Development and validation of a nomogram for predicting the risk of pressure injury in adult patients undergoing abdominal surgery
Xue Feng ,Meng Wng ,Y Zhng ,Qin Liu ,Mingyng Guo ,Hongyin Ling ,*
a Department of General Surgery,General Hospital of Western Theater Command (Chengdu Military General Hospital),Chengdu,China
b Department of Traditional Chinese Medicine,General Hospital of Western Theater Command (Chengdu Military General Hospital),Chengdu,China
Keywords:Adult Nomogram Patients Pressure ulcer Surgical procedures
ABSTRACT Objectives: This study aimed to develop a nomogram for predicting the risk of pressure injury (PI) in adult patients undergoing abdominal surgery and validate its effectiveness among these patients.Methods:This study retrospectively included 11,247 adult patients,who underwent abdominal surgery and postoperative supervision in ICU,in a tertiary care hospital in western China between January 2017 and December 2020.All datasets were extracted from the patient’s medical records and randomly divided into the training cohort(8,997)and the validation cohort(2,250)by 8:2.The univariable logistic regression was used to select potentially relevant features.Then,multivariable logistic regression was also conducted and utilized to establish the nomogram.The nomogram was compared with the Braden scale for predicting PI in the validation cohort through the area under the curve (AUC) of the receiver operator characteristic (ROC) curve,Hosmer-Lemeshow (H-L) test,and decision curve analysis (DCA).Results:873 (7.8%) patients suffered PIs.Logistic regression analysis showed that time of operation,weight,type of operation,albumin,and Braden scale score were independent risk factors for PI.A nomogram integrating five selected characteristics was constructed.The AUC of the ROC curve for the nomogram was 0.831,with a specificity of 85.2% and sensitivity of 63.7%.The AUC of the ROC curve for the Braden scale was 0.567,with a specificity of only 33.0%.The P-values of the H-L test were 0.45(nomogram) and 0.22 (Braden scale),both indicating good calibration.The DCA also displayed that the nomogram had better predictive validity.Conclusion:Compared with the Braden scale,the nomogram showed a better predictive performance.This nomogram is informative and has the potential to better guide caregivers for risk stratification and prevention of PI,although it requires further validation.
What is known?
· Patients undergoing surgery are at high risk of pressure injury(PI).
· Early structured risk assessment of patients can be effective in reducing the incidence of PI;but few tools can accurately assess the risk of PI in patients undergoing abdominal surgery.
· The nomograms have been recognized as a reliable method to evaluate the risk of clinical events recently.
What is new?
· In this study,we developed a nomogram and validated its effectiveness for predicting PI among patients undergoing abdominal surgery.
· The nomogram showed a better predictive performance compared with the Braden scale.
1.Introduction
Pressure injury (PI) is also known as pressure ulcer or pressure sore.In 2016,the National Pressure Ulcer Advisory Panel (NPUAP)defined it as localized damage to the skin and underlying soft tissue that is usually over a bony prominence or related to medical or other devices.The incidence of PI is not only an important indicator for evaluating the quality of care but also is closely associated with the prognosis of patients [1].In patients who incurred a PI,the length of stay was significantly prolonged [2].It has also been reported that PI may increase the mortality in critically ill people by approximately 4-fold[3].The occurrence of PI brings suffering and the threat of death to patients,increases the socioeconomic burden,and poses a tremendous burden on nursing care [4].PI has been reported to be the third most costly item after cancer and heart disease [5].
Patients undergoing surgery are at high risk of PI.In a Dutch hospital,the prevalence of PI was 13.2%,of which 39.1%of patients had undergone surgery [6].Other studies have shown a 12.7%incidence of intraoperative PI in the operating room of an Italian hospital[7].Patients undergoing surgery are unable to relieve local tissue pressure by frequently changing the surgical position intraoperatively [8].Meanwhile,patients who undergo surgery often need to be admitted to the ICU for postoperative care[9].These may be risk factors for the incidence of PI.
In a 2014 consensus,the NPUAP suggested that early structured risk assessment of patients with a valid and reliable risk assessment tool can be effective in reducing the incidence of PI [10].Since the 1960s,more than 30 risk assessment tools for PI have been designed,including the Lothian,Mdeley,Waterlow,Norton,and Braden scales[11].However,it was found that the predictive effect of the risk of PI was not favorable,even though the commonly used assessment scales of Waterlow,Norton,and Braden were used.In a meta-analysis of the Braden scale,it was shown to have moderate predictive validity and good sensitivity but low specificity in adults with severe disease [12].The Munro scale for surgical patients is more comprehensive and more sensitive than the Braden scale,but the Munro scale requires a longer assessment time and needs to be evaluated together with the anesthesiologist and surgeon.Additionally,some individual items in the Munro scale are not routinely measured[13].These results reveal that there is a need to develop or generate a novel tool with a higher predictive effect for the risk of PI.
Currently,there have been a few advances in the assessment of PI with some new assessment tools.The first one is the model constructed via machine learning or deep learning.Far more sophisticated methods and larger data can be leveraged right now,resulting in more accurate and precise predictive models than ever before.PI assessment based on machine learning or deep learning has shown some advantages over traditional tools.In a recent study,electronic health record (EHR) data from 50,851 individuals in the Medical Information Mart for Intensive Care (MIMIC) III database were utilized for machine learning to assess the incidence of PI in the ICU [14].This study found that a machine learning model based on EHR data could be superior to the Braden score as a screening tool for PI.In another study,supervised machine learning based on health data collected on the first day of patient admission showed that the model has the potential to identify patients at high risk for developing PI [15].Nevertheless,the sophistication of the model makes it difficult to comprehend and discourages clinicians from applying the model in practice.
Nomograms,one of the methods commonly used in risk prediction models,have been recognized as a reliable tool,with the advantages of being intuitive and convenient,to evaluate the risk of clinical events by creating a visual statistical predictive graph[16].They provide a more practical explanation of the impact of each predictor variable on the results,showing dynamic vigor in today’s digital era.In a recent study,a nomogram for predicting PI was developed using clinical data from the MIMIC IV database.The results of this study showed that the nomogram had better specificity and sensitivity than the Braden score for assessing the risk of PI in critically ill patients admitted to the ICU[17].A Chinese study of nomograms for predicting PI in the ICU based on hospital EHR data also showed similar results[18].Notably,in this study,surgical suffering was considered an independent risk factor for the incidence of PI.However,none of these studies further analyzed risk factors for the incidence of PI in surgical patients.
In this study,we developed and validated a nomogram for predicting the risk of PI in patients undergoing abdominal surgery.With the assistance of the nomogram,the health care team can make more rational clinical decisions and improve the quality of care.
2.Methods
2.1.Study design
This is a retrospective cohort study.The electronic medical records (EMRs) of patients undergoing abdominal surgery in a tertiary hospital in western China were reviewed.The inclusion criteria included 1)having undergone abdominal surgery between January 2017 and December 2020 and 2) having undergone postoperative supervision in the ICU.The exclusion criteria were 1)the patient had not reached the age of 18 years or 2)the patient did not have a complete medical history.This study follows the Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD).
2.2.Data collection
The clinical data,scale scores,and relevant laboratory test results of eligible patients were extracted from EHR data and medical records by two independent investigators.The inconsistencies were checked and corrected by two investigators and a third investigator after retrieving the data.The purpose of the study was not clear to the investigators when collecting the data.
Based on consultation with clinical experts,reviewing of the relevant literature,and the information we were able to collect,we only included the following relevant complete clinical information on the patients: age,sex,height,weight,history of smoking,drinking,hypertension,heart disease,diabetes,and recent steroid administration.Preoperative laboratory results,including hemoglobin (HB),white blood cell (WBC) count,platelet (PLT) count,serum calcium (Ca),serum total protein (TP),and serum albumin(Alb),were adopted from the patient’s last preoperative examination.The time of operation,type of operation (laparotomy or laparoscopy),preoperative American Society of Anesthesiologists(ASA) score,emergency surgery,estimated blood loss (EBL),and duration of intraoperative hypotension were extracted from the surgical records.The preoperative nutrition risk screening (NRS)score,Braden scale score,administration of ventilation,vasoactive drugs,sedation,and incidence of PI were also extracted from medical records.
The incidence and stages of PI are identified according to the NPUAP revised guidelines[19].Preoperative ASA,NRS,and Braden scores were measured by the supervising physician according to the ASA physical status classification [20],guidelines for nutrition screening 2002 [21],and the Braden risk assessment scale [22],respectively.
2.3.Statistical analysis
Continuous variables are expressed as the means and standard deviations (SDs),while categorical variables are expressed as frequencies and percentages.The t-test or analysis of variance(ANOVA) was used to compare differences between continuous variables.The χ2test was used to compare differences between categorical variables.P values <0.05 were considered statistically significant.All statistical analyses were performed using SPSS software (version 22.0,SPSS,Inc.,Chicago,Illinois,USA) and R software (version 4.1.3 for Windows,Bell Laboratories).
In this study,patients with PI occurring from postoperative to pre-discharge periods were included in the PI group,and patients without PI occurring were included in the non-PI group.And all datasets were randomly divided into training and validation cohorts according to a ratio of 8:2 through the R software [23].The training cohort was adopted for correlation analysis through univariate analysis and multivariable Logistic regression analysis.Based on the filtered-out risk factors,a nomogram was constructed with the R software.The validation cohort was used to validate and compare the predictive efficacy of the nomogram,compared with the conventional Braden scale,for the risk of PI.Before using the external validation cohort,the nomogram underwent 1,000 bootstrap internal validations in the training cohort.
Braden scale is commonly applied to the prediction of PI.Studies are recommending that 18 can be used as a threshold value for Braden scale to predict the occurrence of PI [24].In this study,we used the score of Braden scale <18 as a predictive metric for PI and compared its predictive performance with the nomogram.Receiver operator characteristic (ROC) curves (for Discrimination),Hosmer-Lemeshow (H-L) test (for Calibration),and decision curve analysis(DCA) were used to evaluate the effects of the prediction,which were also conducted with R software [25].
2.4.Ethical considerations
This study was approved by the Ethics Committee of the General Hospital of Western Theater Command(2022ky57).The procedures involved in collecting information from patients were conducted by the code of ethics of the World Medical Association(Declaration of Helsinki).
3.Result
3.1.Patient characteristics
In this hospital,the department of abdominal surgery has 6 wards.As a separate ward,ICU has 26 beds.The average length of stay in the ICU is about 2.51 days,and the bed occupancy rate is about 75%in our hospital.During the study period,11,247 patients who met the inclusion and exclusion criteria were included in the study.Of these patients,5,618(49.9%)of them were male,and 5,629(50.1%) of them were female,with an average age of 45.1 ± 10.9 years.A total of 873 patients (7.8%) suffered a PI during hospitalization.A total of 725 patients (83.1%) had a PI of stage I or II,139 patients(15.9%)had a PI of stage III or IV,and 9 patients(1.0%)had a PI that was difficult to grade.The patients included were randomly divided into a training cohort (n=8,997) and a validation cohort(n=2,250).The baseline demographics and characteristics of the patients are summarized in Table 1.
3.2.Correlation analysis
The patients were divided into a PI group and a non-PI group according to whether PI occurred.Weight,recent steroid administration,Alb,NRS >3,time of operation,type of operation,and Braden scale score were significantly (P <0.05) identified in univariate analysis in the training cohort (Table 2).
The above factors with significant differences were substituted into the multivariate logistic regression analysis (Table 3).The multivariable analysis showed that time of operation (P <0.001),weight (P <0.001),type of operation (P <0.001),Alb (P <0.001),and Braden scale score (P <0.001) were independent risk factors for PI,which were included in the nomogram.
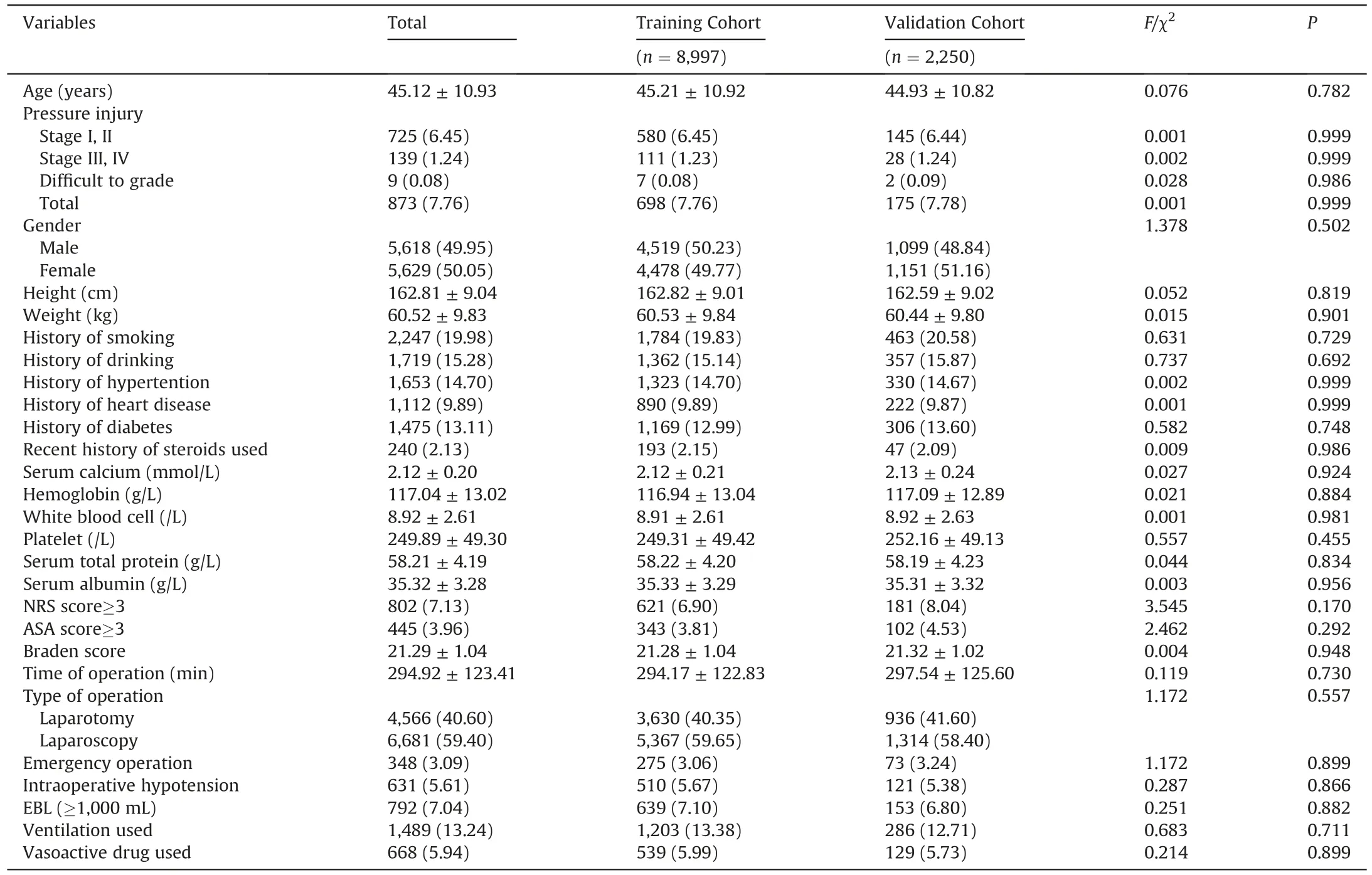
Table 1Baseline demographics and characteristics of the patients (n=11,247).
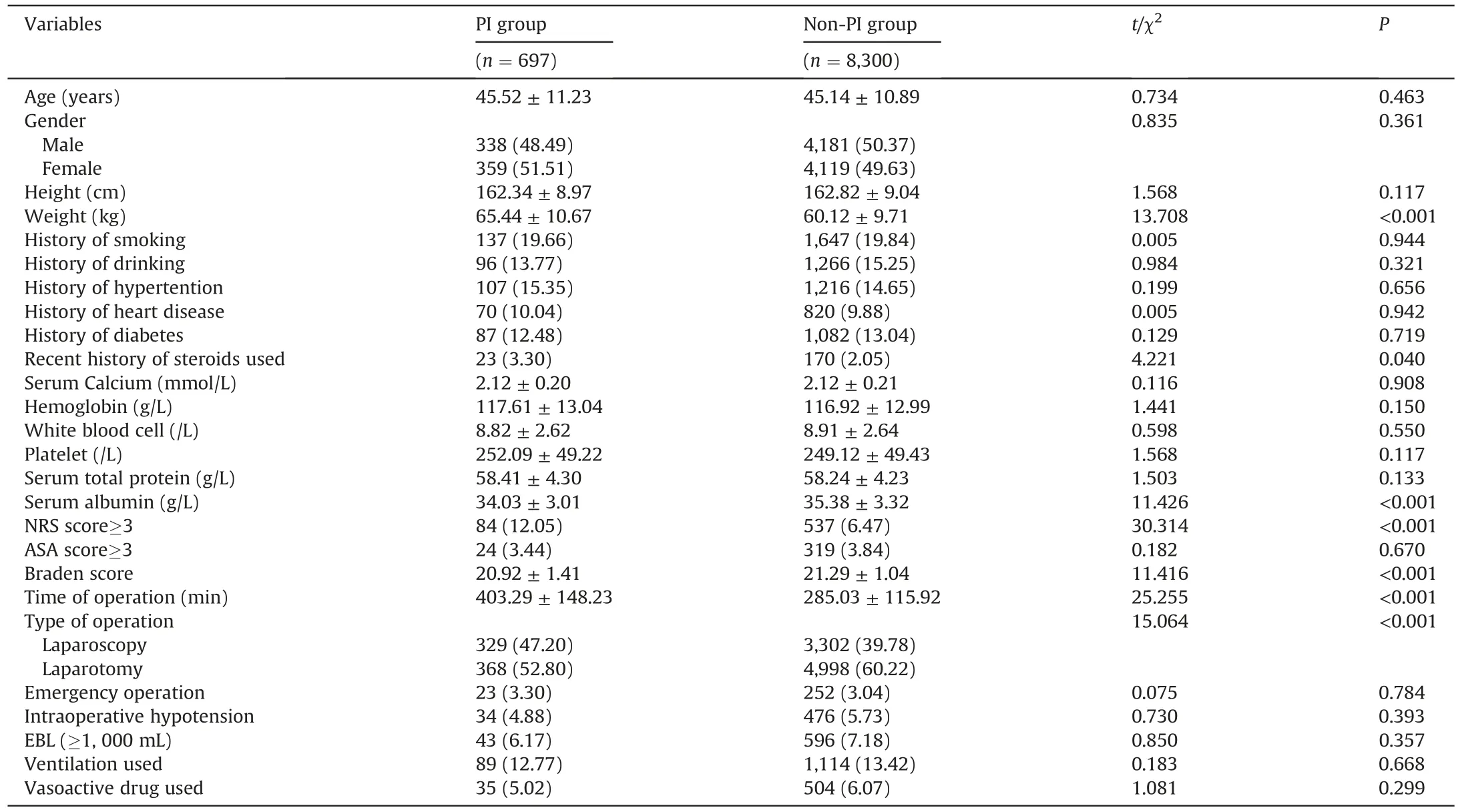
Table 2Clinical characteristics of the patients in the training cohort.
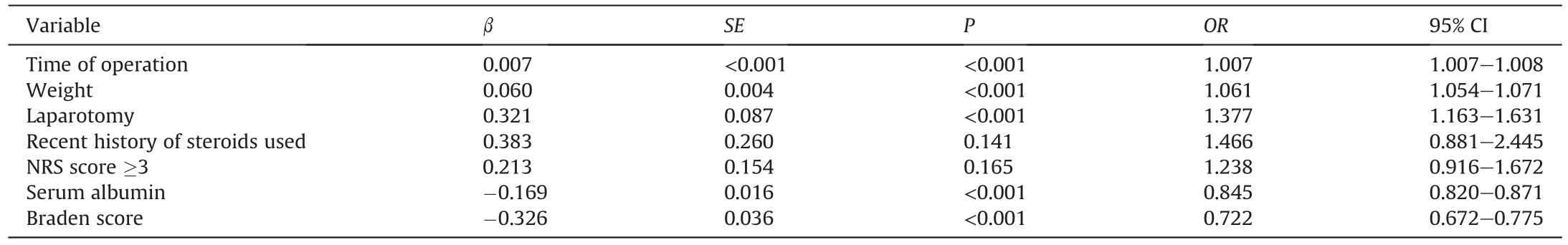
Table 3Risk factors associated with pressure injuries using multivariate logistic regression analysis.
3.3.Construction of the nomogram
A nomogram integrating five selected characteristics of PI in the training cohort (P <0.05) is shown in Fig.1.The value of each risk factor is assigned a score on the point scale axis.The probability of PI occurrence can be easily converted by summing each score and using that value in the total point axis.
3.4.Validation of the nomogram
The model was well-differentiated by using an internal training cohort and an external validation cohort for validation.In the internal validation(Fig.2A),the AUC of the ROC curve for the Braden scale was 0.573,with a specificity of 32.9%and sensitivity of 86.2%.The AUC of the ROC curve for the nomogram was 0.810,with a specificity of 70.7% and sensitivity of 78.7%.In external validation(Fig.2B),the AUC of the ROC curve for the Braden scale was 0.567,with a specificity of 33.0% and sensitivity of 86.7%.The AUC of the ROC curve for the nomogram was 0.831,with a specificity of 85.2%and sensitivity of 63.7%.The P values of the H-L test were 0.45(nomogram) and 0.22 (Braden scale),both indicating good calibration.
The DCA(Fig.3)also showed intuitively that the nomogram had excellent overall net benefits over a wide and practical range of threshold probabilities compared with the Braden scale,which suggests that the constructed nomogram has better prediction effectiveness.
4.Discussion
To our knowledge,this is the first study to predict the risk of PI in adult patients undergoing abdominal surgery utilizing a nomogram.In this study,we analyzed the common factors potentially contributing to the occurrence of PI and finally selected five independent risk factors,which were used for the development of the nomogram.The developed nomogram was compared with the conventional Braden score for predicting the risk of PI.In this study,we found that the Braden scale did not demonstrate a good predictive effect for patients following abdominal surgery.In the validation cohort,the AUC of the ROC curve for the Braden scale was 0.567,with a specificity of only 33.0%.In contrast,the nomogram developed showed a better performance in prediction.In the validation cohort,the AUC of the ROC curve for the nomogram was 0.831,with a specificity of 80.1%and sensitivity of 68.8%.In DCA,the nomogram also showed relatively good predictive validity.
The results of this study showed that both the time of surgery and the surgical procedure affected the occurrence of PI in patients,which were consistent with previous studies.Compared to nonsurgical patients admitted to the ICU,surgical patients may have some specific risk factors for the incidence of PI [26].For instance,in a study of PI in patients undergoing neurosurgery,it was found that being overweight and having a longer surgical time was strongly associated with the occurrence of PI[27].In another study about risk factors for PI in patients undergoing hepatobiliary surgery,prolonged operative time,open surgery,and intraoperative hypotension were found to be associated with an increased incidence of PI [28].Tang recently performed a study regarding risk prediction models for PI in patients transferred to the ICU after surgery [29].This study found that factors such as high preoperative fasting glucose,emergency surgery,type of vasoactive drug,and time of surgery were associated with the development of PI.However,their risk prediction model is not described in detail intheir study,which does not facilitate the replication of this research and its further dissemination.
In this study,age was not significantly associated with the occurrence of PI.With age,the epidermis and dermis become atrophied and thin,the elastic fibers lose elasticity,and the tissue recovery function become poor.In some studies,age has been suggested to have a possible relationship with the occurrence of PI[30].Such inconsistency is probably explained by the different study populations in the different studies.Patients who underwent surgery tended to be younger than those with some chronic diseases.Furthermore,in some studies of PI in surgical patients,age was not found to be the most important factor contributing to PI.
The nomogram has easy-to-use features.The predicted risk probability can not only be calculated automatically using computer software but also can be very easily calculated manually using nomogram charts (Fig.1).The values of clinical indicators can be converted into corresponding scores and the total score can be utilized to predict probability with a simple conversion.This is very beneficial to caregivers in the clinical setting for risk stratification and prevention of PI.Furthermore,our results showed that time of operation,weight,type of operation,Alb,and Braden scale score were independent risk factors for PI.We can screen for patients at high risk of PI by using the nomogram.Reduced operative time,appropriate use of the open surgical approach,and increased perioperative nutritional support may have a positive impact on high-risk patients’ prognosis.
However,there are a few limitations to this study.First,there is still an upper limit to the validity of the prediction model used,although the nomogram showed better prediction than the traditional Braden scale in this study.The nomogram is usually constructed by relying on the results of logistic or Cox regression analysis.However,logistic or Cox regression analysis is a linear model.It is possible to have a bias when there is no linear relationship between risk factors,which may occur in real situations.In this respect,models constructed by deep learning or machine learning have a natural advantage.Of course,these models are too obscure and difficult to understand to facilitate practical use in clinical work,especially in less privileged primary care settings.Second,this study is still a retrospective study,which has a lower level of evidence.The results should be validated in further prospective trials.
5.Conclusion
In summary,this is the study to predict the risk of PI in adult patients undergoing abdominal surgery utilizing a nomogram.Time of operation,weight,type of operation,Alb,and Braden scale score were included in the development of the nomogram.Compared with the conventional Braden score,the nomogram developed showed a better performance in prediction.This is an encouraging finding,and the newly developed nomogram has the potential to better guide caregivers in the clinical setting for risk stratification and prevention of PI,although it requires further validation.
Fig.1.Nomogram based on the probability of pressure injury using the multivariate logistic regression model.OpTime=time of operation,OpType: 1=laparotomy,0=laparoscopy,Alb=albumin.
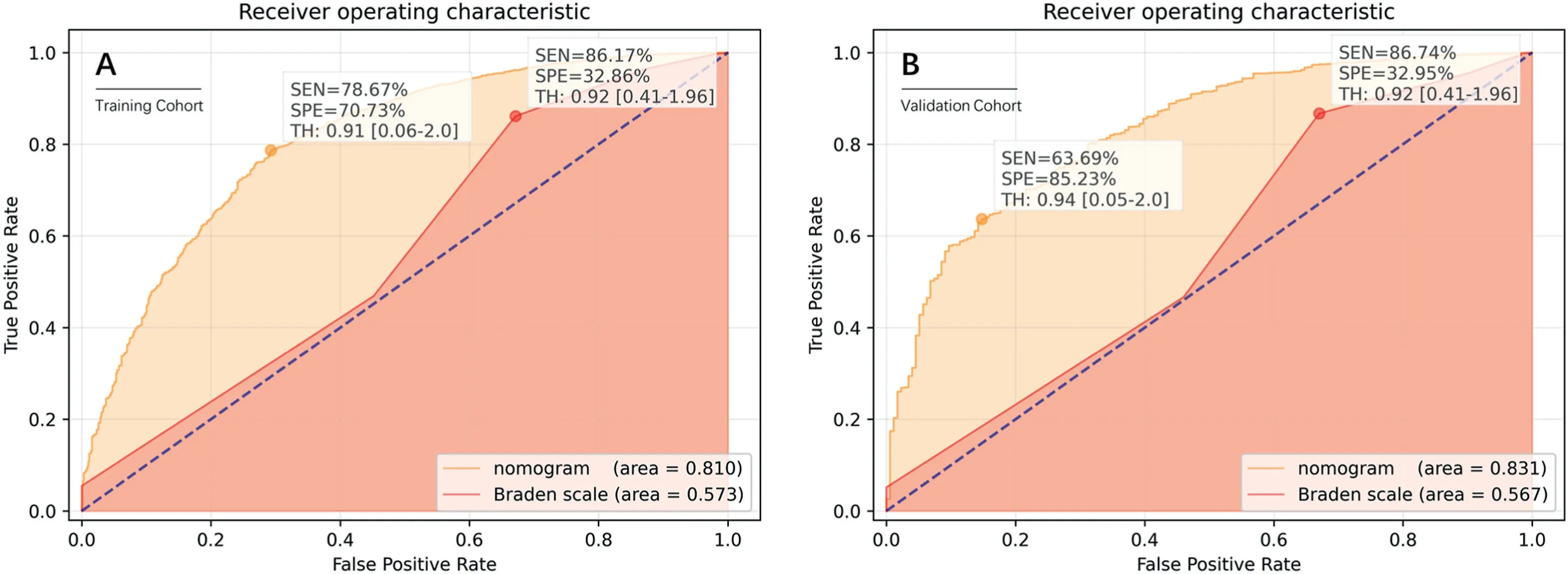
Fig.2.Receiver operator characteristic(ROC)curve of nomogram and Braden scale for the probability of pressure injury.(A)ROC curve in the training cohort;(B)ROC curve in the validation cohort.The area under the curve (AUC) of the ROC curve is calculated,which indicates the accuracy and specificity of the method.
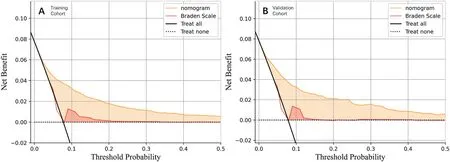
Fig.3.Decision curve analysis(DCA)of nomogram and Braden scale for the probability of pressure injury.(A)DCA in the training cohort;(B)DCA in the validation cohort.Treat all and Treat none curves represent two extreme conditions.A greater distance from these two curves implies a higher net benefit.
CRediT authorship contribution statement
Xue Feng:Formal analysis,Investigation,Writing -original draft.Meng Wang:Formal analysis,Investigation,Writing -original draft.Ya Zhang:Investigation,Data curation.Qian Liu:Investigation,Data curation.Mingyang Guo:Data curation,Methodology.Hongyin Liang:Writing -investigation,Review &editing,Supervision,Software.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We would also like to express our gratitude to the Dr.Xiaodong Xie(General Hospital of Western Theater Command)for his advice on this study.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.09.010.
 International Journal of Nursing Sciences2022年4期
International Journal of Nursing Sciences2022年4期
- International Journal of Nursing Sciences的其它文章
- Effects of equine-assisted interventions on older adults’ health: A systematic review
- Multicenter application of a nursing workload measurement scale in adult hospitalization units
- Exploring social movement concepts and actions in a knowledge uptake and sustainability context: A concept analysis
- Palliative care needs and symptom burden in younger and older patients with end-stage renal disease undergoing maintenance hemodialysis: A cross-sectional study
- Lived experiences with unmet supportive care needs in pediatric cancer: Perspective of Chinese children and their parents
- Factors influencing the optimal selection of central venous access devices: A qualitative study of health care team members’perspectives
