS: COVID-19; eye emergency; ocular trauma;pandemic
INTRODUCTION
In the end month of 2019, coronavirus disease‐2019(COVID‐19) attacked China and more than 20 countries[1‐3].With the highly transmissible, this novel COVID‐19 has spread all over the world in a short time[4‐5]. These had measures that contained lockdown, being facemask, online education and so on. A nationwide lockdown was obligatory from January to April 2020 in China[6]. Although this was followed by gradual relaxation in phases over the next few months, the lifestyle, transportation, labor, and education of almost all the Chinese people have hugely changed in 2020[7‐10]. In the complete lockdown time, the government implemented public transportation closed, private vehicle restricted, work and study in home. In the rest time of 2020, due to sporadic COVID‐19 case, there had many lifestyle difference that a survey indicated the individuals use transportation services more lower to decrease close contact with other people[11]. There are some changes with daily life in 2020. The first different is the work location, many companies decided allow their employee work at home in pandemic time. In the work style, people did not need to commute workplace and home. The whole traffic had a lower loadings that can reduce traffic accident risks. There had about 50% reduction in traffic accident in the USA while it was in the stay‐at‐home orders[12]. The second different thing is outdoor leisure activities such as hiking, go shopping,eating out,etc. All the activities have been greatly reduced.With safe and social distancing reasons, people must cook at home. This had been stated that a French survey that 42.0%of all participants cooking more frequently[13]. During this phenomenon, people has enhance the chance to use the sharp object which increase danger. The last one was that students were be planed study online at home and not need go to school.Students used digital devices to learn with the education teachers and institutions during the COVID‐19 pandemic[14].Ocular trauma is one of the most important causes of monocular blindness and a major factor in vision loss[15‐16].Ocular trauma has a high prevalence and serious disorders.More than 19 million people has under blindness or low vision due to ocular trauma in the world. It annually recorded the number of 2.0 to 2.4 million cases about ocular trauma which can progress to blindness in the USA[15,17‐18]. There has little paper about number with ocular trauma in China. But it reported that the incidence of ocular trauma was higher than some industrialized countries[19‐20]. Ocular trauma has serious complications that are glaucoma, ocular hypertension,retinal detachment, optic nerve contusion, and proliferative vitreoretinopathy[21‐22]. Thus, it is very important to study the epidemiological characteristics of ocular trauma and then can better prevent with control measures. According to previous research, it has found a greater incidence of ocular trauma occurring outside[23‐24]. It means people are more tend to be hurt in outside place and workplace[25]. In the whole 2020, people have great changes in many different aspects that can alter the epidemiology and prevalence of ocular trauma. Early reports have suggested that total emergency eye visits decreased 40% during the pandemic period. Pandemics can influence patient behavior in seeking emergency medical treatment[26‐27].Meanwhile, the composition of different types of ocular trauma and differences in patient demographic information are varied[28‐30]. In the USA, the mean age of ocular trauma patients was decreased from 49.0 to 36.4 (P<0.001) and patients’injury location was more at home during the pandemic[29]. In Italy, it also had the whole patients cases decreased 45.9%and composition ratio types of ocular trauma changed a lot[31].By investigating the status of ocular trauma, it is possible to understand of ocular trauma in classification, prognosis, and medical treatment within special time, and analyze the causes of this phenomenon, which is conducive to timely adjustment of the prevention and control policy of ocular trauma and achieves effective diagnosis and treatment according to the actual situation.
In this study, we investigated the difference in the demographics and characteristics of ocular trauma between 2019 and 2020 in in the First Affiliated Hospital of Zhengzhou University.Then, we summarize the key influence factors, identify the root causes, and eventually propose several strategies for the prevention and management of ocular trauma during COVID‐19 pandemic.
SUBJECTS AND METHODS
Ethical Approval The study was carried out in accordance with the Helsinki Declaration. The study was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University and the approval number is 2021‐KY‐1147‐001. All participants were fully informed of the purpose and procedures of this study, and written consent was obtained from each subject.
SubjectThis is a retrospective comparative study. We searched the medical records inpatients system of Ophthalmological Department in the First Affiliated Hospital of Zhengzhou University from 2019 to 2020 to collect information on patients who were diagnosed with ocular trauma. We collect the age, sex, admission vision acuity (VA), type of diagnosis,hospital stays, mechanism of injury and location of injury. The 883 patients of 2020 were included as the research group, the 714 patients of 2019 were listed as the control group. If the same patient was treated for the same disease more than once,only the first information was included.
Main Outcome MeasuresPatients were grouped into five classes depending on age: preschool (0‐6y), teenagers (7‐17y), young adults (18‐40y), middle‐aged (41‐65y), and older adults (>65y). The location of injury contained home,outdoors, school, and work. The admission best corrected visual acuity (BCVA) was expressed using the logarithm of the minimum angle of resolution (logMAR). The mechanism of injury includes sharp object, blunt, falls, traffic accident,blast, violence, burns/corrosive substances, and others. The types of ocular trauma were divided into mechanical and non‐mechanical injury. Mechanical ocular trauma was divided into closed‐globe and open‐globe injuries. Closed‐globe injuries were divided into contusion and lamellar laceration. Open‐globe injuries were divided into perforating injury, penetrating injury, intraocular foreign body, and eyeball rupture injury.
Statistical AnalysisWith the Kolmogorov‐Smirnov test,the admission VA was conformed to a normal distribution.The data of the normal distribution are expressed as the mean and the standard deviation. An independent sample of two groups was used to compare ordered variables, such as age,admission VA and hospital stays. Pearson’s square test was used to compare differences in sex, location of injury, type of diagnosis, and mechanism of injury. Bonferroni corrections were applied toP‐values to account for multiple comparisons.All data were analyzed using SPSS 26 Statistics, and a two‐sidedP‐value <0.05 indicated statistical significance.
RESULTS
Demographic InformationThe number of patients that were presented in our Ophthalmology Department and diagnosed with ocular trauma was 883 in 2019 and 714 in 2020. The baseline characteristics of patients presented with ocular trauma are listed in Table 1. The mean age of ocular trauma was 36.74y in 2019 and was 37.12y in 2020. There was no significant difference with mean age between 2019 and 2020(P=0.72). No matter in 2019 or in 2020, the male patient’s cases (713 in 2019, 593 in 2020) were much greater than the number of female patients (170 in 2019, 121 in 2020).There was no statistical significance with gender component in 2019 and 2020. The injury number of in work was also the most within the four types of location in this two year(42.36% in 2019, 43.84% in 2020). The number of injuries suffered outdoors in 2019 decreased compared with that in 2020 (37.71%vs27.31%,P<0.01) as there was a substantial increase in the number of patients in the home group (16.08%vs26.19%,P<0.01). However, the number of patients in the school group may not be significant (34vs19,P=0.19).However, the mean hospital stays were 12.66d in 2019 and were 10.81d in 2020.The mean hospital stays of 2020 was decreased than 2019 (P<0.01). The mean admission VA(logMAR) was 1.75 in 2019 and was 1.92 in 2020. It means the admission VA was worse in 2020, implying that the level of injuries in 2020 was more severe than in 2019.
Number of Ocular Trauma Patients in Every MonthThe total number of patients related to COVID‐19 influence was 883 (mean 73.58±11.25 patients per month) in 2019 and 714(59.50±17.92 patients per month) in 2020. The number of ocular trauma patients for each month is shown in Figure 1.The number of patients drastically reduced in February 2020,as we observed a 5‐fold reduction (91 to 16 patients). Every month number of patients in 2020 was less than 2020 cases.
Age Distributions of Ocular Trauma in 2019 and 2020There were the number of five age groups listed in Figure 2.The highest incidence of ocular trauma was the middle‐aged(41‐65y) groups in 2019 and 2020. The lowest incidence of ocular trauma was the older adults (>65y) in 2019 and 2020.
Mechanism of Injury with Patients Who Presented with Ocular Trauma in 2019 and 2020The mechanism of injury with patients who presented with ocular trauma was shown on the Table 2. The most common cause of ocular trauma was sharp objects in 2019 (47.34%) and 2020 (47.58%). Violence had a significant difference as a cause of ocular trauma between 2019 and 2020 (39vs47,P<0.01). The different causes of ocular trauma were significantexcept for sharp objects, blunt objects,and others (bites or scratches caused by animals, injured by surgery, self‐harm, spontaneous cause).
Type of Ocular Trauma Patients Who Presented in 2019 and 2020The type of ocular injuries was detailed in Table 3.There was no significant difference in non‐mechanical injury and mechanical injury (P=0.08). In closed globe injury,contusion was decreased in 2020 compared to 2019 (25.25%vs19.89%,P<0.01).
Notably, in mechanical injury, there was a significant increase in the number of open‐globe injuries compared with that in 2019 (65.57%vs71.71%,P<0.01). In open‐globe injury, there also had a significant increase in the number of intraocular foreign and eyeball rupture compared with that in 2019(14.61%vs21.71%,P<0.01; 7.93%vs14.85%,P<0.01).

Figure 1 The number of patients in 12mo in 2019 and 2020.

Figure 2 The numbers of patients in four class age groups in 2019 and 2020 Preschool (0-6y), teenager (7-17y), young adults (18-40y),middle-aged (41-65y), older adults (>65y).
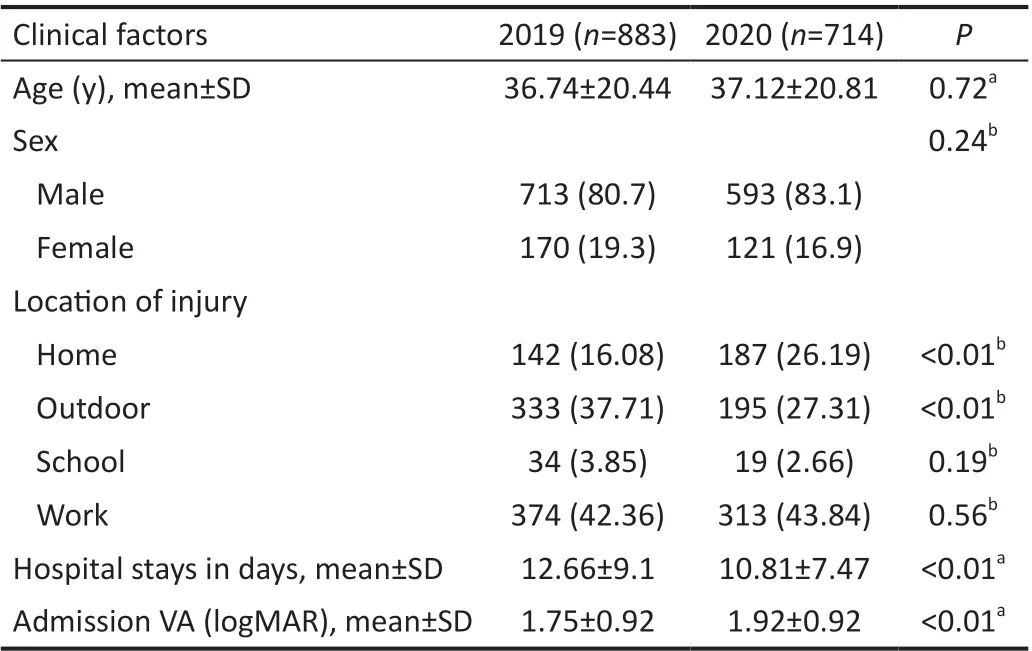
Table 1 Baseline characteristics of patients who presented with ocular trauma in 2019 and 2020 n (%)
DISCUSSION
The COVID‐19 pandemic has changed people’s way of life[7‐10]. In our study, it has decreased 19.1% cases in 2020 compared to 2019 (883 in 2019, 714 in 2020). The most significant decrease (84%) was observed in our hospital in February 2020. There has the same trend in other country’s reports. The number of ocular trauma cases in the USA dropped by 20% in 2020[29]. The frequency of ocular traumaalso declined in countries like England and Italy during the COVID‐19 pandemic in 2020[31‐32]. In the whole 2020, these had different levels lockdown and restrictions in China and other countries especially in February[33‐34]. These measures reduced movement of people between areas. The mean age and sex radio of ocular trauma have not statistical significance between 2019 and 2020 (2019: 36.74y, 2020: 37.12y,P=0.72;2019, male: 80.7%, 2020, male: 83.1%).
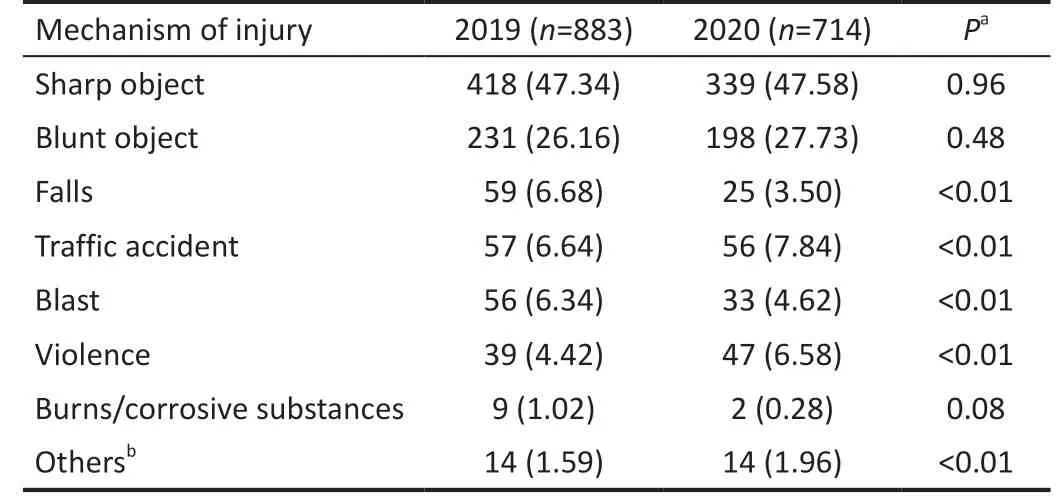
Table 2 Mechanism of injury with patients who presented with ocular trauma in 2019 and 2020 n (%)

Table 3 Types of ocular trauma patients who presented in 2019 and 2020 n (%)
The gender ratio agrees with the published studies[30,35‐36]. The reason is all types of factories and manual labor are dominated by men, and men have higher rates of alcoholism and reckless driving[37]. Meanwhile, the middle‐aged (41‐65y) was the most distribution in ocular trauma patients between 2019 and 2020. Although the main injured group of eye trauma is still controversial, but a paper has reported that the 41‐50y and 51‐60y age groups people are at high risk of ocular trauma[38]. So it is very important strengthen eye protection in manual workers.
The injury number of in work was also the most within the four types of location in this two year (42.36% in 2019,43.84% in 2020). Ocular trauma mainly occurs in manual workers. Even during the epidemic, the risk of eye injuries in this manual labor has not declined. This is consistent with the previously reported location of ocular trauma in Beijing[25].The number of injuries suffered outdoors in 2019 decreased compared with that in 2020 (37.71%vs27.31%,P<0.01) as there was a substantial increase in the number of patients in the home group (16.08%vs26.19%,P<0.01). Due to the policy of home isolation, the proportion of injuries at home will increase from 16.08% in 2019 to 26.19% in 2020 (P<0.01). During this period, the proportion of home‐injured ocular trauma patients who visited the Wills Ophthalmology Department increased from 20% in 2019 to 84% in 2020[28]. It also important to be cautious in our daily life at home.
The mean hospital stays were 12.66d in 2019 and were 10.81d in 2020. The mean hospital stays of 2020 was decreased than 2019 (P<0.01). The hospital stays in 2020 was shorted compared to 2019. A decline in hospital admissions for different diseases was reported[26‐27]. During a special period, hospital admissions dropped significantly, the total load decreased, elective surgeries were delayed, and the occurrence of emergency illnesses and surgeries increased.Patients are more likely to seek medicine help in global public health period time. The mean admission VA (logMAR) was 1.75±0.92 in 2019 and was 1.92±0.92 in 2020. It means the admission VA was worse in 2020, implying that the level of injuries in 2020 was more severe than in 2019. But, about the level of injuries, there had same situation in the USA reports[29].This suggests that although the number of patients during the epidemic decreased compared with before, the serious types in the proportion of patients increased. The treatment in patients should be more effective and suitable in short time.For patients, even in special periods, eye damage should not be ignored and must seek medical help in time.
About the mechanism of ocular trauma, the most common cause of ocular trauma was sharp object in 2019 (47.34%)and 2020 (47.58%,P=0.96). The cause of ocular trauma is related to the occupation and age of the patient, and most of them are injuries caused by life or work events. In this study,the main cause of ocular trauma in the control group and the study group was injured with sharp objects. This is consistent with Beijing’s research on ocular trauma. Injury cause of major ocular trauma is flying object[38]. The cause of eye trauma is related to the occupation and age of the patient, and most of them are injuries caused by life or work events. Workers are mostly in construction, metal cutting, drilling and other related types of work. Violence and others had a significant difference as a cause of ocular trauma between 2019 and 2020(39vs47,P<0.01). Others in our study contains caused by self‐harm, animals, injured by surgery, spontaneous cause and so on. A survey about associations between feelings and behaviors with lockdown during COVID‐19 pandemic shows 12.33% of all participants reported depression and 6.26% of all participants reported anxiety after lockdown[39]. It suggested it is very important to keep mind healthy during special times.The results of the injury mechanism data showed an increase in traffic accidents (6.64%vs7.84%,P<0.01). Strict traffic controls resulted in a significant decrease in the use of public transport for some months, making more people use their privatecarsto achieve their urgent needs[6].
About types of ocular trauma patients, there was no significant difference in non‐mechanical injury and mechanical injury(P=0.08). In closed globe injury, contusion was decreased in 2020 compared to 2019 (25.25%vs19.89%,P<0.01). Notably,in mechanical injury, there was a significant increase in the number of open‐globe injuries compared with that in 2019(65.57%vs71.71%,P<0.01). Mechanical ocular trauma is still the main injury type of hospitalized patients with ocular trauma in China[25,38]. The proportion of mechanical ocular trauma in this study was higher than that reported, reaching 98.98% in 2019 and 99.72% in 2020, which may be related to the fact that the subjects of this study were hospitalized patients. In this study, the proportion of open globe injuries was higher than that of closed globe injury, and the proportion of open ocular trauma in the study group (71.71%) was higher than that in the control group (65.57%). The reason may be that some patients with closed ocular trauma did not receive hospitalization during the epidemic, and the proportion of hospitalized patients with open ocular trauma increased accordingly.
In open‐globe injury, there also had a significant increase in the number of intraocular foreign and eyeball rupture compared with that in 2019 (14.61%vs21.71%,P<0.01; 7.93%vs14.85%,P<0.01). In this study, perforating injury accounted for the highest proportion in open ocular trauma, with perforating injury in the control group and study group accounting for 39.07% and 32.91%, respectively, and intraocular foreign bodies in 14.61% and 21.71%, which were consistent with the above reports. This means the number of eye injuries decreased while the severity of eye injuries increased. Previous reports also support these findings in other countries[28‐29,31].To sum up, during the coronavirus epidemic, the total number of ocular injuries was significantly reduced compared with before, middle‐aged and young adults are still high incident groups. Ocular trauma was more severe. For normal people,we need not to ignore eye injuries during epidemic. For our medical workers, we should deal with ophthalmic patients more efficiently and try our best to protect patients’ vision.
There are still shortcomings in this study, such as the lack of epidemiological information on outpatient ophthalmology during the epidemic, and the lack of multi‐center data, which may be biased. Further research at a later stage.
In conclusion, during the pandemic, the number of patients with ocular trauma decreased, but middle‐aged (41‐65y) are still high incident groups. Mechanical ocular trauma remains the leading cause of hospitalization for ocular trauma patients and the proportion of patients injured at home increased. The severity of ocular trauma increased significantly. It is necessary to arouse social attention and the public’s awareness of eye trauma protection should be strengthened during the pandemic.
ACKNOWLEDGEMENTS
Authors’ contributions: Xu YM and Huo YD analyzed and interpreted the patient data and drafted the manuscript. An GQ collected clinical data and helped draft the manuscript.Du LP, Jin XM, and Zhou PY participated in the draft of the manuscript. All authors read and approved the final manuscript.Foundations: Supported by National Natural Science Foundation of China (No.81800832; No.81970792;No.8217040); Medical Science and Technology Project of Health Commission of Henan Province (No.YXKC2020026).
Conflicts of Interest: Xu YM, None;Du LP,None;Huo YD,None;An GQ,None;Jin XM,None;Zhou PY,None.
 International Journal of Ophthalmology2023年1期
International Journal of Ophthalmology2023年1期
- International Journal of Ophthalmology的其它文章
- Instructions for Authors
- Morphological and functional changes in the macular area in diabetic macular edema after a single intravitreal injection of aflibercept
- Macular vascularisation changes analysed using OCT angiography after successful rhegmatogenous retinal detachment repair
- Comparison of success rate and intraocular pressure spikes between selective laser trabeculoplasty and micropulse laser trabeculoplasty in African American and Hispanic patients
- Efficacy of custom-made soft keratoconus lenses on corneal aberrations and photic phenomena in patients with keratoconus: a corneal topography imaging based study
- Clinical observation of recombinant human nerve growth factor in the treatment of neurotrophic keratitis
