Impact of comorbidities on the prognosis of pediatric vasovagal syncope
a-Ru Wang · Xue-Ying Li Y · Jun-Bao Du,3 · Yan Sun · Wen-Rui Xu · Yu-Li Wang · Ying Liao · Hong-Fang Jin
Vasovagal syncope (VVS) is the primary entity of neurally mediated syncope (NMS) in childhood, and its prognosis is usually considered benign. However, it is found in clinical practice that some children with VVS appear to have a frequent recurrence of syncope and poor response to treatment [ 1], which might seriously aff ect their quality of life[ 2]. In recent years, an increasing number of comorbidities of VVS have been reported. Liao et al. found that 31% of pediatric patients with NMS suff ered from allergic disease[ 3], and Vallejo M reported that more than 50% of patients had headaches [ 4]. These comorbidities might make the clinical manifestations even more complex. However, until now, it has been unclear whether comorbidities are associated with the prognosis of children and adolescents suff ering from VVS. Therefore, the present study was conducted to examine whether there is any impact of comorbidities on the prognosis of pediatric VVS to better understand the outcome and management of children and adolescents with VVS.
In this retrospective cohort study, we enrolled pediatric participants aged from 5 to 18 years who entered the Department of Pediatrics at Peking University First Hospital and were diagnosed with VVS from January 2016 to December 2019. The participants were divided into a simple VVS (S-VVS) group and a VVS with comorbidity (Co-VVS) group according to whether they were complicated with comorbidities including migraine, pediatric psychological disorders (including psychosomatic illness,anxiety disorder, sleep disorder, and emotional disorders),hyperventilation syndrome, f ibromyalgia, chronic fatigue syndrome, and allergic disorders, which had been previously reported in patients with VVS [ 3, 5— 11]. Those who were complicated with epilepsy or cardiogenic syncope or had an uncertain diagnosis were excluded. The clinical data, including sex, age at admission, age at onset, body mass index, course of disease before admission, number of syncopal episodes before admission, supine heart rate,supine blood pressure, anemia or not, and treatment measures, were collected from the patients’ hospitalization data recorded by a Beijing Kaihua Medical Recording Management Digital System.
The pediatric VVS was made based on the patients' clinical presentations according to associated guidelines [ 12, 13].The diagnostic standards in Chinese children with VVS were as follows: (1) usually occuring in older children; (2) often with precipitating factors, such as long-term standing, sudden changes from a supine to an upright position, a muggy environment and emotional stress; (3) symptom of syncope;(4) positive response during the head-up tilt test; and (5)the exclusion of other diseases. The data of comorbidities referred to the conf irmed diagnosis at the participants’ discharge and the diagnosis of comorbidities were made by corresponding specialists.
The participants were followed-up since their f irst discharge through a clinic visit or telephone visit by a dedicated investigator. The last follow-up time point was May 2021.The endpoint of this study was the f irst recurrent episode of syncope during the follow-up. Additionally, trauma resulting from syncope, rehospitalization and/or schooling suspension because of recurrent syncope, was also recorded during the follow-up.
A total of 288 children diagnosed with VVS were included in the study, and 61 were excluded. The remaining 227 patients were followed-up, among whom 21 (9.3%) (18 in the S-VVS group and 3 in the Co-VVS group) were lost.The maximum duration of follow-up was 64 months, and the median follow-up time was 26 months.
The 227 enrolled participants (96 males and 131 females)were aged 5—18 years, among whom 142 were in the S-VVS group and 85 were in the Co-VVS group. The proportion of male patients in the Co-VVS group was signif icantly higher than that in the S-VVS group (P
< 0.05). There were no remarkable diff erences in other basic characteristics(Table 1).In total, 37.4% (85/227) of children in the cohort diagnosed with VVS had comorbidities, among whom 33.0%(75/227) had 1 comorbidity, and 4.4% (10/227) had 2 comorbidities (Fig. 1 a). The comorbidities mainly included allergic disorders, psychological disorders, hyperventilation syndrome and migraine. In the Co-VVS group, the top two common comorbidities were allergic disorders (85.9%,73/85) and psychological disorders (14.1%, 12/85) (Fig. 1 b).
As shown in Fig. 2, the cumulative recurrence rate of syncope (CRRS) in the Co-VVS group was meaningfully higher than that in the S-VVS group (log rankP
= 0.0011,HR: 2.287; 95% CI: 1.392—3.757). The median recurrence time was 33 months in the Co-VVS group and > 63 months in the S-VVS group. In addition, the CRRS was 53.2% at the end of the follow-up in the Co-VVS group but was only 33.6% in the S-VVS group.Since there was a remarkable diff erence in the sex ratio between the two groups in the analysis of basic characteristics, further analysis with Kaplan—Meier (K—M) curves was applied to explore the possible inf luence of comorbidities on the prognosis of pediatric VVS in diff erent sex subgroups. There was an obvious diff erence among the four groups (log rankP
= 0.0091). The results of multiple comparisons demonstrated that the CRRS was not diff erent between the S-VVS group and Co-VVS group neither in the male nor the female subgroup (male: log rankP
= 0.0092; female: log rankP
= 0.0299) [P
< 0.0083(0.05/6) was considered statistically signif icant between any two groups within the set of four groups]. In addition,within the Co-VVS group, there was no apparent diff erence in the CRRS between male and female participants(log rankP
= 0.6813).Considering the diff erence in both physical and psychological development between the preadolescent and adolescent participants, we also performed further subgroup analysis to evaluate the possible impact of comorbidities on the prognosis of VVS in children at diff erent age groups using another set of K—M curves. Subgroups of puberty (males between 13 and 18 years old and females between 11 and 18 years old) [ 14] and prepuberty (males before 13 years old and females before 11 years old) were established based on the participants’ age at onset. There was an obvious diff erence among the four groups (log rankP
= 0.0005). However,there was no signif icant diff erence in prognosis between the two groups within prepubescent participants (log rankP
= 0.0266), while CRRS in the Co-VVS group was signif icantly higher than that in the S-VVS group in the puberty subgroup (log rankP
= 0.0027).We further identif ied the impact of comorbidities on the prognosis of VVS in each sex subgroup at diff erent age stages. In the male subgroup, there was no remarkable difference among the four groups (log rankP
= 0.0712). In the female subgroup, there was a remarkable diff erence within the four groups (log rankP
= 0.0039), although no signif icant diff erence in prognosis was found between the two groups in the prepuberty subset (log rankP
= 0.6611);and the CRRS in the Co-VVS group was dramatically higher than that in the S-VVS group in the puberty subset (log rankP
= 0.0042). That is, the adverse inf luence of comorbiditieson the prognosis of pediatric VVS was the most signif icant in the pubertal females.Table 1 Basic clinical features of the S-VVS and Co-VVS groups
Values are expressed as mean ± standard deviation, median (P , P ) or numbers. < 0.05 is considered to be obviously diff erent. body mass index, - simple vasovagal syncope, - vasovagal syncope with comorbidity, beats per minute. a Nonmedication therapy mainly included health education, upright training, or oral rehydration salts. Medication therapy mainly included midodrine or metoprolol on the basis of nonmedication therapy. b Anemia was def ined as hemoglobin < 110 g/L for children < 6 years old and < 120 g/L for children ≥ 6 years old
Items S-VVS group ( N = 142) Co-VVS group ( N = 85) z/ t/ χ 2 P value Sex (male/female) 50/92 46/39 7.788 0.005 Age at admission, y 12.0 (9.0, 13.0) 11.0 (9.0, 13.0) - 1.005 0.315 Age at onset, y 10.0 (7.0, 12.0) 10.0 (7.0, 12.0) - 0.282 0.778 BMI, kg/m 2 18.0 (16.3, 20.9) 18.1 (16.6, 21.0) - 0.359 0.719 Course of disease before admission, mon 12.0 (4.7, 36.0) 12.0 (2.5, 36.0) - 0.284 0.777 Number of syncopal episodes before admission(≥ 5/< 5)43/99 30/55 0.612 0.434 Supine heart rate, bpm 75.0 (68.7, 85.0) 80.0 (74.0, 85.0) - 1.937 0.053 Supine systolic pressure, mmHg 108.0 ± 10.5 106.0 ± 9.6 1.485 0.139 Supine diastolic pressure, mmHg 62.2 ± 8.7 60.7 ± 7.9 1.314 0.190 Treatment (medication/nonmedication) a 74/68 35/50 2.548 0.110 Anemia (yes/no) b 12/130 3/82 1.365 0.243

Fig. 1 The spectrum of comorbidities in pediatric vasovagal syncope. a The proportion of patients in the Co-VVS and S-VVS groups; b The proportion of diseases in the Co-VVS group. S-VVS simple vasovagal syncope, Co-VVS vasovagal syncope with comorbidity
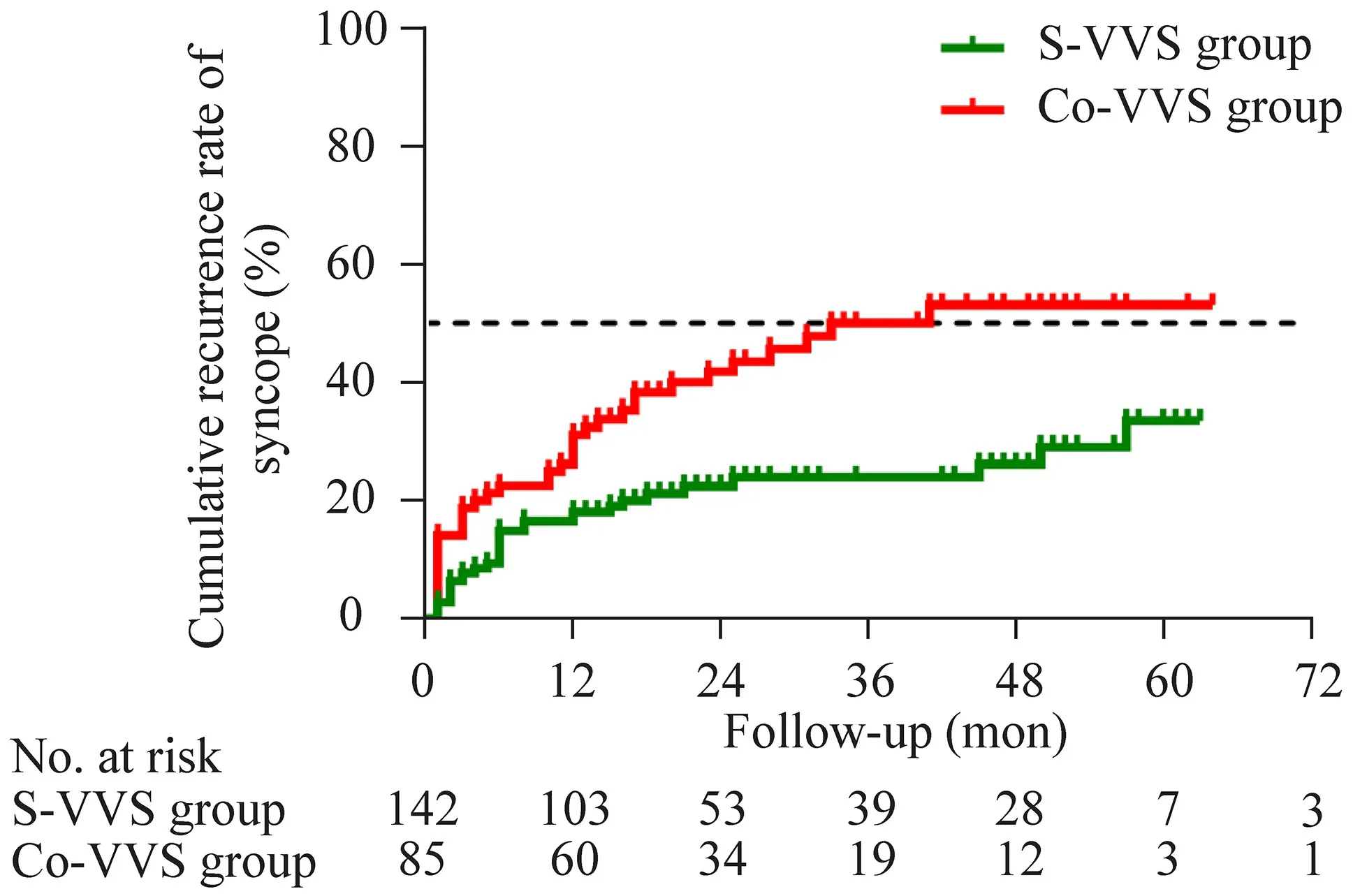
Fig. 2 The cumulative recurrence rate of syncope in the S-VVS and Co-VVS groups. The Kaplan—Meier curves show the cumulative recurrence rate of syncope in the S-VVS group and Co-VVS group during follow-up. The green curve and red curve represent the cumulative recurrence rate of syncope for the S-VVS group and Co-VVS group, respectively. The log rank P of the Kaplan—Meier curves between the two groups is 0.0011. S-VVS simple vasovagal syncope,Co-VVS vasovagal syncope with comorbidity
The total number of events associated with recurrent syncope, such as rehospitalizations, hospital stay, the incidence of inpatient consultations, trauma and schooling suspension,were collected and summarized. Participants in the Co-VVS group had more rehospitalizations and a higher incidence of inpatient consultations than those in the S-VVS group. These diff erences were signif icant (P
< 0.05).We, for the f irst time, show that comorbidities have a negative impact on prognosis, especially for adolescent females,and we described the spectrum of comorbidities in Chinese children with VVS based on data from a single-center analysis. In addition, the comorbidities may increase the diffi culties in the diagnosis and treatment of VVS.
At present, the mechanisms by which comorbidities influence the prognosis of pediatric VVS are not entirely known. It is speculated that comorbidities might directly or indirectly play a part in the pathogenesis of VVS, such as relatively insufficient central blood volume, peripheral vascular dysfunction, and autonomic dysfunction [ 15, 16].For example, allergy-related inflammatory mediators,such as histamines, leukotrienes, and prostaglandins, are known to cause excessive vasodilation or increased vascular permeability, leading to insufficient relative blood volume [ 16] and may theoretically aggravate the clinical manifestations of VVS. Further research is still needed to confirm the potential relationship between comorbidities and VVS.
Further subgroup analysis showed that the inf luence of comorbidities on the prognosis in pediatric VVS was more signif icant in adolescent female patients. We speculated that this distinct diff erence among sex-age subgroups might result from comorbidities, such as poor control of asthma [ 17] and the increased incidence of psychological disorders [ 18].
However, this study also has some limitations. First, the incidence of comorbidities might be underestimated, and the severity of each comorbidity was challenging to evaluate. Second, the above results for the prognosis still need more investigation to conf irm because of the relatively limited numbers of participants, especially in subgroup analysis. In addition, other factors, such as insuffi cient oral intake, menstrual status, and patients’ cardiac evaluation,may also aff ect the outcome of the prognosis; these factors were not included in this study because of the retrospective nature.
Collectively, allergic disorders were the most common comorbidities in Chinese children with VVS. Comorbidities have a negative impact on prognosis of pediatric VVS, especially for adolescent females. Comorbidities may increase the diffi culties in diagnosing and treating children with VVS.Therefore, individualized treatment and prognosis assessments should be made based on sex and the age at onset.Further studies are still needed to clarify the mechanisms by which comorbidities inf luence the prognosis of pediatric VVS.
Acknowledgements
We would like to thank the Department of Pediatrics, Peking University First Hospital and all the researchers who contributed to this paper. In addition, we appreciate the cooperation of parents and patients and the support of the Ethics Committee of Peking University First Hospital for this study.Author contributions
YW: writing-original draft, formal analysis, and data curation; XL: formal analysis, investigation, and methodology;YS, WX and YW: data curation, investigation and project administration; HJ and JD: supervision, project administration, writing-review &editing, and conceptualization; YL: writing-review & editing, validation, and methodology.Funding
This work was supported by the Peking University Clinical Scientist Program (BMU2019LCKXJ001), and the Fundamental Research Funds for the Central Universities, China. Clinical Medicine Plus X - Young Scholars Project (PKU2022LCXQ028), the Fundamental Research Funds for the Central Universities, China. Multicenter Study Project, Peking University First Hospital, China.Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.Declarations
Ethical approval
This study was approved by the Ethics Committee of Peking University First Hospital (2021-095).Conflict of interest
No f inancial or non-f inancial benef its have been received or will be received from any party related directly or indirectly to the subject of this article. Junbao Du is a member of the Editorial Board forWorld Journal of Pediatrics
. The paper was handled by the other Editor and has undergone rigorous peer review process. Junbao Du was not involved in the journal's review of, or decisions related to,this manuscript. World Journal of Pediatrics2022年9期
World Journal of Pediatrics2022年9期
- World Journal of Pediatrics的其它文章
- Association between genetic polymorphisms of base excision repair pathway and glioma susceptibility in Chinese children
- Evaluation of proximal tubule functions in children with COVID-19:a prospective analytical study
- Genotypic and phenotypic spectra of NBEA-related neurodevelopmental disorder with epilepsy: a case series and literature review
- Using echocardiography in newborn screening for congenital heart disease may reduce missed diagnoses
- Eff ect of early feeding practices and eating behaviors on body composition in primary school children
- Asthma mortality among children and adolescents in China,2008–2018
