Postoperative outcomes and recurrence patterns of intermediate-stage hepatocellular carcinoma dictated by the sum of tumor size and number
Xin-Sheng Hu,Hui-Yuan Yang, Chao Leng,Zhi-Wei Zhang
Abstract
Key Words: Hepatocellular carcinoma; Multinodular; Intermediate-stage; Liver resection; Recurrence pattern; Prognosis
INTRODUCTION
As the sixth most common cancer globally, primary liver cancer accounted for 906,000 newly confirmed cancer cases and 830,000 cancer-related deaths worldwide in 2020, of which 75%-85% were hepatocellular carcinoma (HCC)[1].
Barcelona Clinic Liver Cancer (BCLC) staging system, which was proposed in 1999, has been widely used to guide treatment decisions in patients with HCC[2,3]. The 2022 version of the BCLC strategy recommends liver transplantation (LT), transarterial chemoembolization (TACE), and systemic therapy,respectively, for BCLC intermediate-stage HCC patients based on their expected survival time[4].
In addition, emerging studies have suggested that liver resection (LR) may also be a good treatment option for BCLC-B HCC patients[5,6]. Nevertheless, the subgroups of BCLC-B HCC patients who would truly benefit from LR have yet to be defined. Several previous studies found that some BCLC-B HCC patients undergoing LR had favorable long-term overall survival (OS) rates (5-year OS rates: 50%-75%);however, these selected patients still had high postoperative recurrence rates (2-year recurrence rate: ≥50%), which means that many of these patients had good recurrence-to-death survival (RTDS)[7,8]. Both recurrence patterns and treatments after recurrence can affect the RTDS of HCC patients who develop recurrence after LR[9-11]. However, previous studies did not analyze the main reasons why these selected patients had good RTDS, which may affect the judgment of the role of LR in these patients[7,8].
In this study, we retrospectively included patients undergoing curative LR for BCLC stage A or B multinodular HCC (MNHCC) and stratified the BCLC-B patients by the sum of tumor size and number(N + S), which combines the two main prognostic factors of BCLC-B patients into a continuous variable[7,8]. BCLC-B patients more suitable for LR were identified by comparing the outcomes, recurrence patterns, and treatments after recurrence in BCLC-B patients in each subgroup with those in BCLC-A patients.
MATERIALS AND METHODS
Patients
We enrolled BCLC stage A or B MNHCC patients who underwent curative LR in Tongji Hospital from January 2010 to May 2018. The inclusion criteria were: (1) MNHCC pathologically diagnosed with two or more nodules, in which lesions less than 1 cm in diameter and less than 2 cm away from the main nodule were defined as satellite nodules[12]; (2) Curative resection, defined as complete macroscopic removal of all tumors with negative histologic resection margins for the tumors (R0 resection)[13,14];and (3) No preoperative anticancer treatment other than TACE. The exclusion criteria were: (1) Recurrent HCC or combined HCC and cholangiocarcinoma; and (2) Complicated with other malignancies.
Data collection
Patient data at the time of initial hepatectomy including sex, age, body mass index, hepatitis B antigen status, liver function, tumor characteristics, surgical procedure, and preoperative treatment were recorded. Liver function in this study was classified by the albumin-bilirubin score[15]. Maximum tumor size was defined as the maximum diameter of the largest tumor. Microvascular invasion was defined as tumor within a vascular space lined by endothelium that was visible only on microscopy[16].In addition, the recurrence patterns, which consisted of recurrence time and tumor characteristics at the time of recurrence, and treatments after recurrence in those patients who developed recurrence during follow-up were also recorded. Recurrence time was defined as the time between initial LR and the first recurrence.
Initial hepatectomy
In our center, we routinely estimated the residual liver volume in MNHCC patients before hepatectomy,and only patients with residual liver volume of more than 40% of the standard liver volume (for patients with liver cirrhosis) or more than 30% (for patients without liver cirrhosis) would receive LR[17,18]. The decision to perform anatomical or non-anatomical hepatectomy depended largely on the tumor distribution, and major resection was defined as the resection of three or more Couinaud liver segments[19]. Intraoperative ultrasound was routinely used to locate the tumor and screen the nodules.All nodules were completely resected intraoperatively and negative margin was determined according to postoperative pathology.
Follow-up
Patients were followed every month with measurement of serum alpha-fetoprotein (AFP), chest radiography and ultrasound or computed tomography (CT) or magnetic resonance imaging (MRI) in the first 6 mo after discharge from hospital, and every 3-6 mo thereafter. When HCC recurrence was confirmed by CT or MRI, patients were treated with repeated hepatectomy, ablation, TACE or systemic therapy. Follow-up was terminated on May 15, 2022.
Recurrence-free survival (RFS) was calculated from the date of hepatectomy until recurrence or last follow-up. OS was defined as the time from LR to death or last follow-up, and RTDS was defined as the time from recurrence to death or last follow-up.
Statistical analysis
Continuous variables were presented as mean ± SD or median (interquartile range; IQR). Categorical variables were described by frequency and percentage. In the comparison of different subgroups,continuous variables were compared using the Student’stor Mann-WhitneyUtest, and categorical variables using theχ2or Fisher’s exact test, as appropriate. Survival was analyzed by the Kaplan-Meier method, and survival curves were compared by the log-rank test. Univariate and multivariate analyses were based on the Cox proportional analysis. Variables withPvalues less than 0.1 identified by the univariate analysis were included in multivariate analysis. The cutoff value of N + S was determined by X-tile, a bioinformatics tool produced by Camp and colleagues[20]. The area under receiver operating characteristic (ROC) curve (AUC) was compared using DeLong test[21].P< 0.05 was considered to indicate statistical significance. Both SPSS (version 23.0, SPSS, Inc., Chicago, IL, United States) and MedCalc software (version 20.115, MedCalc Software, Ostend, Belgium) were used for the analysis.
RESULTS
Variables and outcomes of the entire cohort
A total of 143 patients who underwent curative LR for BCLC stage A or B MNHCC were enrolled. Their mean age was 52.1 years and most patients were male (n= 134, 93.7%) and were hepatitis B surface antigen positive (n= 131, 91.6%). Median maximum tumor size in the entire cohort was 5.6 cm (IQR:3.4-7.6) and tumor number in the vast majority of patients was ≤ 3 (n= 136, 95.1%). Overall, 17.5% (n=25) of patients had BCLC-A MNHCC, and 82.5% (n= 118) had BCLC-B MNHCC (Table 1).
After a median follow-up of 54 mo (IQR 27-79), 5-year OS and RFS after R0 resection in all patients were 60.2% and 23.2%, respectively. Of note, BCLC-B patients had worse 5-year OS (57.2%vs74.1%,P=0.028, Supplementary Figure 1A) and RFS (19.4%vs41.6%,P= 0.002, Supplementary Figure 1B).
Stratification of BCLC-B patients based on N + S
Among patients undergoing LR for BCLC-B HCC, the median maximum tumor size was 6.2 cm (IQR:4.1-8.4) and tumor number in 111 (94.1%) patients was ≤ 3. Of note, 43.2% (n= 51) of patients had bilateral disease and 14.4% (n= 17) of patients underwent TACE before initial LR (Table 1).
Using the X-tile program[20], patients with BCLC-B HCC were divided into two groups by N + S:BCLC-B1 (≤ 10,n= 83, 70.3%), BCLC-B2 (> 10,n= 35, 29.7%) (Supplementary Figure 2).
The prognostic ability of N + S and the rationality of the cut-off value of 10 were then verified by time-dependent ROC curves and Cox-regression analysis. The AUCs for 3-year and 5-year OS in BCLCB patients were 0.650 and 0.646, respectively, for N + S, and 0.640 and 0.643, respectively, for stratification according to N + S (Figure 1). Multivariate analysis showed that N + S > 10 was an independent risk factor for OS [hazard ratio (HR) 2.996, 1.779 to 5.045; P < 0.001] (Table 2) and RFS (HR 1.657, 1.057 to 2.596;P= 0.028) (Table 3) in BCLC-B patients.
In addition, we compared the predictive accuracy of N + S with those of tumor burden score (TBS)and total tumor volume (TTV), both of which were previous prognostic models based on tumor size and number of HCC patients[22,23]. The results showed that the AUCs of N + S at 3 and 5 years were both similar to those of TBS (3-year AUC, 0.650vs0.646,P= 0.552; 5-year AUC, 0.646vs0.643,P= 0.762) and TTV (3-year AUC, 0.650vs0.628,P= 0.171; 5-year AUC, 0.646vs0.636,P= 0.535) (Figure 1).
Comparison of the clinical characteristics, OS, and RFS among BCLC-A, BCLC-B1 and BCLC-B2 patients
Clinical characteristics, OS and RFS of patients with BCLC-B1, BCLC-B2, and BCLC-A were compared(Figure 2, Supplementary Table 1). The results showed that BCLC-B2 patients had a higher serum AFP level and a larger proportion of bilateral tumor distribution, compared to patients with BCLC-A and BCLC-B1. With an increase in N + S, the maximum tumor size gradually increased, and a larger proportion of patients underwent major resection (Supplementary Table 1).
Both BCLC-A patients and BCLC-B1 patients had good 5-year OS (74.1%vs67.4%,P= 0.250), which was better than that in BCLC-B2 patients (74.1%vs33.6%,P< 0.001; 67.4%vs33.6%,P< 0.001)(Figure 2A). Compared with BCLC-A patients, BCLC-B1 patients had a worse RFS (median RFS: 19 movs48 mo;P= 0.022), which was better than that in BCLC-B2 patients (median RFS: 19 movs7 mo;P<0.001) (Figure 2B).

Table 1 Characteristics of patients with Barcelona Clinic Liver Cancer stage A or B multinodular hepatocellular carcinoma, n (%)
Comparison of recurrence patterns, treatments after recurrence, and RTDS in BCLC-A, BCLC-B1 and BCLC-B2 patients
During follow-up, 14 (56%) BCLC-A, 66 (79.5%) BCLC-B1 and 34 (97.1%) BCLC-B2 patients developed recurrences (P< 0.001). Nine BCLC-B1 and 4 BCLC-B2 patients who lacked information on tumor characteristics at the time of recurrence and treatments after recurrence were excluded from the analysis. Ultimately, 14 BCLC-A, 57 BCLC-B1 and 30 BCLC-B2 patients with recurrence were included in the analysis. The recurrence patterns and treatments after recurrence in these patients are summarized in Supplementary Table 2.
Compared with BCLC-A and BCLC-B1 patients, BCLC-B2 patients had a shorter recurrence time and a higher proportion of recurrence with macrovascular invasion and/or extrahepatic metastasis.However, there were no significant statistical differences in recurrence patterns and treatment after recurrence between BCLC-B1 and BCLC-A patients. Fewer BCLC-B2 patients underwent curative treatments after recurrence than BCLC-A patients, but the treatment after recurrence was similar between BCLC-B2 patients and BCLC-B1 patients (Supplementary Table 2).
Both BCLC-B1 and BCLC-A patients had good RTDS (median RTDS: Not reached,vs49 mo for BCLC-B1 and BCLC-A patients, respectively;P= 0.599), while BCLC-B2 patients had a worse RTDS (16 movsnot reached,P< 0.001; 16 movs49 mo,P= 0.042) (Figure 3).

Table 2 Univariate and multivariate analysis of overall survival in patients with Barcelona Clinic Liver Cancer stage B hepatocellular carcinoma
Independent risk factors for RTDS
We further conducted a multivariate analysis of the factors affecting RTDS of BCLC stage A or B MNHCC patients undergoing LR. Multivariate analysis showed that initial tumor with BCLC-B2 (N + S> 10) (HR 2.696, 1.468 to 4.953;P= 0.001), recurrence within 2-year (HR 4.353, 1.024 to 18.503;P= 0.046),recurrent tumor number > 3 (HR 3.247, 1.629 to 6.474;P= 0.001), recurrence with macrovascular invasion and/or extrahepatic spread (HR 2.894, 1.458 to 5.746;P= 0.002) and noncurative treatments after recurrence (HR 2.423, 1.209 to 4.854;P= 0.013) were independent risk factors for RTDS(Supplementary Table 3).
DISCUSSION
The role of LR in BCLC-B HCC patients is unclear. Although the latest BCLC staging system still does not recommend LR for BCLC-B patients, the results of emerging studies have indicated that LR resulted in a good 5-year OS for BCLC-B HCC patients[4-6]. In this study, patients who underwent LR for BCLCB HCC had an overall 5-year OS rate of 57.2%, which demonstrated that LR was a good treatment option in these patients.
To select BCLC-B patients more suitable for LR, we stratified these patients according to N + S, which has been used to select HCC patients who are more suitable for LT and for TACE[24,25]. In fact,Matsukumaet al[26] suggested that N + S was a good prognostic factor for BCLC-B HCC patients undergoing hepatectomy. The present study increased the cutoff point of N + S from 8 to 10, which may be related to different study cohorts and different calculation methods used for the cutoff value[26].Nevertheless, the results of this study and in the study by Matsukumaet al[26] demonstrated that N + S could predict the recurrence and OS of BCLC-B HCC patients undergoing hepatectomy. In addition, the present study showed that N + S had a predictive accuracy similar to TBS and TTV in predicting OS inBCLC-B patients. However, compared with the complicated calculation of TBS and TTV, the calculation of N + S is simpler and more suitable for clinical application.
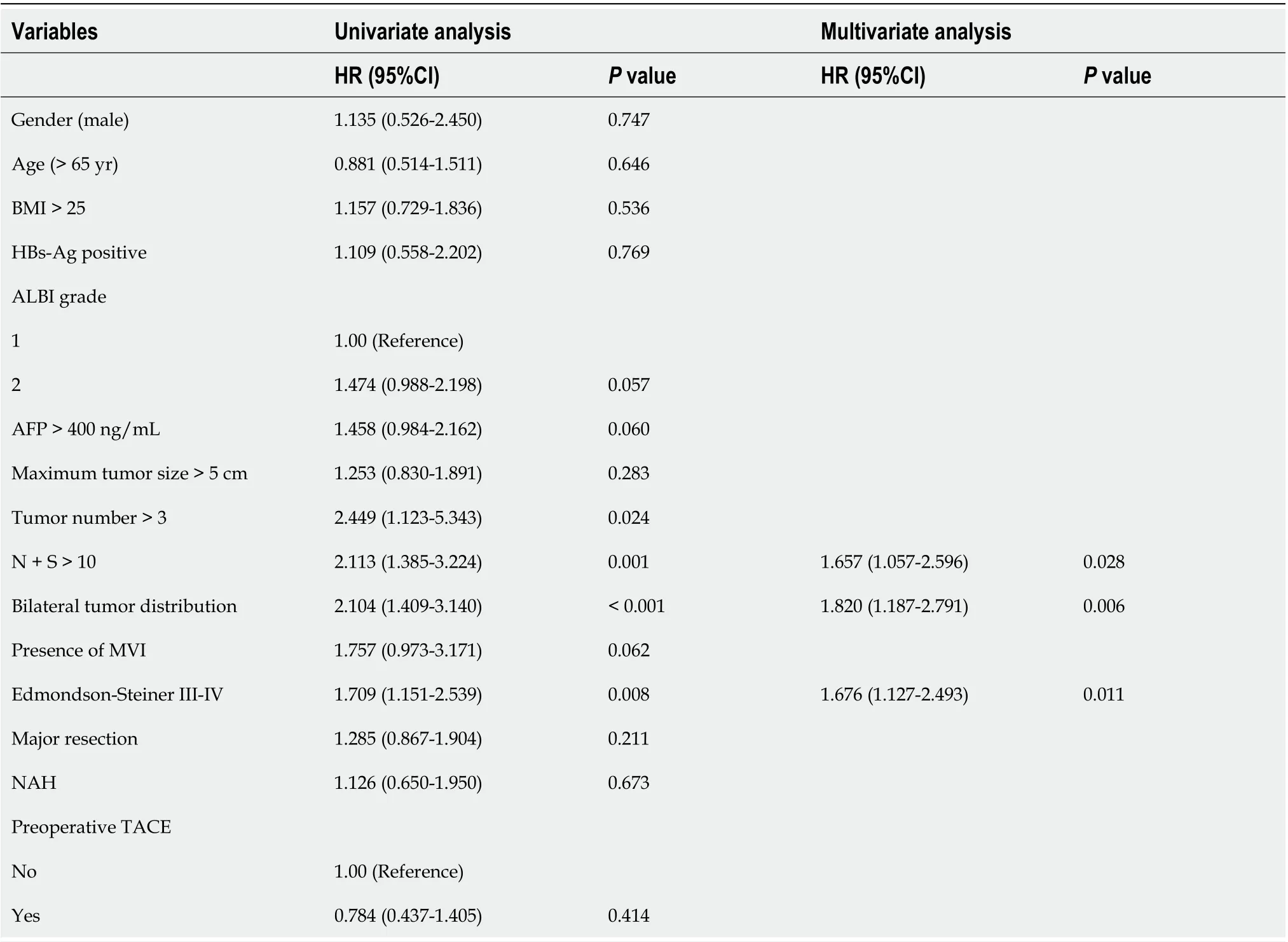
Table 3 Univariate and multivariate analysis of recurrence-free survival in patients with Barcelona Clinic Liver Cancer stage B hepatocellular carcinoma
Previous studies have focused on the OS when selecting BCLC-B patients for LR, and ignored that those selected patients still had a high postoperative recurrence rate[7,8]. In order to demonstrate that the selected BCLC-B HCC patients truly benefit from LR rather than remedial treatments after recurrence, and to better understand the tumor characteristics of the selected patients, we compared not only the OS and RFS, but also the RTDS, recurrence patterns, and treatments after recurrence.
In the present study, BCLC-B1 (BCLC-B with N + S ≤ 10) HCC patients were considered as BCLC-B HCC patients who likely benefitted most from LR. Although BCLC-B1 HCC patients were still more likely to develop recurrence after LR than BCLC-A MNHCC patients, these BCLC-B1 patients had mild recurrence pattern, good RTDS and excellent OS similar to BCLC-A MNHCC patients.
However, BCLC-B2 (BCLC-B with N + S > 10) HCC patients not only had a high postoperative recurrence rate, but also an aggressive recurrence pattern. Although the treatment after recurrence was similar between BCLC-B2 patients and BCLC-B1 patients, the BCLC-B2 patients still had a worse RTDS.The long-term OS of BCLC-B2 patients undergoing LR is not satisfactory.
To the best of our knowledge, this study is the first to demonstrate that N + S could predict not only prognosis in BCLC-B HCC patients, but also the recurrence patterns and RTDS in these patients.
In addition, it is interesting to note that patients with BCLC-B1 HCC had worse RFS but comparable OS than patients with BCLC-A MNHCC in this study. In fact, previous studies comparing LTvsLR in HCC patients found a similar phenomenon. These studies showed that although patients receiving LR had a higher rate of postoperative recurrence, the 5-year OS between LR and LT was comparable[27,28].Previous studies have suggested that the reasons for this phenomenon may be related to noncancerous death in the LT group and treatment after recurrence in the LR group, and our results suggest that it may also be related to the recurrence patterns after LR.
As a single-center retrospective study, the present study has some limitations. Firstly, the sample size was small, which may have affected the accuracy of the results. Secondly, there was a lack of comparison of treatment options other than LR. Some patients with BCLC-B HCC and N + S ≤ 10 would meet the ‘Extended Liver Transplant criteria’, and the best treatment option for these patients remains to be explored[29]. Finally, the results of this study need to be verified by an external cohort.
CONCLUSION
N + S is a good measure that could predict the OS, RFS, RTDS and recurrence patterns in BCLC-B HCC patients undergoing LR. In particular, BCLC-B patients with N + S ≤ 10 had survivals similar to those of BCLC-A MNHCC patients. Given the computational simplicity of N + S, it is worth exploring the application of N + S to guide decision-making in the treatment of BCLC-B patients.
ARTICLE HIGHLIGHTS
Research motivation
There is a lack of studies on whether the sum of tumor size and number (N + S) can be used to select BCLC-B patients who are more suitable for LR. The effect of recurrence patterns on long-term survival in BCLC-B patients undergoing LR is also poorly explored.
Research objectives
The present study aimed to identify BCLC-B patients more suitable for LR and to further analyze the reasons why these patients could benefit from LR.
Research methods
BCLC stage A or B multinodular HCC (MNHCC) patients undergoing curative hepatectomy were enrolled. Overall survival (OS), recurrence-free survival (RFS), recurrence-to-death survival (RTDS),recurrence patterns, and treatments after recurrence in BCLC-B patients in each subgroup according to N + S were compared with those in BCLC-A patients.
Research results
N + S could predict not only the OS and RFS in BCLC-B HCC patients undergoing hepatectomy, but also the recurrence patterns and RTDS in these patients. BCLC-B patients with N + S ≤ 10 had mild recurrence patterns, good RTDS and excellent OS similar to those in BCLC-A MNHCC patients.
Research conclusions
N + S can be used to select BCLC-B HCC patients who are more suitable for LR, and LR should be considered in BCLC-B patients with N + S ≤ 10.
Research perspectives
As a measure that can be easily obtained and calculated in clinical practice, N + S can help with the clinical decision-making in the treatment of BCLC-B HCC patients.
FOOTNOTES
Author contributions:Hu XS performed the research and wrote the paper; Yang HY performed the follow-up; Leng C designed the research and supervised the report; Zhang ZW provided clinical advice and supervised the report; and all authors read and approved the final version.
Institutional review board statement:This study was reviewed and approved by the Ethics Committee of the Tongji Hospital of Tongji Medical College of Huazhong University of Science and Technology (Approval No. TJIRB20210918).
Informed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Xin-Sheng Hu 0000-0002-0863-7909; Hui-Yuan Yang 0000-0003-0877-656X; Chao Leng 0000-0002-5391-651X; Zhi-Wei Zhang 0000-0002-4679-2598.
S-Editor:Liu GL
L-Editor:A
P-Editor:Liu GL
 World Journal of Gastroenterology2022年44期
World Journal of Gastroenterology2022年44期
- World Journal of Gastroenterology的其它文章
- Comment on “Prognostic value of preoperative enhanced computed tomography as a quantitative imaging biomarker in pancreatic cancer”
- Randomized controlled trial to evaluate the efficacy and safety of fexuprazan compared with esomeprazole in erosive esophagitis
- Virological and histological evaluation of intestinal samples in COVID-19 patients
- Glucagon-like peptide-2 analogues for Crohn’s disease patients with short bowel syndrome and intestinal failure
- Development of Epstein-Barr virus-associated gastric cancer: Infection, inflammation, and oncogenesis
- Machine learning insights concerning inflammatory and liver-related risk comorbidities in noncommunicable and viral diseases
