Can physical activity eliminate the mortality risk associated with poor sleep?A 15-year follow-up of 341,248 MJ Cohort participants
Li-Jung Chn,Mrk Hmr,Yun-Ju Li,c,d,Bo-Hui Hung,Po-Wn Ku,Emmnul Stmtkis,#
a Department of Exercise Health Science,(National)Taiwan University of Sport,Taichung 40404,China
b Institute of Sport Exercise and Health,Division of Surgery and Interventional Science,Faculty of Medical Sciences,University College London,London,WC1E 6BT,UK
c Division of Endocrinology and Metabolism,Department of Internal Medicine,Puli Branch of Taichung Veterans General Hospital,Nantou 54552,China
d School of Medicine,(National)Yang-Ming University,Taipei 11221,China
e Charles Perkins Centre,School of Health Sciences,Faculty of Medicine and Health,University of Sydney,Sydney,NSW 2006,Australia
f Graduate Institute of Sports and Health,(National)Changhua University of Education,Changhua 50007,China
g Department of Kinesiology,(National)Tsing Hua University,Hsinchu 30013,China
Abstract Background:This study examined the joint associations of sleep patterns and physical activity(PA)with all-cause,cardiovascular disease(CVD),and cancer mortality.Methods:A total of 341,248 adults(mean age=39.7 years;men:48.3%)were included in the study,with a 15-year follow-up.Participants reported sleep duration and disturbances(difficulty falling asleep,easily awakened,or use of sleeping medication).PA was classified into 4 levels:<7.5,7.5-14.9,15.0-29.9,and≥30.0 metabolic equivalent hours per week(MET-h/week).To understand the joint associations of sleep patterns and PA with mortality,Cox proportional hazard models were conducted,with exposure variables combining sleep duration/disturbances and PA.Results:Compared with the reference group(sleeping 6-8 h/day),individuals who slept>8 h/day had higher risk for all-cause mortality(hazard ratio(HR)=1.307,95%confidence interval(95%CI):1.248-1.369),CVD mortality(HR=1.298,95%CI:1.165-1.445),and cancer mortality(HR=1.128,95%CI:1.042-1.220).Short sleep duration was not associated with mortality risk.Increased risk of all-cause and CVD mortality was found in participants who had difficulty falling asleep(HR=1.120,95%CI:1.068-1.175;HR=1.163,95%CI:1.038-1.304,respectively),and used sleeping medication(HR=1.261,95%CI:1.159-1.372;HR=1.335,95%CI:1.102-1.618,respectively)compared with those who slept well.Long sleep duration and sleep disturbances were not associated with risk of all-cause and CVD mortality among individuals achieving a PA level of≥15 MET-h/week,and in particular among those achieving≥30 MET-h/week.Conclusion:Long sleep duration,difficulty falling asleep,and use of sleeping medication were related to a higher risk of death.Being physically active at a moderate intensity for 25-65 min/day eliminated these detrimental associations.
Keywords:Exercise;Heart disease;Inactivity;Insomnia;Sleep disorders
1.Introduction
Research has shown that more than a third(34.8%)of American adults(n=444,306)do not get the recommended amount of sleep per day(7 h/day),1and 24% of the participants in a 10-country survey(n=35,327)reported sleep disturbances.2Sleep disturbances have been linked to adverse physical and mental health outcomes,such as cardiovascular disease(CVD),depression,and anxiety.3,4Both short and long sleep duration have been associated with increased risk of all-cause mortality and CVD events.5-8In addition to sleep duration,difficulty falling asleep has been related to increased risk of all-cause and CVD mortality,whereas the association of other sleep disturbances(e.g.,difficulty maintaining sleep and early-morning awakening)with the risk of death is less clear.9
Physical activity(PA)is important for preventing several chronic diseases and improving psychological well-being.10,11It has also been well-established in providing protective links against cause-specific and overall mortality.12-15
Sleep and PA are essential health behaviors that occupy the same 24-h cycle.PA seems to affect sleep patterns,16-18and it may also mitigate the adverse effects of poor sleep patterns,such as impaired glucose regulation,19dyslipidemia,hypertension,20and chronic pain.21If increased PA levels are beneficial for extending disease-free survival in those who have poor sleep patterns,interventions that address both behaviors may be valuable.
This study aimed to explore the joint associations between sleep duration and disturbances and PA in relation to mortality risk.We examined whether the associations between poor sleep patterns and all-cause,CVD,and cancer mortality were attenuated or eliminated by PA.
2.Methods
2.1.Study population
Participants were from the MJ Cohort,which was established by the MJ Health Management Institution.The study was based on a large cohort of the general population undergoing a check-up program and included more than half a million Chinese in Taiwan,China since 1996.Participants or their employers paid for these routine health examinations.All participants provided informed consent authorizing MJ Health Management Institution to process the data generated from medical screening.22Each participant completed a self-administered questionnaire,anthropometric measurements,physical examination,and blood and urinary tests at the time of the health check-ups.These check-ups have included questions about sleep since 1996,23and the sleep questions were modified after 2009.The entire current MJ Cohort data includes 615,350 individuals who participated from 1996 to 2017 and were between the ages of 2 and 119 years old.In our study,individuals who were 18 years old or above and participated in the cohort between 1998 and 2008 were selected(n=342,284)since several lifestyle questions(e.g.,smoking,alcohol consumption,sleep,and exercise)were more consistent during this period.To minimize the chance of reverse causality,we excluded participants who died within the first 2 years of follow-up(n=1036).Our study was approved by the(National)Changhua University of Education Research Ethics Committee,Taiwan,China(NCUEREC-108-072).
2.2.Data collection
2.2.1.Measures of sleep patterns
Participants were asked 2 questions concerning sleep patterns.One was related to sleep duration“How long do you sleep per day?”,and 4 response categories were provided(<4 h,4 to<6 h,6 to 8 h,and>8 h).Since only 1%of participants slept less than 4 h,the categories of<4 h and 4 to<6 h were combined for further analyses.The other question asked about sleep disturbances“How have you slept in the past month?”,and 5 response categories were offered(difficulty falling asleep,easily awakened,frequent dreaming,use of sleeping medication,and slept well).23,24Dreaming can be positively or negatively associated with health depending on the dream content25and thus may not reflect sleep disturbances.Therefore,those who reported“frequent dreaming”were excluded for sleep disturbances analyses.Those who reported“slept well”served as the reference group.
2.2.2.PA
Information a bout leisure time PA was collected by selfcompleted questionnaire,which has been described in detail elsewhere.22,26,27Individuals were asked:“What kind of exercise do you usually do?”,with multiple responses possible.Respondents were given several examples of activity types under 4 intensity categories,with a“yes”or“no”answer possible:light(e.g.,gardening,golf),moderate(e.g.,brisk walking,table tennis),medium vigorous(e.g.,jogging,climbing the stairs),and very vigorous(e.g.,running,rope skipping).Then they were asked to report how often and how much time they participated in these activities.The questionnaire has been shown to have acceptable convergent validity through its association with established outcomes,including mortality,diabetes,and systemic inflammation.26,28,29Using established methods,27,28we calculated the metabolic equivalent hours per week(MET-h/week)of PA as the intensity(2.5 METs for light,4.5 METs for moderate,6.5 METs for vigorous,and 8.5 METs for very vigorous)multiplied by frequency and duration.Participants were classified into 4 levels ranging from low to high(<7.5 MET-h/week,7.5-14.9 MET-h/week,15.0-29.9 MET-h/week,and≥30.0 MET-h/week,respectively).A 7.5 MET-h/week classification is roughly equivalent to the minimum recommended amount of PA(3 METs×2.5 h/week),30and 30 MET-h/week represents 50-65 min of moderate-intensity(4-5 METs)activity per day.31
2.2.3.Ascertainment of all-cause,CVD,and cancer mortality
The mortality data were obtained through linkage with the Chinese cause-of-death register,which records the date of death and the underlying cause of death with the International Classification of Diseases,Tenth Revision;these codes were used to identify CVD mortality(I01-I02,I05-I09,I10-I15,I20-I25,I27,I30-I52,I60-I69,I70,and I71)and cancer mortality(C00-C97).
2.2.4.Possible confounding factors
We selected covariates a priori based on previous literature:age,sex,education(<10 years,10-12 years,and≥13 years),marital status(single,married,and other—divorced/separated/widowed),smoking(never,former,and current),alcohol consumption(none/occasional,former,and at least once per week),fruit and vegetable intake(as a marker of dietary quality),and physical health status.Total fruit and vegetable intake(portions/day)was the sum of the intake of fruits and deep-and light-green vegetables.32The Charlson comorbidity index(none=0,mild=1,and severe=2+)was used to reflect physical health status.33The Charlson index is based on the number and self-reported severity of chronic diseases an individual has,including hypertension,heart disease,stroke,diabetes,cancer,chronic obstructive pulmonary disease,liver disease,and renal disease,34,35and has been found to be associated with mortality.33Weight and height were measured,and body mass index(BMI)was calculated as weight in kilograms divided by the square of height in meters.We used the Asianspecific cut-points for underweight,overweight,and obesity BMI of<18.5 kg/m2,24 to<27 kg/m2,and≥27 kg/m2,respectively).The participants’normal range of BMI36was 18.5 to<24 kg/m2.
2.3.Data analyses
Cox proportional hazard models were used to examine the association between sleep patterns and the risk of all-cause,CVD,and cancer mortality.The models were adjusted for PA and the other potential confounders mentioned above.The proportional hazards assumptions were examined using Kaplan-Meier curves.Time at entry was the date of recruitment.Censorship was December 31,2017,or the date of death,if earlier.To understand the joint association of sleep patterns and PA with mortality,we developed additional Cox proportional hazard models,with exposure variables that combined sleep(duration/disturbances)and PA levels,as in previous studies examining the joint effects of PA and sedentary behavior31,37or alcohol intake.38We derived 2 joint variables:(a)a variable combining sleep duration and PA levels of 12 groups,where the group that slept 6-8 h/day and had the highest PA level(≥30 MET-h/week)served as the reference group and(b)a variable combining sleep disturbances and PA levels of 16 groups,where the group having the highest PA level and the absence of sleep disturbances(“slept well”)served as the reference group.
Our analyses did not adjust for clinical sleeping disorders(e.g.,sleep apnea)and mental health due to the absence of such data in the MJ Cohort.To evaluate the robustness of our results and reduce the possibility of spurious associations due to residual confounding,we conducted a set of sensitivity analyses where we excluded(a)those who were obese(as a proxy of sleep apnea)and(b)those who used psychiatric medications(as a proxy of mental disorders).
The level of significance was set at 0.05 for all statistical analyses,which were performed with SPSS Version 22.0(IBM Corp.,Armonk,NY,USA).
3.Results
Among the 341,248 participants entered in the core analyses,there were 21,893 all-cause deaths(3845 from CVD and 8386 from cancer),with a mean follow-up of 15.0±3.4 years(mean±SD).Table 1 shows the characteristics of the participants by sleep patterns.Characteristics of participants with mortality for various groups of PA levels and sleep patterns are presented in Supplementary Table 1.Participants had a mean age of 39.7±13.4 years.The majority of the participants(70.0%)slept 6-8 h/day,21.1% slept less than 6 h/day,and 8.9% reported long sleep duration(>8 h/day).Nearly three-quarters of the participants(73.5%)engaged in PA less than the recommended amount(7.5 MET-h/week),and 15.0% reported a PA level equal to the upper recommendation(≥15.0 MET-h/week).
The association of sleep patterns and PA with all-cause,CVD,and cancer mortality are shown in Table 2.For reference,Supplementary Table 2 presents the Cox model results for all covariates entered in the model.Compared with the reference group(sleeping 6-8 h/day),individuals who slept>8 h/day had a higher risk for all-cause mortality(hazard ratio(HR)=1.307,95% confidence interval(95%CI):1.248-1.369),CVD mortality(HR=1.298,95%CI:1.165-1.445),and cancer mortality(HR=1.128,95%CI:1.042-1.220).We found no association between short sleep duration(<6 h/day)and the 3 mortality end-points.Increased risk of all-cause and CVD mortality were found in participants who had difficulty falling asleep(HR=1.120,95%CI:1.068-1.175;HR=1.163,95%CI:1.038-1.304,respectively)and who used sleeping medication(HR=1.261,95%CI:1.159-1.372;HR=1.335,95%CI:1.102-1.618,respectively)compared with those who slept well.
We observed an increased risk of all-cause and CVD mortality with lower levels of PA.Compared with individuals reporting high PA(≥30.0 MET-h/week),all-cause mortality rates were higher in the 2 least active groups(<7.5 MET-h/week:HR=1.243,95%CI=1.165-1.327;and 7.5-14.9 MET-h/week:HR=1.138,95%CI:1.060-1.223).Low PA was also related to high risk of CVD mortality(<7.5 MET-h/week:HR=1.340,95%CI:1.147-1.565).No association was found between PA and cancer mortality.
When combining sleep duration with PA levels(reference group:6-8 h of sleep/day and≥30.0 MET-h/week of PA),we observed attenuated or eliminated risk for all-cause and CVD mortality in the top 2 PA groups(≥15.0 MET-h/week)(Fig.1A-B,Supplementary Table 3 for numerical results).In the 2 least physically active groups(<15.0 MET-h/week),all sleep duration groups were associated with elevated mortality risk,except the group that slept<6 h/day and had 7.5-14.9 MET-h/week of PA,where the 95%CIs marginally crossed unity for CVD mortality(HR=1.236,95%CI:0.982-1.557,p=0.071).Those sleeping>8 h/day and having<7.5 MET-h/week of PA had the highest all-cause mortality risk(HR=1.555,95%CI:1.428-1.693)and CVD mortality risk(HR=1.783,95%CI:1.453-2.189)compared to the reference group(Fig.1A-B).
Compared to those who reported sleeping well and were highly active(≥30.0 MET-h/week),use of sleeping medication,difficulty falling asleep,and easily awakened were associated with a 33.3%-53.5%,23.3%-33.8%,and 14.0%-23.5%,respectively increased risk of all-cause mortality among the 2 or 3 lowest PA groups(<15.0 or<30.0 METh/week)(Fig.2A,Supplementary Table 3 for numerical results).A similar pattern was found with CVD mortality,with the exception of difficulty falling asleep at the 7.5-14.9 PA level,which had a marginally statistically significant association(HR=1.335,95%CI:0.983-1.812,p=0.064)(Fig.2B).However,these detrimental associations with all-cause and CVD mortality were not present among participants who achieved at least 30.0 MET-h/week of PA.Those who slept well but did not achieve the recommended amount of PA (<7.5 MET-h/week)also had an increased risk of all-cause mortality(HR=1.239,95%CI:1.131-1.357)and CVD mortality(HR=1.457,95%CI:1.165-1.821)compared to the reference group
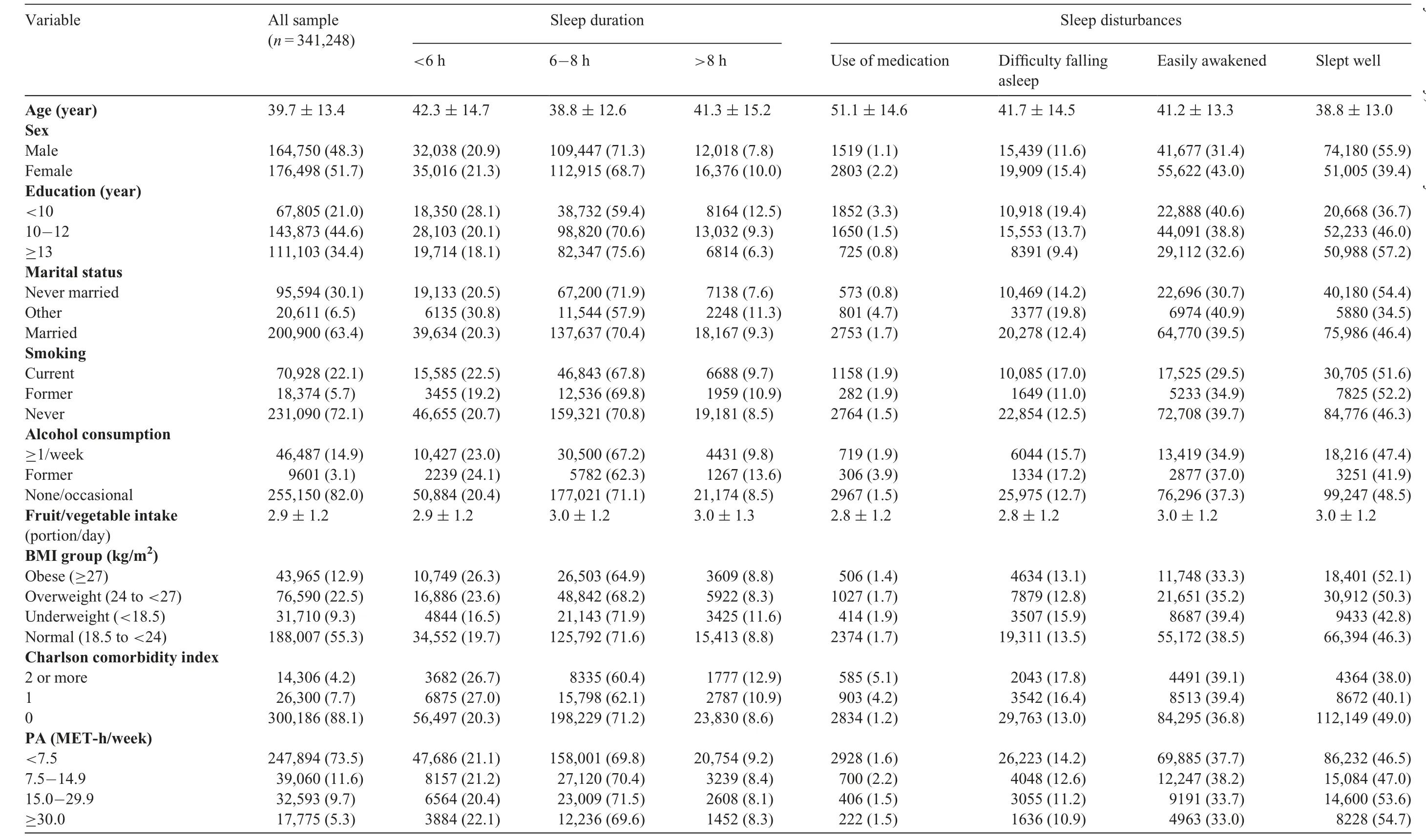
Table 1Characteristics of participants by sleep duration and sleep disturbances(n(%)or mean±SD).
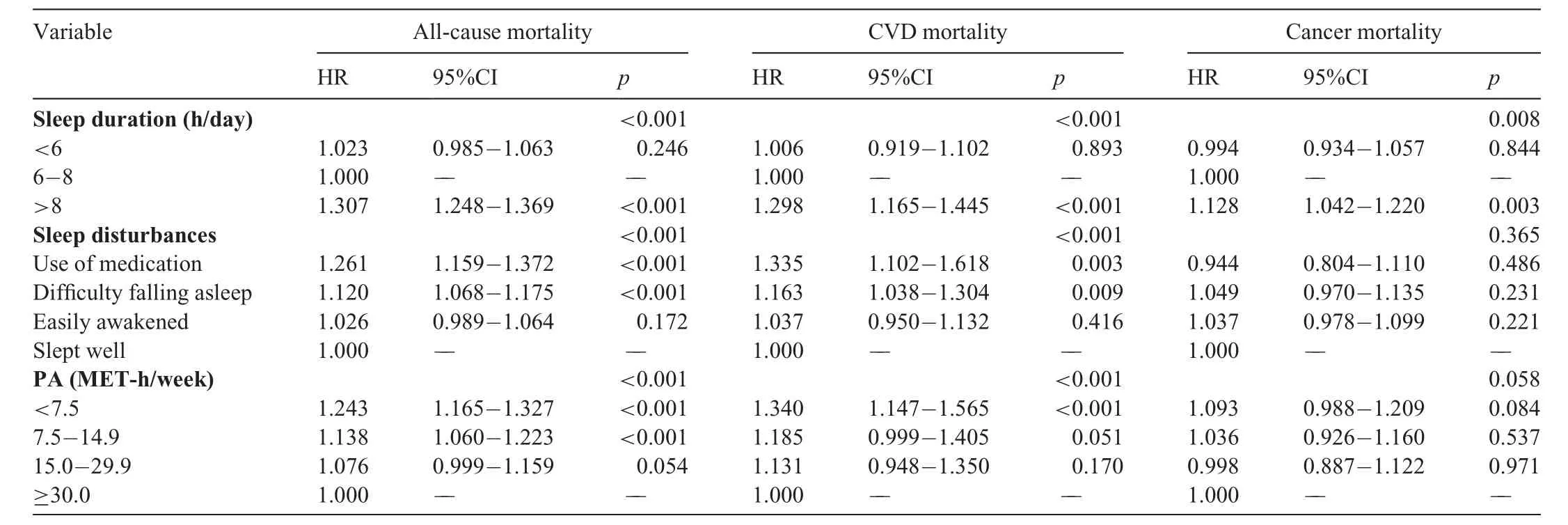
Table 2Risk of all-cause,CVD,and cancer mortality by sleep patterns and PA.
No increased risk of cancer mortality was found with sleep duration or disturbances in combination with PA levels,with the exception of the group with the lowest PA level(<7.5 MET-h/week)and highest sleep level(>8 h/day),where a 15.3% increased risk was found(HR=1.153,95%CI:1.009-1.318)(Fig.1C and Fig.2C).
We also examined an alternative combination of sleep patterns and PA by grouping PA into 3 levels(<7.5 MET-h/week,7.5-14.9 MET-h/week,and≥15.0 MET-h/week).When PA was divided into 3 levels,the attenuation of the association of poor sleep patterns with all-cause and CVD mortality were less apparent(Supplementary Table 4).Results from the sensitivity analyses excluding participants who were obese or used psychiatric medications showed a similar pattern,with high PA(≥30 MET-h/week)eliminating the increased risk of all-cause mortality associated with sleep duration and the increased risk of CVD mortality associated with sleep disturbances(Supplementary Table 5).The detrimental association of sleep disturbance with all-cause mortality were not present among participants who achieved 15.0 MET-h/week of PA.The same applied to participants who achieved the recommended amount of PA(7.5 MET-h/week).Participants had no increased risk of CVD mortality among each sleep duration group.
4.Discussion
This is the first investigation,to our knowledge,examining the joint effects of sleep patterns and PA with all-cause,CVD,and cancer mortality.Previous research examining these associations tended to focus on sleep duration.39,40Long sleep duration,difficulty falling asleep,and use of sleeping medication were all related to a higher risk of death,independent of a wide range of potential confounders.Our results consistently indicated that higher levels of PA appeared to attenuate or even eliminate the detrimental association between poor sleep patterns and increased all-cause and CVD mortality risk.Specifically,amounts of PA≥15.0 MET-h/week(and,in particular,≥30.0 MET-h/week),long sleep duration,use of sleeping medication,and difficulty falling asleep were no longer associated with all-cause and CVD mortality risk.
Our study found a 13%-31%increase in all-cause,CVD,and cancer mortality risk among long duration sleepers,whereas there was no significant increase in mortality risk among short duration sleepers.Our results support previous meta-analyses showing that long sleep duration was associated with an increased risk of allcause,CVD,and cancer mortality.5-7,41,42Some earlier meta-analyses have reported a significant association between short sleep duration and increased risk of all-cause or CVD mortality,5-8while others have not found such an association.42,43A greater increase in risk of death was observed among those with long sleep duration than with short sleep duration,which is consistent with recent systematic reviews.42,43There are some explanations for the detrimental association of long sleep duration with mortality.40,44-47First,mortality risk associated with(self-reported)long sleep duration might be partly attributable to spending a long time in bed as a compensatory behavior for increased sleep fragmentation.Second,long periods of time spent in the dark could have physiological effects,such as short photoperiods and photoperiodic abnormalities,both of which have been associated with mortality.Third,health issues,such as sleep apnea,depression,and frailty(e.g.,low PA levels,very slow walking speeds),might partly explain the relationship between long sleep duration and mortality.Additionally,feelings of lethargy and malaise noted in long duration sleepers could indicate a cytokine imbalance,which can impair resistance to stress and disease.Therefore,it is possible that the association between long sleep duration and mortality may simply be the result of reverse causality or residual confounding.40
In our study,short sleep duration was associated with allcause mortality in the 2 least active groups and was associated with CVD mortality in the least active group.This finding was not present in the full-sample analyses.Our results are novel in that they indicate that the deleterious effect of short sleep duration on mortality may be conditional on other lifestyle health behaviors.For example,the 45 and up study examined a lifestyle risk index and multiple behavioral risk combinations,including physical inactivity,sedentary behavior,and sleep duration,in relation to all-cause mortality among Australian adults aged 45 years or older.The results showed that when sleep alone was analyzed,short sleep duration was only marginally associated with all-cause mortality(HR=1.09,95%CI:1.00-1.18).However,the combination of short sleep duration and physical inactivity was more strongly associated with allcause mortality(HR=1.60,95%CI:1.45-1.78).40
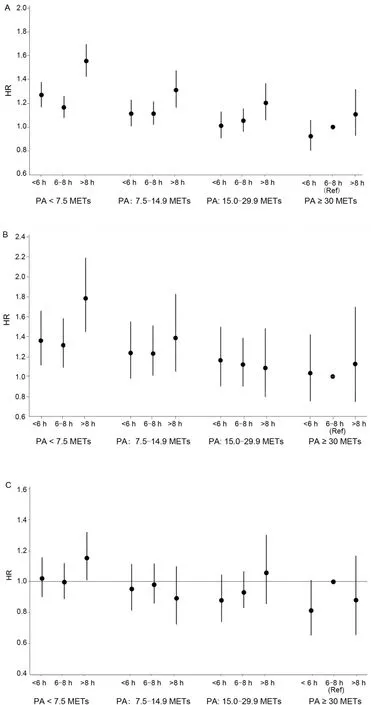
Fig.1.Joint association of sleep duration and PA with(A)all-cause mortality;(B)CVD mortality;and(C)cancer mortality.CVD=cardiovascular disease;HR=hazard ratio;METs=metabolic equivalents;PA=physical activity.
Our study also found that increased risk of all-cause and CVD mortality was related to difficulties in falling asleep but not to the condition of being easily awakened,which is consistent with the recent systematic review conducted by Ge et al.9This result indicates that a delay in falling asleep is associated with a greater mortality risk when compared to sleep maintenance.In our study,the use of sleeping medications was associated with a 26% increase in risk for all-cause mortality and a 34% increase in risk for CVD mortality,which is similar to the results in a systematic review showing that users of hypnotic/anxiolytic medications had a 43% higher risk of allcause mortality.48Our data suggested that both quantity and quality of sleep are related to mortality risk,a result that has been noted in previous research.49The pattern in our study for the association between sleep disturbances and cancer mortality was somewhat weaker,which might be due to the lack of differentiation in site-specific cancer outcomes.
Our results related to the joint association of sleep disturbances and PA with mortality showed that all sleep disturbances were associated with an elevated mortality risk in the least active groups PA groups(<15.0 MET-h/week and<7.5 MET-h/week).More importantly,if individuals engaged in 50-65 min of moderate-intensity(4-5 METs)activity per day(≥30.0 MET-h/week),the increased risks of all-cause and CVD mortality associated with sleep disturbances were virtually eliminated.
When PA was divided into 3 levels,with the highest level set at≥15.0 MET-h/week,the attenuation of the association between poor sleep patterns with all-cause and CVD mortality was less apparent compared with the highest-level PA group(≥30.0 MET-h/week)of the 4-level categorization.These results suggest that the effects are largely driven by the highest levels of PA exceeding current guidelines.
Our data suggest that PA might alleviate the deleterious health consequences of poor sleep patterns.Inadequate sleep duration is associated with obesity,inflammation,and negative cardiovascular outcomes;50-52and sleep disturbances are risk factors for depression and dementia.53,54However,higher levels of PA are related to lower levels of depression,cognitive decline,obesity,and CVD.55-58The positive association between PA and health could potentially act as a mechanism,with PA decreasing the risk of mortality among individuals with poor sleep patterns.This might help explain why PA attenuates or eliminates the detrimental association of poor sleep patterns with mortality.
Our analyses adjusted for a wide range of sociodemographic and behavioral factors,as well as physical health status,with a large sample size and a long follow-up period.However,our study has some limitations.First,participants were relatively young and tended to have a slightly higher socioeconomic status than the general adult population.However,this lack of representativeness is highly unlikely to have influenced the associations we examined.59Second,our data are observational,and we cannot rule out the possibility of unmeasured confounding.Moreover,PA and sleep data were self-reported,which may have introduced recall bias.However,previous research suggests good agreement between sleep self-reports and polysomnography.60It is also notable that some of the CIs are wide.This may have been due to the small sample size in specific groups(e.g.,the group of medication use with PA≥30.0 MET-h/week).
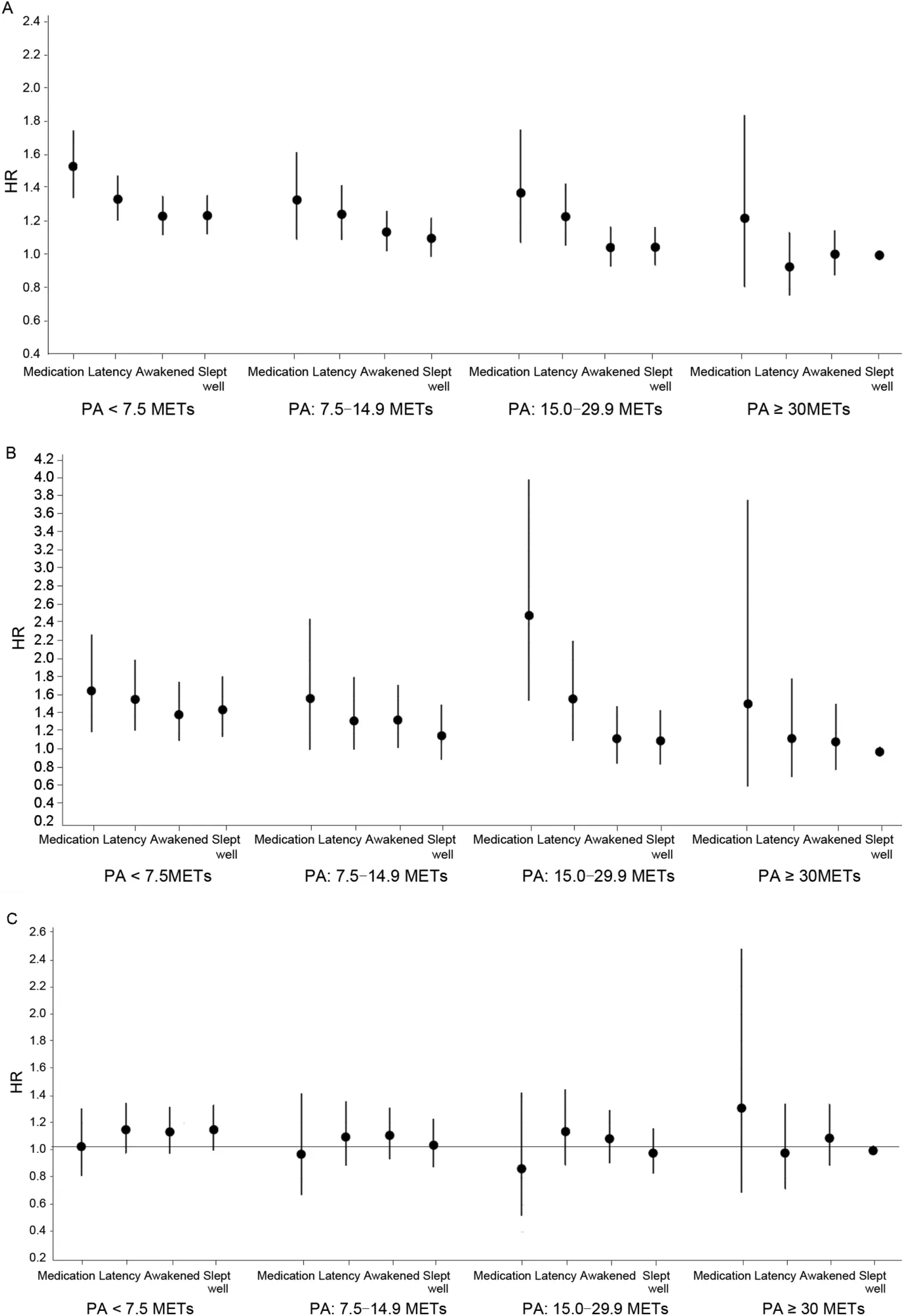
Fig.2.Joint association of sleep disturbances and PA with(A)all-cause mortality;(B)CVD mortality;and(C)cancer mortality.CVD=cardiovascular disease;HR=hazard ratio;METs=metabolic equivalents;PA=physical activity.
5.Conclusion
Long sleep duration(>8 h/day)and sleep disturbances,such as difficulty falling asleep and use of sleeping medication,were related to a higher risk of all-cause and CVD death among the entire sample.Being physically active(engaging in 25-65 min of moderateintensity activity per day)attenuated or eliminated the deleterious association of poor sleep patterns with mortality risk.Our results suggest that the mortality risks from short sleep duration,long sleep duration,or sleep disturbances are exacerbated by physical inactivity.These findings support the integration of PA into clinical sleep interventions and public health guidelines.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
All of the data used in this research were authorized for use by the MJ Health Resource Center(Authorization code:MJHRF2019013A)and by the Health and Welfare Data Science Center,Ministry of Health and Welfare.Any interpretations or conclusions described in this paper do not represent the views of the MJ Health Resource Center.
Authors’contributions
LJC contributed to the conceptualization,data analysis,and writing(original draft);MH contributed to the conceptualization,data interpretation,and writing(review and editing);YJL and BHH contributed to the conceptualization,and writing(review and editing);PWK contributed to the funding acquisition,conceptualization,data analysis,and writing(original draft);ES contributed to the funding acquisition,conceptualization,data interpretation,and writing(review and editing).All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Financial disclosure
PWK’s work is supported in part by the Ministry of Science and Technology(MOST 108-2410-H-018-028-MY3).ES is funded by the National Health and Medical Research Council(NHMRC)through a Senior Research Fellowship.The sponsors had no role in the study design,data collection,data analysis,data interpretation,or the writing of the report.
Supplementary materials
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2021.03.001.
 Journal of Sport and Health Science2022年5期
Journal of Sport and Health Science2022年5期
- Journal of Sport and Health Science的其它文章
- Risk management strategies for the 2022 Olympic Winter Games:The Beijing scheme
- Risk of bias and reporting practices in studies comparing VO2max responses to sprint interval vs.continuous training:A systematic review and meta-analysis
- Effectiveness of statins vs.exercise on reducing postprandial hypertriglyceridemia in dyslipidemic population:A systematic review and network meta-analysis
- Association of accelerometer-derived step volume and intensity with hospitalizations and mortality in older adults:A prospective cohort study
- Number of parous events affects the association between physical exercise and glycemic control among women with gestational diabetes mellitus:A prospective cohort study
- Cardiorespiratory fitness,white blood cell count,and mortality in men and women
