Using echocardiography in newborn screening for congenital heart disease may reduce missed diagnoses
un-Xiang Qiu · Wei Jiang Y · Jia-Yu Zhang · Die Li · Kai uY · Cang-Cang Fu · Xiao-Min aTng · Wei-Ze Xu
Congenital heart disease (CHD) is the most common type of birth defect in China. According to a national study, the overall prevalences of CHD and critical CHD were 8.98 per 1000 live births and 1.46 per 1000 live births, respectively,in China [ 1]. CHD, particularly critical CHD, not only seriously aff ects the quality of life of patients and their family,but creates huge economic and mental burdens on the family and on society as a whole [ 2]. Early diagnosis of CHD is imperative for early intervention and treatment. For early diagnosis of CHD, CHD screening in all newborns was f irst initiated in Shanghai, China on June 1, 2016 [ 3]. Since July 30, 2018, the China National Health Commission initiated newborn screening program for CHD; “double index methods” (cardiac auscultation plus pulse oximetry) were used to screen CHD for newborns 6 hours and 72 hours after birth.
In Zhejiang province, China, CHD screening was carried out in all newborns since January 1, 2019. Costs of “double index methods” have been free since January 1, 2020 in Zhejiang province. Although CHD screening has been carried out for 3 years in Zhejiang province, many cases of CHD were unrecognized during the neonatal period and were diagnosed later in our tertiary children’s hospital. We aimed to f ind the factors related with the missed diagnosis at screening. Therefore, we carried out a pilot CHD screening program using echocardiography and “double index methods” in f ive secondary-care hospitals. All staff members in the CHD screening program have been trained before the study.
From August 1, 2020 to July 31, 2021, we selected f ive secondary-care hospitals (four maternity hospitals) in f ive counties for this pilot study; 4665 newborns delivered at the f ive hospitals were screened using both “double index methods” and echocardiography on a voluntary basis. The demographic data of subjects are shown in Table 1. Newborns who were diagnosed with CHD prenatally were excluded from this study. The severity of CHD was def ined based on Ewer et al.: critical CHD, defects causing death or needing intervention before 28 days after birth, such as tetralogy of Fallot and total anomalous pulmonary venous connection; serious CHD, defects requiring intervention before age 1 year; signif icant CHD, defects persisting beyond age 6 months, but not classif ied as critical or serious, like small patent ductus arteriosus (PDA); and nonsignif icant, defects not physically appreciable and not persisting after age 6 months [ 4]. All diagnoses in this study were made according to the echocardiography conducted by trained doctors in secondary-care hospitals and checked by our hospital. We calculated sensitivity, specif icity, and false-negative rate of using the “double index method’ to detect diff erent severities of CHD.
During the study period a total of 168 newborns were screened positive by single cardiac auscultation and 181 positive by “double index methods”. Among them, 22 newborns were diagnosed with CHD by echocardiography (critical CHD, 3; serious CHD, 5; signif icant CHD, 14) (Fig. 1).Among the 4484 newborns screened negative by “double index methods”, 204 newborns were diagnosed with CHD(serious CHD, 67; signif icant CHD, 137). Spectrum of the diagnosed CHD is shown in Table 2 . Among the 226 newborns diagnosed with CHD by echocardiography, atrial septal defect (ASD) (combined with PDA or persistent pulmonary hypertension of the newborn) and ASD plus ventricular septal defect were the most common types. The detection rates of critical CHD, serious CHD and signif icant CHD using “double index method” are 100%, 6.9%, and 9.3%,respectively.
Our results were consistent with a previous study that“double index methods” had enough sensitivity and high specif icity in detecting critical CHD [ 5]. However, misseddiagnoses can still occur, especially in patients with severe CHD who need to be managed or followed-up. Even in highincome countries, about 13—48% of newborn babies with critical CHD leave the hospital undiagnosed [ 6]. The proportion may be higher in low-income countries or regions. We found that trained physicians in secondary-care maternity hospitals are still less able to clinically diagnose CHD, and auscultation technique in neonatologists or pediatricians was still lower than their peers in tertiary hospitals. Klocko et al.suggested that clinicians’ auscultation skills can wither if they do not have contact with patients with valvular heart disease during clinical practice, or if they rely on echocardiography [ 7]. Neonatologists or pediatricians in secondary hospitals in China were less likely to be trained in pediatric cardiology which limited their experiences in identifying murmurs. A large portion of patients have been found to be undiagnosed and delayed to be treated which will compromise the optimal outcome [ 8].
Table 1 Demographic data of subjects in this cohort
interquartile range
Variables Regions Total Fuyang Lishui Pingyang Qujiang Wenling Number of individuals 1727 463 1142 758 575 4665 Mother age (y), median (IQR) 29.03 (26.56—32.27)28.75 (25.85—32.57)29.55 (26.74—32.62)29.26 (25.75—33.58)28.81 (25.28—32.76)29.12 (26.26—32.63)Baby gender (male/female) 1.15 1.36 1.23 0.94 1.23 1.16
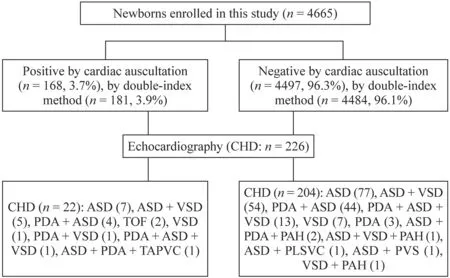
Fig. 1 Flowchart of screening procedure and statistic results. CHD congenital heart disease, ASD atrial septal defect, VSD ventricular septal defect, PDA patent ductus arteriosus, TOF tetralogy of Fallot,TAPVC total anomalous pulmonary venous connection, PAH pulmonary arterial hypertension, PLSVC persistent left superior vena cava,PVS pulmonary vein stenosis
Table 2 Spectrum of congenital heart disease diagnosed in this cohort
congenital heart disease, tetralogy of Fallot, total anomalous pulmonary venous connection, atrial septal defect, ventricular septal defect, patent ductus arteriosus, persistent pulmonary hypertension of the newborn
Variables CHD diagnosed by echocardiography after screening positive by“double index method”CHD diagnosed by echocardiography after screening negative by “double index method”Total number Number Gestational age (≤ 35 wk)Gestational age (> 35 wk)Number Gestational age (≤ 35 wk)Gestational age (> 35 wk)Critical CHD 3 0 3 0 0 0 3 TOF 2 0 2 0 0 0 2 TAPVC 1 0 1 0 0 0 1 (combined with ASD and PDA)Other CHD 223 Pulmonary stenosis 0 0 0 1 0 1 1 (combined with ASD)ASD + VSD 6 0 6 69 2 67 75 (combined with PDA or PPHN)ASD 11 0 11 123 4 119 134 (combined with PDA or PPHN)VSD 2 0 2 8 0 8 10 (combined with PDA or PPHN)PDA 0 0 0 3 1 2 3
Based on the results of this pilot CHD screening results, we propose using echocardiography for CHD screening in wellprivileged areas for the following four reasons: (1) prenatal ultrasonography and echocardiography have been carried out routinely in prenatal screening; (2) echocardiography examination for newborns may be more easy to be trained in maternity hospitals because they have been well trained in prenatal ultrasonography screening; (3) the cost of echocardiography for newborn is relatively low (only US$3—5 after medical reimbursement); (4) echocardiography examination is helpful to screen out newborns with CHD which may be undiagnosed in secondary-care hospitals.
In conclusion, a large portion of newborns with CHD have been found to be undiagnosed and delayed to be treated in secondary-care hospitals. Physicians involved in newborn CHD screening in secondary-care hospitals require more training in pediatric cardiology. Children with CHD should be diagnosed in secondary-care hospitals. Therefore, echocardiography can be used for integrating newborn CHD screening and diagnosis in well-privileged areas in China.
Acknowledgements
The authors thank all the staff members at the Network Platform of Congenital Heart Disease, the National Clinical Research Center for Child Health and f ive secondary-care hospitals for their assistance.Author contributions
QYX and JW contributed equally to this article.QYX contributed to conceptualization, data curation, formal analysis,writing of the original draft. JW contributed to data curation, formal analysis, validation, visualization, reviewing and editing. ZJY contributed to visualization, reviewing and editing. LD and YK contributed to data curation, reviewing and editing. FCC and TXM contributed to reviewing and editing. XWZ contributed to conceptualization, funding acquisition, supervision. All the authors approved the f inal version of the manuscript.Funding
This work was supported in part by the Zhejiang Province Key Research and Development Project (2020C03120 and 2022C03087).Data availability
The data supporting the f indings of this study are available from the corresponding author upon reasonable request.Declarations
Ethical approval
This study has been approved by China Clinical Trial Registration Center (registration number: 2019-IRB-146) and the Ethics Committee of Children’s Hospital, Zhejiang University School of Medicine. All participants and their guardians understood the content and signif icance of the study and signed informed consent forms before participating.Conflict of interest
No f inancial or non-f inancial benef its have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conf lict of interest to declare. World Journal of Pediatrics2022年9期
World Journal of Pediatrics2022年9期
- World Journal of Pediatrics的其它文章
- Association between genetic polymorphisms of base excision repair pathway and glioma susceptibility in Chinese children
- Evaluation of proximal tubule functions in children with COVID-19:a prospective analytical study
- Genotypic and phenotypic spectra of NBEA-related neurodevelopmental disorder with epilepsy: a case series and literature review
- Impact of comorbidities on the prognosis of pediatric vasovagal syncope
- Eff ect of early feeding practices and eating behaviors on body composition in primary school children
- Asthma mortality among children and adolescents in China,2008–2018
